Ultrasound-Guided Orthotopic Implantation of Murine Pancreatic Ductal Adenocarcinoma
In This Article
Summary
We describe a protocol for the ultrasound guided implantation of murine-derived pancreatic ductal adenocarcinoma cell lines directly into the native tumor site. This approach resulted in pancreatic tumors detectable by ultrasound scanning within 2-4 weeks of injection, and significantly reduced the proportion tumor cell seeding on the peritoneal wall as compared to surgical orthotopic implantation.
Abstract
The recent success of immune checkpoint blockade in melanoma and lung adenocarcinoma has galvanized the field of immuno-oncology as well as revealed the limitations of current treatments, as the majority of patients do not respond to immunotherapy. Development of accurate preclinical models to quickly identify novel and effective therapeutic combinations are critical to address this unmet clinical need. Pancreatic ductal adenocarcinoma (PDA) is a canonical example of an immune checkpoint blockade resistant tumor with only 2% of patients responding to immunotherapy. The genetically engineered KrasG12D+/-;Trp53R172H+/-;Pdx-1 Cre (KPC) mouse model of PDA recapitulates human disease and is a valuable tool for assessing therapies for immunotherapy resistant in the preclinical setting, but time to tumor onset is highly variable. Surgical orthotopic tumor implantation models of PDA maintain the immunobiological hallmarks of the KPC tissue-specific tumor microenvironment (TME) but require a time-intensive procedure and introduce aberrant inflammation. Here, we use an ultrasound-guided orthotopic tumor implantation model (UG-OTIM) to non-invasively inject KPC-derived PDA cell lines directly into the mouse pancreas. UG-OTIM tumors grow in the endogenous tissue site, faithfully recapitulate histological features of the PDA TME, and reach enrollment-sized tumors for preclinical studies by four weeks after injection with minimal seeding on the peritoneal wall. The UG-OTIM system described here is a rapid and reproducible tumor model that may allow for high throughput analysis of novel therapeutic combinations in the murine PDA TME.
Introduction
Pancreatic ductal adenocarcinoma (PDA) is a notoriously aggressive disease that is refractory to current treatments, with a dismal 5-year survival rate of 9%1. PDA recently surpassed breast cancer to become the third-leading cause of cancer-related mortality in the U.S. and is projected to become the second-leading cause (behind only lung cancer) by the year 20302. A number of features characteristic of the immunologically 'cold' PDA tumor microenvironment (TME)-including high infiltration of immunosuppressive myeloid cell populations3,4,5,6,7, dense stromal deposition8,9,10,11, and a dearth of T cells5,12,13-contribute to the failure of immunotherapies in PDA14. To this end, the use of a clinically-relevant animal model is an essential tool for investigating the efficacy of novel drug combinations for immunologically cold tumors in vivo.
The genetically engineered KrasG12D+/-;Trp53R172H+/-;Pdx-1 Cre (KPC) mouse model of PDA faithfully recapitulates salient clinical aspects of human PDA, including the molecular drivers of disease and histopathological features15. KPC tumors develop spontaneously in fully immunocompetent mice, allowing for interrogation of therapeutic approaches including chemotherapy16,17, immunotherapy18,19,20,21, and stroma-targeting therapy9,11,22 in vivo prior to the administration of these drugs in the clinical trial setting. Despite its many strengths as a preclinical model of PDA, the use of KPC mice is disadvantaged by the highly variable progression of spontaneous tumor development as tumor onset can range from 4 to 40 weeks (thus requiring the maintenance a large breeding colony)15. Additionally, KPC mice have the potential for polyclonal primary tumors23, and there is a rapid decline in animal health and increase in co-morbidities including cachexia and ascites as disease progresses15.
One alternative to the spontaneous KPC mouse model is to use an orthotopic implantation model of PDA24. The direct surgical implantation of tumor cell lines in to the native tissue site is a more cost-effective and predictable method of recapitulating the tissue-specific tumor microenvironment (TME) of PDA. Tumor implantation allows for injection of clonal tumor cell lines to genetically backcrossed mice5, allowing for host mice with additional genetic manipulations that would be time-consuming to breed in to the KPC mouse model. However, pancreatic tumor implantation requires a labor-intensive surgical procedure that introduces aberrant inflammation at the suture site in the abdominal wall24,25,26, and often includes a lengthy post-operative recovery27,28,29.
Technological advances in ultrasound imaging using rodent-specific transducers provides high resolution images in real-time. Guided by the ultrasound imaging of the injection needle movement in the peritoneal cavity, one can specifically implant tumor cells into the pancreas, leveraging the benefits of orthotopic tumor injections in the absence of surgical implantation and associated inflammation. This approach, termed ultrasound-guided orthotopic tumor implantation model (UG-OTIM) has been previously established in a xenograft models of pancreatic cancer30 as well as in several other cancer models including Ewing's sarcoma, neuroblastoma and bladder cancer31,32.
