Network Analysis of Foramen Ovale Electrode Recordings in Drug-resistant Temporal Lobe Epilepsy Patients
In This Article
Summary
This protocol describes a procedure to track the evolution of mesial network measures in temporal lobe epilepsy (TLE) patients. It is based on the combination of intracranial recordings with a novel numerical technique for data analysis. Specifically, we present a protocol for network analyses of foramen ovale recordings.
Abstract
Approximately 30% of epilepsy patients are refractory to antiepileptic drugs. In these cases, surgery is the only alternative to eliminate/control seizures. However, a significant minority of patients continues to exhibit post-operative seizures, even in those cases in which the suspected source of seizures has been correctly localized and resected. The protocol presented here combines a clinical procedure routinely employed during the pre-operative evaluation of temporal lobe epilepsy (TLE) patients with a novel technique for network analysis. The method allows for the evaluation of the temporal evolution of mesial network parameters. The bilateral insertion of foramen ovale electrodes (FOE) into the ambient cistern simultaneously records electrocortical activity at several mesial areas in the temporal lobe. Furthermore, network methodology applied to the recorded time series tracks the temporal evolution of the mesial networks both interictally and during the seizures. In this way, the presented protocol offers a unique way to visualize and quantify measures that considers the relationships between several mesial areas instead of a single area.
Introduction
Epilepsy is a disabling disease that affects 1 - 2% of the world's population. In the majority of cases, seizures — the hallmarks of epilepsy — can be completely controlled or abolished with anti-epileptic drugs. However, approximately 30% of epilepsy patents are refractory to drug therapies. In the most common type of epilepsy, the temporal lobe epilepsy (TLE)1, fortunately surgery is a valid alternative to improve the patient's condition. Results from meta-analyses show that almost two thirds of drug-resistant TLE patients are seizure-free in the first two to three years after the resective surgery2,3, although this proportion varies across several factors, most notably, the type of hippocampal sclerosis2. A critical step for a successful outcome is the accurate localization of the so-called epileptic focus, the cortical area responsible for the generation of seizures, which is typically located in the mesial area of the temporal lobe. However, even in those cases where the epileptic focus has been correctly identified and resected during the surgery, a significant minority of patients either remains with post-operative seizures or must be placed under strict antiepileptic drug treatment to control seizures. Therefore, a new perspective has emerged in which attention is no longer focused solely on isolated areas, instead cortical interactions now constitute the fundamental issue. This "network" approach is grounded in the connectome concept4, which focuses attention in the neural connections between different areas rather than highlighting the role of compartmentalized structures. This new paradigm was found in graph theory, a mathematical framework devoted to the study of topological and statistical properties of graphs, the appropriate tool to express its fundamental findings. Under this perspective, the brain is considered as a set of nodes interconnected by links5-9 such that nodes are represented by the cortical areas covered by the electrodes and the links between them are given by the degree of synchronization. Thus, this network approach has been used in the analysis of invasive electrode recordings and has provided new information to promote the understanding of the underlying mechanism of seizure generation and propagation.
Among the many invasive neurophysiological techniques routinely employed in most epilepsy centers around the world, the foramen ovale electrode (FOE) is particularly remarkable. FOE is a semi-invasive technique because there is no need to perform a craniotomy, which reduces surgery-related complications10. Additionally, the location of FOE in the ambient cistern11 makes them especially convenient for recording mesial activity from several cortical structures involved in seizure generation and propagation, such as the entorhinal cortex. Therefore, its use since its appearance is widespread in the presurgical evaluation of drug-resistant TLE patients. Traditionally, this technique is used to locate irritative activity in the form of interictal epileptogenic spikes and sharp-waves, and more importantly, to accurately identify the area of mesial seizure onset.
The new definition proposed from the Commission on Classification and Terminology from the International League against Epilepsy (ILAE) suggests that seizures originate at some point within particular networks12. Moreover, several studies have demonstrated that seizures are caused by abnormal network activity rather than by an isolated pathological area13-16. Clearly, this new perspective requires reanalysis of previously acquired information using new numerical methods, such as complex network methodology. Although the practical use of these analyses is still incipient in clinical practice, several research studies have demonstrated their value13-17.
The protocol described below is the combination of a clinical practice routinely performed on drug-resistant TLE epilepsy patients with a novel technique of network analysis. The method allows for the evaluation of the temporal evolution of mesial network parameters. The bilateral insertion of FOE into the ambient cistern simultaneously records the electrocortical activity at several mesial areas of the temporal lobes. A network approach applied to the recording time series tracks the temporal evolution of the mesial networks both interictally and during the seizures. In this way, the presented protocol offers a unique way to visualize and quantify measures that considers the relationships between several mesial areas.
Protocol
In the protocol described below, steps 1, 2 and 3 belong to both the research and clinical protocols, which are both strictly followed from every mesial TLE candidate for resection surgery selected only by clinical criteria. Steps 4 and 5 belong exclusively to the research protocol. Both procedures are in accordance with the guidelines of the Ethical Committee of the Hospital de la Princesa.
1. Pre-implantation Procedures
- Explain the experimental procedures to the participant, specifying which points correspond to the research and which ones are applicable to clinical practice, remarking that the research procedure is in no way modifying the clinical procedure. Pay special attention to explaining the potential risks of the surgical implantation of electrodes. Obtain a signed informed consent form the participant.
- For all candidates for resection surgery, perform presurgical neurological and neuropsychological examinations18.
- Evaluate the patient by interictal single photon emission computer tomography (SPECT) with 99Tc-HmPAO, magnetic resonance imaging (MRI) 1.5 T and video-electroencephalography (v-EEG) using 25 scalp electrodes according to the 10 - 20 international system and Maudsley's protocol18.
- During the presurgical v-EEG recording stay, progressively taper the antiepileptic drugs from the second day to the fourth day (approximately one-third of the dose per day).
2. Implantation Procedures (Surgery)
- Administer antiepileptic drugs pre-operatively, and perform surgery under general anesthesia (3 mg/kg propofol bolus, followed by 0.2 - 0.3 mg/kg fentanyl and 0.5 mg/kg rocuronium).
- Insert two six-contact FOEs with a 1-cm center-to-center distance bilaterally into the ambient cisterns using Kirschner's technique19.
- Place the patient on the operating table in the supine position, with the neck gently extended at 15 degrees. Prepare the patient's cheek with an iodine solution, starting at the incision site and circling outward, and drape the area immediately surrounding the incision site.
- Puncture the skin with a 20-gauge spinal needle according to Hartel's landmarks20: an entry point approximately 3 cm lateral to the ipsilateral side of the oral commissure toward a point immediately inferior to the ipsilateral pupil in the anterior-posterior plane and a point approximately 2.5 cm anterior to the external auditory meatus in the lateral plane.
- Advance the needle toward the region of the foramen ovale under fluoroscopic guidance. Use the lateral views provided by the fluoroscopy images to determine the position of the needle tip. When the needle passes the foramen ovale, remove the stylet, replace it with an electrode, and advance it into the ambient cistern (Figure 1A).
- Assess correct implantation by fluoroscopic imaging in the operating room21; this is important to exclude penetration into the foramina of the skull base, such as the inferior orbital fissure (located anterior to the foramen ovale) and the jugular foramen (located posterior to it). Such misplaced cannulation could potentially lead to serious neurovascular injury22.
- Once the electrodes are correctly positioned in the ambient cisterns, secure them to the skin with drapes. Wake up the patient, and lead him or her to the recovery room.
3. Acquisition of FOE Recordings
- Return the patient to the v-EEG room for a stay of approximately 5.2 ± 2.4 days (mean ± SD).
- Place 19 electrodes according to the international 10-20 system.
- Measure the distance between the nasion (bridge of the nose) and the inion (occipital protuberance) using a measuring tape, and mark with a marker the middle point (location of the Cz electrode). Measure and mark the point 10% of the distance above the nasion (location of the Fpz electrode).
- Repeat the same procedure for the inion (location of the Oz electrode), marking the distances 20% from the Cz in both the nasion and inion directions (locations of the Fz and PZ electrodes, respectively).
- Measure the distances between both preauricular points, and mark the distances 10% above the left and right preauricular points (T3 and T4 electrodes, respectively). Then, mark the distances 20% above both T3 and T4 in the Cz direction to obtain the locations of C3 and C4.
- Create a circumference using the measuring tape to link the Fpz and Oz at 5% of the distances above both electrodes at FP1 (left) and FP2 (right) in the front and at O1 (left) and O2 (right) in the back.
- In the same circumference, add 10% of the distance upward in the inion direction to obtain the position of F7, add 10% to reach T3 (it should be located above the line between the preauricular points), and add another 10% to obtain T5 (O1 electrode). Mark each electrode position and repeat the same procedure for the right (even) electrodes.
- Measure and mark the intersection (F3 electrode location) halfway between F7 and Fz and 20% of the distance upward from Fp1 in the F3 direction. Repeat this process in each quadrant of the head to obtain F4 (front-right position), P3 (back-left position) and P4 (back-left position).
- Clean and dry the skin. Place a moderate quantity of collodion with conductive gel in each electrode cup, and position the electrodes in the prepped areas. Dry the collodion with a hair dryer.
- Measure the distance between the nasion (bridge of the nose) and the inion (occipital protuberance) using a measuring tape, and mark with a marker the middle point (location of the Cz electrode). Measure and mark the point 10% of the distance above the nasion (location of the Fpz electrode).
- Connect all of the electrodes (scalp and FOEs) by wires to the electrode box, which is already connected to an electroencephalographer. Ensure that the electrode signals are good, and verify that the scalp electrodes impedances are under 10 kΩ using the electroencephalographer.