Here, we provide a detailed protocol for performing ultrasound-guided injections of tumor cell lines in to the murine pancreas. We show the resultant tumors recapitulate the histological and immunological features of the KPC TME and can therefore be used to investigate novel therapeutic combinations, including immunotherapies, to rapidly reveal the most promising treatments to move forward in to clinical trials.
Protocol
Animal protocols were reviewed and approved by the Institutional of Animal Care and Use Committee at the University of Pennsylvania. Female 5-to-6-week-old C57Bl/6 mice were purchased (see Table of Materials) and used after 1-3 weeks rest. The University Laboratory Animal Resources oversaw animal care.
1. Preparation of PDA tumor cell lines for injection
- Grow KPC-derived PDA cell line in tumor cell (TC) media: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS), 2mM L-glutamine and 83 μg/mL gentamicin.
- Allow cells to grow to 80-85% confluency in flasks maintained at 37°C and 5% CO2.
- Once the cells reach ideal confluency, decant the media from flasks and wash twice with warm (37°C), sterile phosphate-buffered saline (PBS), enough to cover the monolayer of adherent cells. Pipette of remaining PBS after final wash.
- Add warm (37°C) 0.05% trypsin-EDTA solution (0.5% stock trypsin-EDTA diluted 1:10 in Hanks'-based enzyme-free cell dissociation buffer) to cover the monolayer in each flask and incubate at 37°C for 3-5 minutes or until cells detach with tapping on the sides of the flask.
- Add 10-25mL of cold (4°C), sterile TC media in to each flask to stop the trypsinization reaction. Pour cell suspension into a 50mL conical(s), fill to 50mL with cold TC media.
- Centrifuge at 300g for 5 minutes at 4°C. Discard supernatant and resuspend pellet in cold, sterile DMEM (serum-free). If multiple conical tubes were used to collect cells, all pellets can be combined to a single conical at this step.
- Centrifuge at 300g for 5 minutes at 4°.
- Repeat steps 1.6-1.7 twice. In final wash, take an aliquot of cells for counting. Cell viability of ≥90% is recommended for in vivo injections.
- Prepare a uniform suspension of the PDA tumor cells at the desired concentration of tumor cells. We used 10-20 x 106 cells/mL (250,000 to 500,000 cells/25µL) in the appropriate amount of sterile, cold DMEM or PBS, but each cell line should be titrated in vivo.
- Keep cells cold, on ice, until ready to inject.
2. Pre-Surgical Preparation of Mice
NOTE: This step is recommended to be performed 24 hours prior to the procedure.
- Place cages containing experimental mice on a warmer set to 37°C.
- Obtain new, clean cages and place on a second warming platform set to 37°C.
- Thoroughly clean the biological safety cabinet, the induction chamber and the ultrasound (US) stage with sterilant (see Table of Materials).
- Turn the warming function of the US stage to 37°C.
- Turn on the anesthesia machine: adjust the dials on the tube splitter so that airflow is restricted to the induction chamber only. Turn on the oxygen tank and set to flow rate to 1 L/min. Turn on the isoflurane vaporizer to 2-3%.
- Place a single mouse into the induction chamber. Monitor mouse until no longer mobile and breathing has slowed.
- Adjust the dials on the splitter so that airflow is permitted to both the induction chamber and the nose cone. Quickly move mouse from the induction chamber and lay it in ventral recumbency on the warm US stage with its muzzle in the nose cone.
- Test the level of induction by observing any reflexive response to toe pinching. If there is none, the mouse is ready for hair removal.
- Place a small amount of eye lubricant (see Table of Materials) on both eyes to prevent tissue dehydration. Turn the mouse so that it lays in dorsal recumbency on the stage. Gently adhere the upper and lower extremities to the stage with paper tape in order to maximize exposure of the abdomen and secure the mouse to the stage.
- Use a sterile cotton-tip applicator to apply a generous layer depilatory cream to the upper left quadrant of the abdomen. The depilatory should be applied in the general area of the spleen and extend towards the midline. Allow to sit for about one minute.
- Test the degree of hair removal by gently using the opposite end of the cotton tip applicator to wipe away the depilatory cream, once it removes easily, wipe the abdomen clean with a dry gauze pad. Then wet a clean layer of gauze with a small amount of warm saline and wipe the area once more to completely remove the depilatory agent. Do not exceed 2 full minutes of direct contact on mouse skin in order to reduce the chance of chemical burns.
- Once the hair has been sufficiently removed from the abdomen, return mouse to a new, clean cage on warmer.
- While the first animal is undergoing hair removal on the US stage, the next animal can be added to the induction chamber.
- Before anesthetizing the next cage of mice, turn off the isoflurane and flush the induction chamber with oxygen. Clean the induction chamber and US stage/nose cone with sterilant. Repeat steps 2.5-2.14 until all cages and mice have undergone hair removal.
NOTE: Fasting animals by temporary withdrawal of food for a period prior to implantation can be considered to minimize visual obstruction of abdominal organs due to undigested food in stomach and intestines (12-24 hours). Water restriction is not recommended. If animals are fasted, it is recommended that they are treated with an injection of 1mL warm (37°C), sterile saline following tumor injection in order to prevent dehydration.
3. Ultrasound-Guided implantation of PDA cells
NOTE: All ultrasound procedures are performed using ultrasound imaging machine and software (see Table of Materials). The transducer has a center frequency of 40 MHz and a bandwidth of 22-55 MHz.
- Adjust the ultrasound platform such that the platform surface is parallel to the floor and the investigator faces the left side of the animal, with the animal's head to the right. Adjust the transducer position so that a transverse abdominal image will be obtained (Figure 1A).
- Anesthetize the mouse to be injected as described in steps 2.1-2.8. Stabilize the mouse on the US platform as described in step 2.9.
- Apply a generous amount of warm (37°C) ultrasound gel to the hairless section of the abdomen.
- Gently lower the transducer to contact the mouse abdomen. Adjust the transducer as needed until the pancreas is clearly visible. Locate the left kidney and spleen in order to provide an accurate orientation of the abdominal cavity.
NOTE: Because the transducer position has been changed to allow access to the left side of the abdomen, the X and Y axis on the stage controls are now inverted. - Load a 29G x ½" insulin syringe (see Table of Materials) with 25µL of tumor cell suspension. Wipe needle tip with sterile alcohol prep pad prior to injection in order to minimize tumor cell seeding in the abdominal wall.
- Using blunt-edge forceps, grasp the skin and peritoneal wall to increase tension at the desired injection site. Holding the syringe at approximately a 25°-45° angle to the ultrasound platform surface, slowly advance the needle through the skin and the peritoneal wall. Confirm the needle has punctured through the peritoneal wall before proceeding to the next step. A small pop should be felt as the needle pierces the peritoneal wall.
- Under ultrasound visualization, guide the needle directly into the pancreas (Figure 1B-C). Confirm the needle is within pancreas tissue by gently moving the syringe barrel up and down. If placement is correct, the needle tip will remain within the pancreas tissue while the syringe barrel is moving.
- Slowly inject the tumor cells and confirm the cells are being implanted in the desired location by the formation of a fluid bolus within the pancreas (visible on the ultrasound screen, Figure 1D).
NOTE: Some resistance should be felt while depressing plunger. Be careful not to pierce pancreas multiple times as this increases the likelihood of leakage into the abdominal cavity. - Once the full volume of suspension has been injected and a fluid bolus can be seen in the pancreas, keep needle very still for several seconds. Slowly retract needle from mouse abdomen, taking great care not to disturb the injected cells.
- Place the mouse in a clean, warm cage and ensure that the mouse fully recovers from anesthesia. Repeat this process for all animals.
- Before anesthetizing the next mouse, clean the induction chamber and US stage/nose cone with sterilant.
- Repeat steps 3.2-3.11 until all mice have been injected.
Representative Results
The goal of this report was to provide a detailed protocol for performing ultrasound-guided implantation of KPC-derived PDA cell lines. In the representative experiments shown in Figure 2-4, we confirm that UG-OTIM tumors grow at a consistent rate and in a dose-dependent manner. Furthermore, we show that UG-OTIM tumors recapitulate the salient immunological and histological features of the KPC TME. Thus, the UG-OTIM system is a preclinical PDA mouse model that can be used in a high-throughput manner to rapidly screen new treatment combinations in vivo.
Using the UG-OTIM protocol outlined here, the mice were prepared for implantation, secured to the heated ultrasound platform and the positions of both the platform and the transducer were adjusted for this procedure as shown in Figure 1A. High-resolution ultrasound imaging was used to identify an injection site within the mouse pancreas that could be targeted without perforation of either the kidney or spleen (Figure 1B). Under ultrasonographic visualization, the needle was carefully introduced to the abdominal cavity through the peritoneal wall and guided into the mouse pancreas (Figure 1C). After correct placement of the needle was established, the tumor cell suspension was injected very slowly into the pancreas. A successful implantation was confirmed by the presence of a bubble within the pancreas (Figure 1D). In early experiments, the mouse was sacrificed, and efficacy of the procedure was verified by directly visualizing a fluid bolus in the gross pancreas tissue (Figure 1E).