- Acquire digital scalp electroencephalogram (EEG) data and FOE data at 1,024 Hz using a video synchronized electroencephalographer (v-EEG), and filter the data using a band-pass filter in the range 0.5 - 100 Hz and a Notch filter (50 Hz) with the electroencephalographer.
- Progressively remove the antiepileptic drugs from the second to the fourth day (approximately one-third of the dose per day) to increase the likelihood of seizures. This step depends on the particular drug prescription of each patient.
- Use both interictal paroxysmal and ictal activities to approximately locate the ictogenic areas by identifying the electrodes/channel where epileptogenic elements appear23, including the slow-wave complex, polyspikes, runs of rapid spikes, sharp waves, sharp-and-slow-wave complex, slow sharp waves, spikes and spike and slow waves. Record the times of seizure onset and end, as well as any other clinical signs or occurrences relevant to the study. There is a one-to-one mapping between the electrodes location in the patient's head and the head model in the EEG software which allows identifying anatomically where the epileptogenic activity appears.
- When the study is finished, remove the FOEs at the v-EEG unit by gently pulling them out while the patient's mouth remains half-opened. Do not systematically perform imaging after FOE removal, except when neurological symptoms appear. In such cases, perform an urgent computed tomography (CT) scan.
4. FOE Signal Preprocessing
- Export the data stored on the electroencephalographer at 200 Hz in ASCII format in epochs suitable for numerical analysis of approximately 30 min of seizure activity (already identified by an expert neurophysiologist) (Figure 1C). Avoid epochs containing artifacts, such as saturated electrical activity, muscle activity, and electrode displacements.
- Open the exported files using any UNIX stream editor, and remove all non-numerical characters from the exported data files, leaving only time stamps and channel voltages. Save the modified files for further numerical analysis.
NOTE: From now on, perform all calculations using R packages from the R repository or homemade codes (Table 1). - Using R software, install the required R packages, and load the modified data files into the R environment. Order all channels, assigning each one to a particular column of the array that contains all of the data, eliminating empty channels and referencing them to an average mid-line reference (Fz + Cz + Pz)/3.
- Use the Fast Fourier Transform algorithm (R function: fft) and plot the resulting variable to check for the effective removal of the line frequency (approximately 50 Hz). Use the frequency domain to filter other spurious frequencies that may contaminate the signals.
- Convert the loaded data to a multivariate time-series object (mts) of 28 columns — 16 scalp and 12 FOEs — using the R function ts. Divide the mts object into non-overlapping temporal windows of 5 seconds each (1,000 data points at 200 Hz) to reduce the file size and optimize computation time.
5. Post-processing Calculations (Complex Network Analysis)
NOTE: Calculate the measures described below in each temporal window, starting at 5 min before seizure onset (60 windows) and ending at 5 minutes after seizure onset (60 windows), with the aim of visualizing the temporal evolution.
- Calculate univariate measures, spectral power, excitability and spectral entropy for each individual column/channel without considering the correlations between different time series.
- Calculate excitability (S) for each voltage activity time series using a homemade code according to the equation proposed by Schindler24 (see supplemental file). S > 2.5 is considered epileptogenic, an empirically determined threshold17,25,26.
- For each activity time series, calculate the power spectral density using a homemade code for the Delta (>0.5 Hz and <4 Hz), Theta (4 - 7 Hz), Alpha (7 - 14 Hz), Beta (14 - 30 Hz) and Gamma (>30).
- Calculate Shannon entropy with a homemade code using the power spectral density of each time series instead of the corresponding probability time series. Average the individual spectral entropy (SE) values obtained for each channel over a set of electrodes. Shannon entropy is explained in the supplemental file.
NOTE: A decrease in SE should be interpreted as a decrease in the number of frequencies of the spectrum because SE is the entropy of the spectrum.
- Network measures
NOTE: This section assesses the interactions between different time series of electrodes.- Calculate the functional connectivity between each pair of voltage time series in each temporal window using the absolute value of the linear cross-correlation coefficient computed at zero lag (R function: ccf).
NOTE:To eliminate non-representative values of synchronization, establish a threshold based on previous studies17,25,26. Use a threshold of 0.5 in this particular case. - Install the igraph R package27. Create an igraph object from the adjacency matrix (R function: graph.adjacency). Use the correlation matrix obtained in the previous step, specifying that the graph is weighted and undirected.
- In each temporal window calculate the average path length (APL) (R function average.path.length) for the entire network (scalp+FOE), and for each of the four sub-networks: left scalp, right scalp, left FOE and right FOE. In exactly the same way, calculate the density of links (DoL) (R function: graph.density), modularity (Mod) (R function: modularity) and the Average clustering coefficient (ACC) (R function: transitivity).
- Repeat the previous steps 5.2.1 through 5.2.3 using phase synchronization (homemade R code) as an estimate of functional connectivity instead of the cross-correlation function.