Tumor implantation and growth rate was monitored by weekly ultrasound imaging. Successful implantations produced tumors that were contained within the borders of the pancreas throughout the time of the experiment (Figure 2A). The ultrasound software (see Table of Materials) used allowed for tumor area and volume to be determined for each time point as well as for 3D mapping of measured tumors to be generated (Figure 2B), and the 3D images were confirmed at the time of mouse necropsy (Figure 2C). An improper cell injection during the UG-OTIM procedure can result in the development of a peritoneal wall tumor (a representative image of which is shown in Figure 2D). Mice that present with peritoneal tumors can be excluded from further studies.
To determine the concentration of cells optimal for use in preclinical studies, a C57Bl/6 KPC-derived PDA cell line (4662)9 was injected in to naïve, wild-type C57Bl/6 mice across six independent experiments. This cell line (passaged in vitro six times) was derived from a fully backcrossed KPC tumor-bearing mouse (>10 generations, confirmed by SNP-analysis19) to prevent molecular histocompatibility complex mismatch tumor rejection antigens. Tumor cells were injected at a low titer (1.25 x 106 cells/25µL) and at a high titer (5 x 106 cells/25µL) dose. The high titer tumor injections resulted in a larger proportion of tumor-bearing animals three weeks after injections compared to the low titer cohort (Figure 3A). Despite the delay in tumor onset, the overall tumor growth rate was not significantly different between the two doses (Figure 3B). Similarly, while the survival rate between the two cohorts was not significantly different, the data trend towards slightly improved survival in the low titer cohort (Figure 3C). The high titer cohort also produced a greater proportion of mice with tumors that were enrollable in preclinical studies (designated at ≥20mm3 tumor volume) by four weeks post-injection than the low titer cohort (Figure 3D). The majority of mice from both high and low titer cohorts presented with enrollable tumors by day 25 and developed end-stage disease symptoms including ascites (data not shown). Metastases, which do not occur using 4662 at the cell doses from this protocol, may be modeled with different cell lines or doses33.
The UG-OTIM method required a mastery of fine motor skills to accurately localize the desired injection site, which was challenging in our earliest experiments. For this reason, we included a table depicting the number of animals that developed tumors within the pancreas (successful implantations) compared to the total number of animals that underwent ultrasound-guided tumor implantation (Table 1). Animals were eliminated from future analyses if tumors developed in an undesired location (i.e., kidney) or if there was no evidence of tumor by six weeks post-injection, as indicated. The weekly progression of the proportion of mice bearing enrollable pancreatic tumors (≥20mm3 tumor volume) from each experiment is also shown in Table 1.
To determine if there was a benefit to using the UG-OTIM approach rather than the traditional surgical orthotopic model (beyond time investment after gaining proficiency at the technique), we compared the seeding of PDA tumors in the peritoneal wall of mice after each procedure. We found that only 2/31 mice (6.5%) developed unintended peritoneal wall tumors after UG-OTIM injections, as compared 7/15 mice that developed peritoneal wall tumors after surgical injection (46.6%, p < 0.0029) (Table 1). Thus, the rate of seeding additional tumors in the peritoneum is greatly reduced in the UG-OTIM method as compared to surgical implantation.
Upon sacrifice of mice bearing UG-OTIM tumors, we found that the gross anatomy of the tumors was similar to spontaneous KPC tumors (Figure 4A). Histological analysis demonstrated a pattern of abnormal ductal structures that was similar in both models and that recapitulated the morphology of the human disease (Figure 4B). To investigate the immune infiltrate within both KPC and UG-OTIM tumors, representative histological samples were stained for CD3 (expressed by T cells) and F4/80 (expressed by macrophages). In both models, staining patterns revealed tumors that were poorly infiltrated by T cells (Figure 4C), but highly infiltrated by macrophages (Figure 4D). This finding is consistent with the immunologically cold phenotype of most human and KPC PDA samples5,7,12.
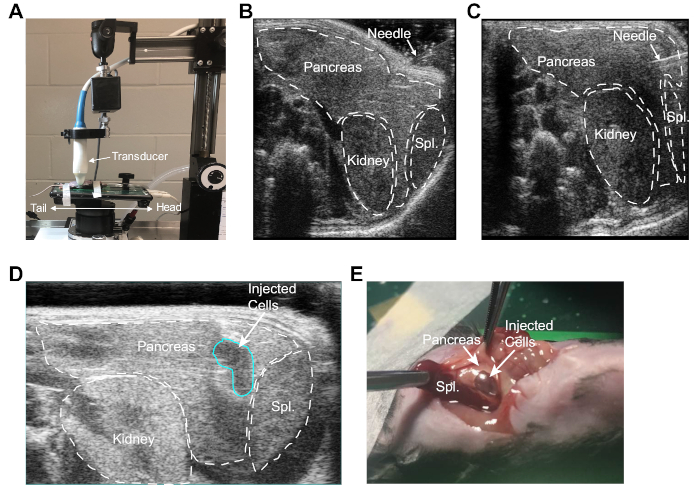
Figure 1: Ultrasound-guided implantation of PDA cells into the murine pancreas. (A) Orientation of mouse, ultrasound stage, and ultrasound probe used to obtain a high-resolution image of abdominal organs. Note the stage and platform have been turned 90° from the standard orientation to allow easy access to the upper left quadrant of mouse abdomen. (B) Ultrasonographic image depicting the identification of kidney, spleen and pancreas. Here the injection needle is positioned against the mouse abdomen. (C) Ultrasonographic image depicting the needle within the mouse pancreas. (D) Ultrasonographic image depicting the bubble at the injection site (outlined in blue) following controlled injection of tumor cells in to the pancreas. (E) Laparotomy revealing the fluid bolus containing PDA cells in the pancreas after ultrasound guided injection. Please click here to view a larger version of this figure.
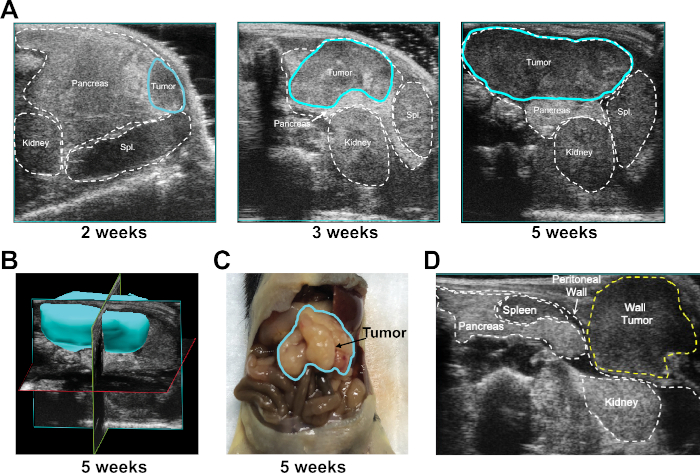
Figure 2: Monitoring tumor growth after UG-OTIM injection. (A) Representative ultrasonographic image of UG-OTIM tumor (outlined in blue) at 2, 3, and 5 weeks post-injection, as indicated. (B) Representative reconstructed 3D image of UG-OTIM tumor 5 weeks post-injection using the ultrasound software. (C) Representative gross anatomy of UG-OTIM tumor 5 weeks post-injection upon mouse necropsy. (D) Representative ultrasonographic image of a peritoneal wall tumor growing in the subcutaneous layer after improper cell injection at 7 weeks post-injection. Please click here to view a larger version of this figure.
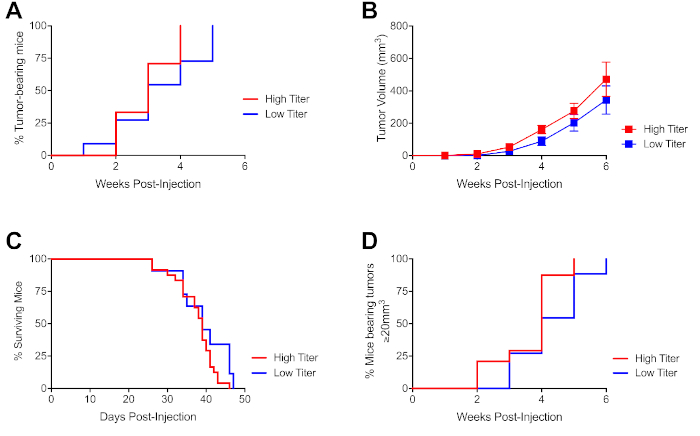
Figure 3: Dose-dependent onset of enrollable tumors following ultrasound guided injection of PDA cells. (A) Proportion of tumor-bearing mice at indicated time points after injection as described in Figure 1 with high titer (500,000 cells/25µL) or low titer (125,000 cells/25µL) tumor cells, as indicated. (B) Tumor growth kinetics of mice from (A), each symbol represents a group of mice, error bars indicate SEM. (C) Proportion of mice from (A) alive at indicated time points after injection. Mice were euthanized or censored if tumors were >1000mm3 or body condition was poor due to tumor comorbidities. (D) Time to enrollable tumor onset for mice from (A). Enrollable tumors are considered to be ≥20mm3 in volume. Data representative of 4 independent experiments with n=8-20 mice/experiment. Please click here to view a larger version of this figure.