- Calculate the functional connectivity between each pair of voltage time series in each temporal window using the absolute value of the linear cross-correlation coefficient computed at zero lag (R function: ccf).
- To represent the size effects in the variable changes, calculate the standardized mean difference (SMD) (R function from package MBESS: smd), between the preictal and the ictal stages as well as between the preictal and postictal stages.
- Taking the preictal as the baseline, select thirty seconds (6 values) five minutes before seizure onset mark, as the preictal value. A similar temporal window of 30 s can be chosen during the seizure in order to quantify the change, respect to the preictal stage, by using the SMD.
- In a similar fashion, 5 min after seizure ends, select a temporal window of 30 s in order to quantify the change during the postictal stage (in respect to the preictal stage).
Representative Results
The final position of the FOE is in the ambient cistern, as seen in the axial and sagittal MRI (Figure 1A upper panels). The contacts of the FOE record electrical activity from several mesial structures of the temporal lobe (Figure 1A lower panel). After the surgery (Figure 1B left panel), the patient is dispatched to the video-EEG room, where scalp electrodes are placed according with the 10 - 20 system (Figure 1B right). During the stay at the video-EEG room, the patient is continuously monitored, saving for further analysis scalp and FOE recordings, as well video and vital constants. A typical raw scalp and FOE signals (Figure 1C) show the appearance of a seizure at the left FOE and its spread to scalp and right FOE contacts.
Representation of the epileptogenic activity by using the excitability (S) (Figure 2) corresponding to the raw EEG recordings from Figure 1C, during the transition from the preictal to the ictal and postictal periods. Seizure onset is marked with a solid vertical line and time (x-axis) are referred to this point. A value of S (excitability) >2.5 represented irritative or epileptogenic activity17,25,26. Higher excitability (reddish colors) appeared firstly with higher intensity on the left FOE contacts (LFOE). This result is concordant with a left mesial temporal lobe epilepsy as informed by an expert neurophysiologist.
Temporal dynamics of several network measures as well as the spectral entropy (Figure 3) during the transition from the preictal to the ictal and postictal stages, corresponding to the same seizure displayed in Figure 1C and 2. Seizure onset is marked with a solid vertical line and time (x-axis) are referred to this point. In this case, the network was built upon the whole set of electrodes, including both scalp and FOE. DoL and ACC values were higher during seizures, with a decrease in the APL and Mod, suggesting an increase in the overall connectivity. During this period also, lower levels of SE were observed and sustained after the excitability (dotted vertical lines) disappears.
The analysis of the network measures ACC, DoLs and APL and the SE for each FOE (right and left) (Figure 4) during the transition from the preictal to the ictal and postictal stages. Seizure onset is marked with a solid vertical line and time (x-axis) are referred to this point. The evolution of this measures correspond to the same seizure of Figures 1, 2 and 3. The ipsilateral (left) mesial ACC, DoLs and APL presented earlier and higher changes than the contralateral values, which could be explained by the location of the seizure onset zone in the left temporal lobe. In this case, Mod could not be calculated because no subdivisions were available.
A representative video of the functional connectivity (Figure 5) during the same seizure of Figure 1, 2, 3, and 4 presents a critical change just after the seizure onset (Time 0). At that point the connectivity between all the electrodes increase dramatically, as can be seen by an increase of the number of links and the thickness (intensity) of that edges. This increase starts between the left FOE at time 0.1 and 0.2, and spreads to the contralateral side before reaching the whole network.
| fft | 4.3 | (stats package) Computes the Fast Fourier Transform of a signal. |
| ts | 4.4 | (stats package) Creates a multivariate time-series object (mts). The sampling frequency should be provided. |
| Excitability | 5.1.1 | (homemade) function based on diff R function. Computes the absolute value of the slope of the signal and then normalize it to the standard deviation short baseline period. Threshold should be provided. |
| Power spectral Density and Spectral Entropy | 5.1.2 | (Homemade) function based on spectrum and entropy R functions. Compute the normalized power spectrum and the Shannon entropy of the normalized power spectrum |
| ccf | 5.2.1 | (base package) calculates the linear cross-correlation of mts object by using Pearson correlation at zero lag, generating a correlation matrix. Absolute values should be calculated. |
| graph.adjacency | 5.2.2 | (igraph package) Creates an igraph graph, the basic object used by the following igraph functions |
| average.path.length | 5.2.3 | (igraph package) determines the average path length of the graph, by computing the average number of steps along the shortest paths through all of the network nodes. |
| graph.density | 5.2.3 | (igraph package) Computes the density of links of the graph by computing the ratio between the actual number of links and all possible links of the network. |
| modularity | 5.2.3 | (igraph package) Determines the modularity of the graph, by computing which groups of nodes are more connected between them than with other nodes of the network |
| transitivity | 5.2.3 | (igraph package) Determines the average clustering coefficient of the graph, by computing the proportion of neighboring nodes that are also neighbors of one another |
| Phase synchronization | 5.2.4 | (homemade) function based in fft R function that calculates the mean phase coherence to obtain values between zero and one |
| smd | 5.3 | (MBESS package) Determines the standard mean difference -size effects- by computing the difference in mean between groups relative to the pooled difference |
Table 1: R functions Used for Data Processing.