| Experiment | Pancreas-tumor bearing/total injections | Week 1 (Enrollable) | Week 2 (Enrollable) | Week 3 (Enrollable) | Week 4 (Enrollable) | Seeded Peritoneal Tumors |
| High Titer | 24/31 | ND | 8/24 (3/24) | 15/24 (7/24) | 23/23 (20/23) | 2/20 |
| Low Titer | 11/17 | ND | 3/11 (0/11) | 6/11 (3/11) | 9/11 (5/11) | 0/11 |
| Surgical Injection | 15/17 | ND | ND | 15/15 (9/15) | 15/15 (14/15) | 7/15 |
Table 1: Number of successful UG-OTIM tumors compared to surgical implantation. Data combined from 2-4 independent experiments per high or low titer condition with n=5-10 mice per experiment. "Surgical injection" indicates mice that received abdominal laparoscopic surgical injection of 125,000 tumor cells. "Tumor-bearing" indicates mice with a pancreatic tumor. "Enrollable" indicates proportion of tumor-bearing mice at each time point with a tumor volume >20mm3. "Seeded Peritoneal Tumors" indicates the total proportion of tumor-bearing mice that had concomitant seeding of tumors on the peritoneal wall from tumor cell injection. Mice with tumors presenting incorrectly in tissues other than the pancreas (i.e., kidney) were excluded from "tumor-bearing" populations (but included in total injected mice). ND, not determined. Frequency of peritoneal wall seeding comparing high and low titer groups combined versus surgical implantation, p < 0.0029 via 2-tailed T test with Mann-Whitney post-test.
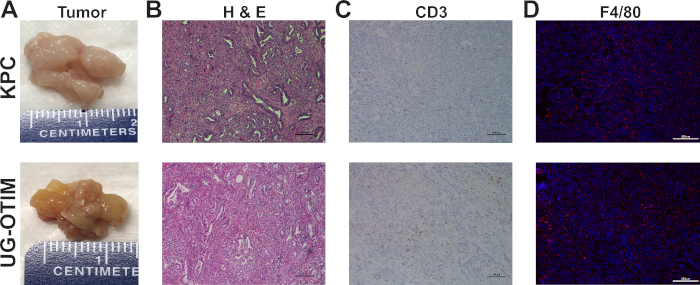
Figure 4: UG-OTIM tumors recapitulate the KPC tumor microenvironment. Representative images are shown. Top row, KPC tumors. Bottom row, UG-OTIM tumors at 5 weeks post-implantation. (A) Gross anatomy of excised tumors upon necropsy. (B) H&E (10X, bar=100µm) (C) Immunohistochemistry staining for CD3 (brown) (10X, bar=100µm). (D) Immunofluorescent staining of F4/80 (red) and DAPI (blue) (4X, bar=500µm). Please click here to view a larger version of this figure.
Discussion
We show here that the use of high-resolution ultrasonography to direct implantation of murine PDA cell lines to the autochthonous tissue site is a reliable alternative to both the KPC and surgical orthotopic model systems. UG-OTIM produces biologically relevant tumors that retain the immunopathological features of PDA with a shortened time-frame to tumor-diagnosis and reliable tumor growth kinetics. Ultrasound guided injection can therefore serve as a useful tool for rapid production of mice bearing orthotopically implanted PDA tumors, allowing for investigation of therapeutic combinations in a clinically relevant model.
Ultrasound-guided implantation offers important improvements over standard models of preclinical investigation. Firstly, this procedure eliminates the time-intensive monitoring of KPC mice for the development of spontaneous tumors by directly implanting fully C57BL/6 backcrossed PDA cells in to the murine pancreas. Secondly, similar to traditional surgical orthotopic injections, the UG-OTIM approach allows for control over the cell line injected, including selection of a monoclonal tumor cell line and/or ex vivo manipulation of the cell line, as well as control over the host receiving the tumor cell implantation. Thirdly, this minimally invasive technique avoids the arduous labor of survival surgery and bypasses the complicated post-operative recovery period for the animals as well as inflammatory signals from surgical wound healing. Finally, UG-OTIM tumors - similar to surgical implantation - recapitulate the TME observed in the KPC mice, including low T cell infiltration and high macrophage infiltration. Thus, the UG-OTIM model retains key features of the KPC tumors without the additional complications that retard therapeutic investigations in the spontaneous KPC model.