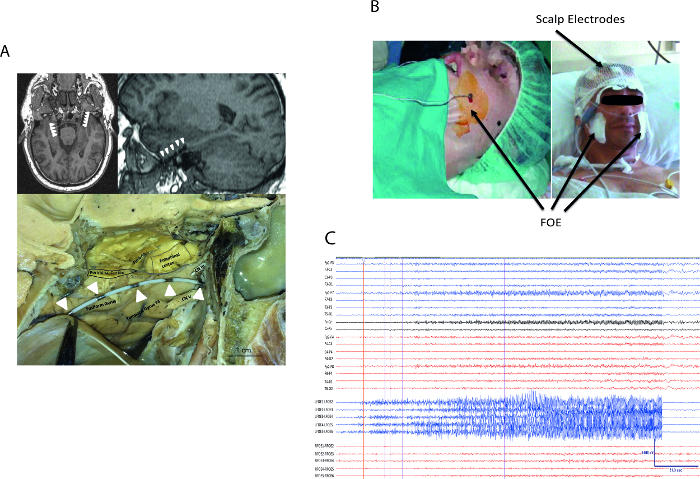
Figure 1: Foramen Ovale Electrodes. (A) Final position of FOE into the ambient cistern. Upper panels show an axial (left) and sagittal (right) MRI images displaying the FOE contacts location (white arrows). A human specimen (cadaver) with an inserted FOE (lower panel, contacts marked with white arrows). (B) FOE and scalp electrodes setup. Patients head just after the FOE insertion surgery (left panel) and during the video-EEG stay (right panel). (C) FOE and scalp recordings. Complex partial seizure from a left TLE patient (5 min after and before seizure onset). RFOE1-RFOE6 stands for right FOE#1 to #6 and LFOE1-LFOE6 stands for left FOE#1 to #6. Seizure onset is marked by a vertical red line and a white arrow head. Please click here to view a larger version of this figure.
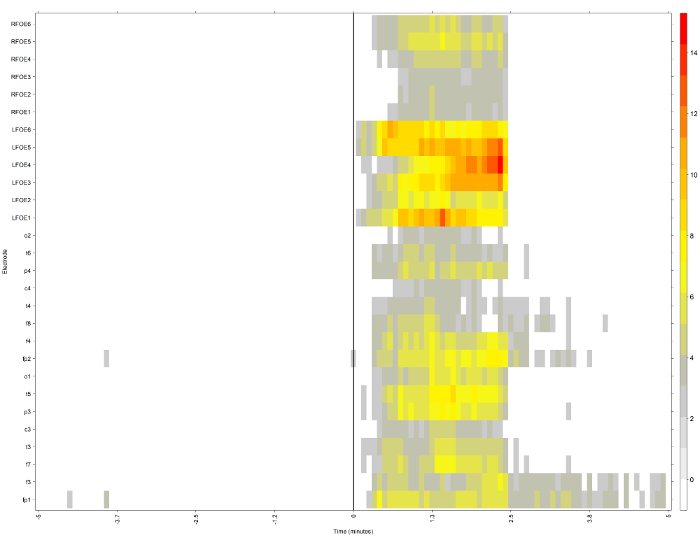
Figure 2: Representation of a Complex Partial Seizure from a Left TLE Patient Quantified by Excitability. The color scale quantifies the excitability level (S) for each electrode. The right foramen ovale electrode (RFOE) and left foramen ovale electrode (LFOE) represent the contacts of the right and left foramen ovale electrodes (y-axis), respectively. The x-axis marks the time (in min) relative to seizure onset (thick vertical line) as determined by an expert neurophysiologist. Please click here to view a larger version of this figure.
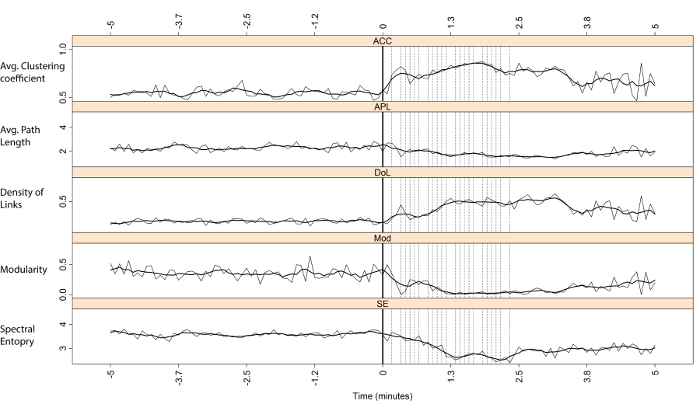
Figure 3: Entire Network (scalp+FOE) Measures from the Same Patient and Same Seizure from Figure 2. The average clustering coefficient (ACC), average path length (APL), density of links (DoLs), modularity (Mod) and spectral entropy (SE) for the entire network (scalp + FOE) are represented. The vertical dotted lines represent the excitability (S). The x-axis marks the time relative to seizure onset (thick vertical solid line). A moving average over ten consecutive windows is represented by a thick solid black line. Please click here to view a larger version of this figure.
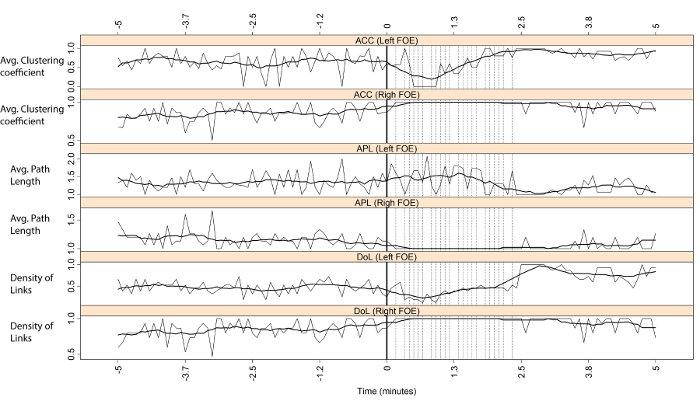
Figure 4: Mesial Measures of the Same Patient from Figure 2 and 3. The average clustering coefficient (ACC), average path length (APL), density of links (DoLs) and spectral entropy (SE) for both the left and the right foramen ovale electrodes (FOEs). The vertical dotted lines mark the excitability. The x-axis marks the time relative to seizure onset (thick vertical solid line). A moving average over ten consecutive windows is represented by a thick solid black line. Please click here to view a larger version of this figure.
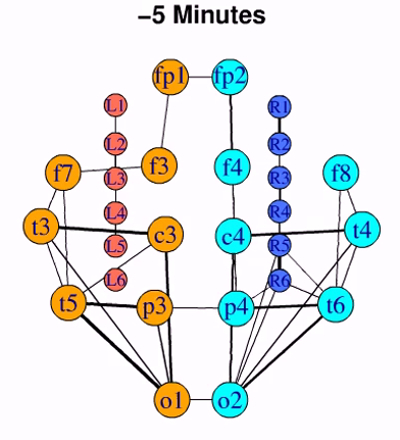
Figure 5: Dynamic of Connectivity Pattern during a Complex Partial Seizure. Links intensity is represented by the thickness of the edges. Times (lower numbers) are relative to the seizure onset (Time 0). Each frame is 5 sec long. Left and right foramen ovale electrodes (L1-L6 and R1-R6) are represented by coral and blue circles, respectively. Left and right scalp electrodes are represented by orange and cyan circles, respectively. Please click here to download this movie.
Discussion
Traditionally, epilepsy was studied under a zone-oriented approach, which isolated the importance of particular areas, essentially the seizure onset zone, as the unique cause of seizures. Very recently, a true network approach that emphasizes the importance of interactions between cortical areas has been favored over the classical zone-oriented perspective13-17,28. However, the current body of evidence for epilepsy as a network disease is still highly fragmented, and more research is needed. The present work aims to reanalyze data provided by traditional methods as the FOE, under the complex network approach. The protocol presented here describes a step by step methodological procedure to perform a complex network and spectral analysis of semi-invasive recordings in TLE patients.
The application of the technique described above has demonstrated the usefulness of the network approach as compared with the more traditional localized or zone-oriented perspectives. In recent works17,29 it was shown that, using the very same procedure as the one described here, an imbalance in the mesial connectivity in refractory TLE patients is apparent. Mesial connectivity is reduced in the ipsilateral side both during the interictal29 and ictal17,29 stages. This result could not be anticipated by looking solely at the areas where the epileptogenic activity arises. This somehow surprising result was also described by using network theories on fMRI signals30,31. Moreover, the application of the combined technique of FOE+network theory has shown the equivalence of mesial activity during seizures and under the effects of a promoter of epileptogenic activity, as it is the pharmacological administration of etomidate32.
The technique described here is capable of detecting mesial network imbalance in short interictal recordings lasting at most one or two hours29. In this way, a drastic reduction in the analysis time and patient hospital stay could be achieved. In addition, from a therapeutic perspective, the existing imbalance in TLE patients could be "resolved" by using chronically implanted (by neurosurgeons) devices, as much as the way it is done in deep brain stimulation.