A number of critical steps in the protocol are key to master for the success of the technique. Expertise in murine ultrasound imaging is essential for this procedure, but the manual dexterity required to successfully implant cells in the pancreas is a skill set that must be developed independently. For mice on a 12-hour light/dark cycle, fasting the animals overnight ensured the stomach and intestines were cleared of any undigested food that could block view of the pancreas, kidney and spleen by ultrasound. Additionally, each cell line used for orthotopic injection should be titrated prior to further experiments to understand the growth kinetics and determine the metastatic potential33. During injection, the use of forceps to pinch skin at the injection site created the tension needed to gently puncture through both the skin and peritoneal wall. A key step in the procedure was to carefully guide the needle into the pancreas without perforating the tissue or puncturing an off-target site such as the spleen or kidney. Confirmation of a fluid bolus was the best indicator of successful tumor cell injection in the proper tissue. After injection, the needle should be withdrawn slowly so as not to disturb the fluid bolus. We found that a series of trial injections using either DMEM or Trypan Blue helped to develop a mastery of the fine motor skills needed for this injection.
During troubleshooting of this procedure, we identified a number of factors that impacted the success of the protocol. In trial experiments, our most frequent error was perforating the kidney during implantation, which occurred more frequently in our early experiments suggesting that regular exercise of this skill improves proficiency. Additionally, we found that confirming the presence of a fluid bolus after tumor cell injection via both ultrasound and direct visualization at necropsy during the troubleshooting phase improved successful injection technique. If the formation of a bubble is not confirmed by ultrasound during the injection, the location of the needle can be adjusted before fully depressing the syringe to release the remaining bolus of tumor cells. We also observed that suspension volumes injected too quickly resulted in the spillage of tumor cells into the peritoneal cavity or collapse of the fluid bolus in the pancreas. Generally, these animals went on to develop pancreatic tumors with the exception of n=7 animals that showed no evidence of tumor 4 weeks post-injection. This result was reported only in our first attempts (and 6/7 animals were injected with a low titer of tumor cells). Mice that have questionable tumor cell injections, or requiring repositioning of the needle, should be closely monitored for the development of tumors outside of the pancreas.
The foremost limitations of the ultrasound-guided method are the availability of the required instruments and the technical skill associated with tumor implantation. The procedure is not completely sterile, as the mouse is injected non-sterilely on the ultrasound platform, with the syringe and needle tip passing through the ultrasound gel. Although we have seen no evidence of infection in n=148 mice across a total of 8 independent experiments since initiating these studies, it is possible that an infectious agent could enter the pancreas through the injection needle during this process. As such, as many aspects of the protocol as possible (including gloves, ultrasound surfaces, ice boxes) should be sprayed with disinfectant or 70% ethanol to reduce the potential exposure to pathogens. An additional limitation of the current protocol was the lack of metastasis using the 4662 cell line at the current dilutions. Each cell line used in the UG-OTIM system should be titrated for the desired growth rates as well as metastatic potential33. Finally, our current protocol established techniques for injecting tumor cells in a single-cell suspension. However, the addition of an extracellular matrix substrate could be added to potentially enhance tumor establishment and prevent tumor cell leakage (as it is used in surgical implantation models27,30,31,32). Thus, many of the limitations of UG-OTIM can be overcome with appropriate testing of the cell lines being used in the orthotopic injections.
In summary, the UG-OTIM model is a precise method of tissue-directed injection of tumor cells in to the murine pancreas. This minimally invasive implantation technique benefits both the investigator and the animals by reducing procedure time, minimizing post-surgical complications and improving accuracy of injection. Tumors arising from UG-OTIM injections retain the characteristic immunobiological features of spontaneous KPC tumors, have reliable time to tumor onset, and reproducible tumor growth kinetics. Thus UG-OTIM model can be used in a relatively high-throughput manner to interrogate therapeutic combinations in a preclinical setting to reveal novel treatments for patients with the greatest unmet clinical need.
Disclosures
The authors have no disclosures.
Acknowledgements
The authors wish to thank Dr. Robert Vonderheide and all members of the Vonderheide laboratory, all members of the Pancreatic Cancer Mouse Hospital, Dr. Ben Stanger, the Pancreatic Cancer Research Center at the University of Pennsylvania, and Devora Delman for helpful discussions. This work is supported by funding from the Parker Institute for Cancer Immunotherapy Fellow Award (KTB) and the Pancreatic Cancer Research Center at the University of Pennsylvania (CC).