To obtain optimal results using the information provided in this protocol, some issues should be considered in advance. First, the implantation of the electrodes should be performed by an experienced neurosurgeon because their incorrect placement could produce severe neurological consequences and misleading recordings. Furthermore, the selection of appropriate epochs for further analysis relies entirely on the neurophysiologist's interpretation of the raw EEG; therefore, experience in clinical EEG analysis is mandatory. The data format of the exported files from the electroencephalograph depends on the particular brand; consequently, good programming skills are needed to adapt the scripts to different data formats. Finally, to ensure the reliability of the data, quality controls should be applied to the results. Overestimation and false positives are likely to appear when working with a high number of correlations. In such cases, statistical methods to improve sensitivity should be used. In this regard, it is important to establish a threshold in the correlations to discard values that are not representative of a true underlying synchronization. Thus, in this protocol, an edge between nodes i and j will be only considered to exist if the absolute value of the correlation between these nodes is greater than 0.5, a criterion previously employed17,26. Other thresholds in the range of 0.2 to 0.8 should be employed to verify similar results and to ensure a smooth transition from one threshold to the following threshold. In addition to thresholds, other methodologies may be used to obtain reliable results, such as Bonferroni correction or surrogate data testing. Moreover, when working with EEG data, it is important to keep in mind that brain networks are complex systems with non-linear dynamics; therefore, in addition to the linear correlation, other non-linear synchronization measures should be used to ensure the quality of the results, such as mutual information or phase synchronization33.
Calculating connectivity directly from scalp electrodes, as it is partially done in this work, entails some risks. The main problem rest in the contamination effect due to volume conduction, always present with scalp recording. One way to overcome this issue is by working on the sources space, an appealing alternative employed by many researches. Another approach demands the use of measures of synchronization which minimizes the contamination of amplitude effects. By using the phase synchronization (also known as Phase Locking Value) we minimize the effect of volume conduction, as it was demonstrated in several works34.
As in other invasive neurophysiological techniques, recordings from FOE cannot be obtained from control subjects, a fact that severely limits the use of certain research protocols. Data from FOE recordings provide valuable information about mesial temporal lobe activity17,29,35, especially during lateralization to the epileptogenic side in TLE patients33. Compared with invasive techniques, the FOE technique is non-traumatic for the brain and involves relatively simple manipulation, and its recordings are of high quality over long periods of time11. Compared to MRI, FOE recordings provide better time resolution of electrocortical activity. In addition, many possibilities exist to explore measures other than those used in this work. These facts also increase the possibility of analyzing several biomedical recordings simultaneously. These advantages of FOE recordings combined with complex network and spectral analysis make this technique a powerful tool for epilepsy research with potential applications in clinical practice.
Acknowledgements
This work was funded by grants from Instituto de Salud Carlos III, through PI10/00160 and PI12/02839, partially supported by F.E.D.E.R and from Mutua Madrileña. A.S-G. is the recipient of a postdoctoral fellowship from Mutua Madrileña. 3D simulation were created using BioDigital Human software (www.biodigital.com) and ZygoteBody Professional software (www.zygotebody.com)
Materials
| Name | Company | Catalog Number | Comments |
| Foramen Ovale Electrodes | AD-Tech, Racine, USA | FO06K-SP10X-000 | Six-contact platinum |
| Electroencephalograph | XLTEK, Canada | XLT-EEG32T | Natus XLTEK |
| MRI machine | General Electric | ||
| SPEC machine | General Electric |
References
- Wiebe, S. Epidemiology of Temporal Lobe Epilepsy. Can J Neurol Sci. 27, 6-10 (2000).
- Thom, M., Mathern, G. W., Cross, J. H., Bertram, E. H. Mesial temporal lobe epilepsy: How do we improve surgical outcome. Ann Neurol. 68 (4), 424-434 (2010).
- Tellez-Zenteno, J. F., Dhar, R., Wiebe, S. Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain. 128 (5), 1188-1198 (2005).
- Sporns, O., Tononi, G., Kotter, R. The human connectome: a structural description of the human brain. PLoS Comput Biol. 1, 42 (2005).
- Fornito, A., Zalesky, A., Bullmore, E. . Fundamentals of Brain Network Analysis. , (2016).
- Wig, G. S., Schlaggar, B. L., Petersen, P. E. Concepts and principles in the analysis of brain networks. Ann. N.Y. Acad. Sci. 1224, 126-146 (2011).
- Rubinov, M., Sporns, O. Complex network measures of brain connectivity: uses and interpretations. Neuroimage. 52, 1059-1069 (2010).
- Boccaletti, S., Latora, V., Moreno, Y., Chavez, M., Hwang, D. -. U. Complex networks: Structure and dynamics. Phys Rep. 424, 175-308 (2006).
- Sporns, O., Chialvo, D. R., Kaiser, M., Hilgetag, C. C. Organization, development and function of complex brain networks. Trends Cogn Sci. 8 (9), 418-425 (2004).
- Pastor, J., Sola, R. G., Hernando-Requejo, V., Navarrete, E. G., Pulido, P. Morbidity associated with the use of foramen ovale electrodes. Epilepsia. 49 (3), 464-469 (2008).
- Wieser, H. G., Schwarz, U. Topography of foramen ovale electrodes by 3D image reconstruction. Clin Neurophysiol. 112 (11), 2053-2056 (2001).
- Berg, A. T., et al. Revised terminology and concepts for organization of seizures and epilepsies: Report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia. 51 (4), 676-685 (2010).
- Bertram, E. H., Xing-Zhang, D., Mangan, P., Fountain, N., Rempe, D. Functional anatomy of limbic epilepsy: a proposal for central synchronization of a diffusely hyperexcitable network. Epilepsy Res. 32, 194-205 (1998).
- Bartolomei, F., Wendling, F., Bellanger, J., Regis, J., Chauvel, P. Neural networks involved in temporal lobe seizures: a nonlinear regression analysis of SEEG signals interdependencies. Clin Neurophysiol. 112, 1746-1760 (2001).
- Spencer, S. S. Neural networks in human epilepsy: evidence of and implications for treatment. Epilepsia. 43, 219-227 (2002).
- Bartolomei, F., et al. Pre-ictal synchronicity in limbic networks of mesial temporal lobe epilepsy. Epilepsy Res. 61, 89-104 (2004).
- Vega-Zelaya, L., Pastor, J., de Sola, R. G., Ortega, G. J. Disrupted Ipsilateral Network Connectivity in Temporal Lobe Epilepsy. PLoS ONE. 10 (10), 0140859 (2015).
- Pastor, J., et al. Impact of experience on improving the surgical outcome in temporal lobe epilepsy. Rev Neurol. 41 (12), 709-716 (2005).
- Kirschner, M. Electrocoagulation des Ganglion Gasseri. Zentralbl Chir. 47, 2841-2843 (1932).
- Härtel, F. Über die intracranielle Injectionsbehandlung der Trigeminus neuralgie. Med Klin. 10, 582-584 (1914).
- Zampella, J. E., Brown, A. J., Azmi, H., Gandhi, D. C., Schulder, M. Percutaneous techniques for trigeminal Neuralgia. Handbook of Stereotactic and Functional Neurosurgery. , (2003).
- Franzini, A., Ferroli, P., Messina, G., Broggi, G., Nappi, G. Surgical treatment of cranial neuralgias. Handbook of Clinical Neurology. , (2010).
- Tatum, W. O., Husain, A. M., Benbadis, S. R., Kaplan, P. W. . Handbook of EEG interpretation. , (2008).
- Schindler, K., Leung, H., Elger, C. E., Lehnertz, K. Assessing seizure dynamics by analysing the correlation structure of multichannel intracranial EEG. Brain. 130 (1), 65-77 (2007).
- Bartolomei, F., Chauvel, P., Wendling, F. Epileptogenicity of brain structures in human temporal lobe epilepsy: a quantified study from intracerebral EEG. Brain. 131 (7), 1818-1830 (2008).
- Vega-Zelaya, L., Pastor, J. E., de Sola, R. G., Ortega, G. J. Inhomogeneous cortical synchronization and partial epileptic seizures. Front. Neurol. 5, 187 (2014).
- Csardi, G., Nepusz, T. The igraph software package for complex network research. InterJournal, Complex Systems. 1695 (5), (2006).
- Kramer, M. A., Cash, S. S. Epilepsy as a Disorder of Cortical Network Organization. Neuroscientist. 18 (4), 360-372 (2012).
- Ortega, G. J., Peco, I. H., Sola, R. G., Pastor, J. Impaired mesial synchronization in temporal lobe epilepsy. Clin Neurophysiol. 122 (6), 1106-1116 (2011).
- Bettus, G., et al. Decreased basal fMRI functional connectivity in epileptogenic networks and contralateral compensatory mechanisms. Hum Brain Mapp. 30 (5), 1580-1591 (2009).
- Pereira, F. R., et al. Asymmetrical hippocampal connectivity in mesial temporal lobe epilepsy: evidence from resting state fMRI. BMC Neurosci. 11, 66 (2010).
- Vega-Zelaya, L., Pastor, J., Tormo, I., de Sola, R. G., Ortega, G. J. Assessing the equivalence between etomidate and seizure network dynamics in temporal lobe epilepsy. Clin Neurophysiol. 127 (1), 169-178 (2011).
- Pastor, J., Sola, R. G., Ortega, G. J., Stevanovic, D. Hyper-Synchronization, De-Synchronization, Synchronization and Seizures. Epilepsy - Histological, Electroencephalographic and Psychological Aspects. , (2012).
- Stam, C. J., Nolte, G., Daffertshofer, A. Phase lag index: assessment of functional connectivity from multi channel EEG and MEG with diminished bias from common sources. Hum Bran Mapp. 28 (11), 1178-1193 (2007).
- Pastor, J., Sola, R. G. Utility of foramen ovale electrodes in temporal lobe epilepsy surgery. Recent Advances in Epilepsy. , 1-8 (2008).
This article has been published
Video Coming Soon
ABOUT JoVE
Copyright © 2025 MyJoVE Corporation. All rights reserved