Materials
| Name | Company | Catalog Number | Comments |
| 50 mL Conicals | Thomas Scientific | 2602A26 | |
| Blunt edged forceps | Fine Science Tools | 11000-12 | |
| Cell Dissociation Buffer | Thermo-Fisher | 13151014 | |
| Cotton Tipped swabs | Thermo-Fisher | 19062614 | |
| Covidien Monoject 3/10mL, 29G X 1/2" | Thermo-Fisher | 8881600145 | |
| Depilatory Agent | Amazon | Nair Body Lotion | |
| DMEM | Thermo-Fisher | 10-566-016 | |
| FBS | Gemini Bio-oroducts | 100-106 | |
| Flask | Sigma-Aldrich | CLS430825 | |
| Forceps (blunt edge) | Fine Science Tools | 11000-12 | |
| Gauze | Fisher | 13-761-52 | |
| Gentamicin | Thermo-Fisher | 15750060 | |
| Induction Chamber | VetEquip | 941444 | |
| Isofluorane | Penn Vet Supply | VED1350 | |
| Isofluorane Vaporizer | VetEquip | 911103 | |
| L-glutamine | Thermo-Fisher | 25030081 | |
| Optixcare | MidWest Veterinary Supply | 052.50310.3 | |
| Paper Tape | Medline | MMM1530Z5 | |
| PBS | Thermo-Fisher | 14-190-250 | |
| Slide warmer | C&A Scientific | XH-2001 | |
| Sterilant (Clidox-S) | Fisher Scientific | NC0332382 (activator) NC9189926 (base) | Needs to be combined according to manufacturer's instructions |
| Sterile Alcohol prep pad | Covidien | 6818 | |
| Trypsin | Thermo-Fisher | 15090046 | |
| Ultrasound gel | Thermo-Fisher | 03-34-1LT | |
| Visualsonics Ultrasound Vevo 2100 | Visual Sonics | Vevo 2100 |
References
- Siegel, R. L., Miller, K. D., Jemal, A. Cancer statistics, 2019. CA Cancer Journal for Clinicians. 69 (1), 7-34 (2019).
- Rahib, L., et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Research. 74 (11), 2913-2921 (2014).
- Chao, T., Furth, E. E., Vonderheide, R. H. CXCR2-Dependent Accumulation of Tumor-Associated Neutrophils Regulates T-cell Immunity in Pancreatic Ductal Adenocarcinoma. Cancer Immunology Research. 4 (11), 968-982 (2016).
- Steele, C. W., et al. CXCR2 Inhibition Profoundly Suppresses Metastases and Augments Immunotherapy in Pancreatic Ductal Adenocarcinoma. Cancer Cell. 29 (6), 832-845 (2016).
- Li, J., et al. Tumor Cell-Intrinsic Factors Underlie Heterogeneity of Immune Cell Infiltration and Response to Immunotherapy. Immunity. 49 (1), 178-193 (2018).
- Beatty, G. L., et al. Exclusion of T Cells From Pancreatic Carcinomas in Mice Is Regulated by Ly6C(low) F4/80(+) Extratumoral Macrophages. Gastroenterology. 149 (1), 201-210 (2015).
- Bayne, L. J., et al. Tumor-derived granulocyte-macrophage colony-stimulating factor regulates myeloid inflammation and T cell immunity in pancreatic cancer. Cancer Cell. 21 (6), 822-835 (2012).
- Beatty, G. L., et al. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science. 331 (6024), 1612-1616 (2011).
- Lo, A., et al. Tumor-Promoting Desmoplasia Is Disrupted by Depleting FAP-Expressing Stromal Cells. Cancer Research. 75 (14), 2800-2810 (2015).
- Rhim, A. D., et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 25 (6), 735-747 (2014).
- Ozdemir, B. C., et al. Depletion of Carcinoma-Associated Fibroblasts and Fibrosis Induces Immunosuppression and Accelerates Pancreas Cancer with Reduced Survival. Cancer Cell. 28 (6), 831-833 (2015).
- Clark, C. E., et al. Dynamics of the immune reaction to pancreatic cancer from inception to invasion. Cancer Research. 67 (19), 9518-9527 (2007).
- Stromnes, I. M., Hulbert, A., Pierce, R. H., Greenberg, P. D., Hingorani, S. R. T-cell Localization, Activation, and Clonal Expansion in Human Pancreatic Ductal Adenocarcinoma. Cancer Immunology Research. 5 (11), 978-991 (2017).
- Morrison, A. H., Byrne, K. T., Vonderheide, R. H. Immunotherapy and Prevention of Pancreatic Cancer. Trends in Cancer. 4 (6), 418-428 (2018).
- Hingorani, S. R., et al. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell. 7 (5), 469-483 (2005).
- Yip-Schneider, M. T., et al. Dimethylaminoparthenolide and gemcitabine: a survival study using a genetically engineered mouse model of pancreatic cancer. BMC Cancer. 13, 194 (2013).
- Frese, K. K., et al. Nab-Paclitaxel potentiates gemcitabine activity by reducing cytidine deaminase levels in a mouse model of pancreatic cancer. Cancer Discovery. 2 (3), 260-269 (2012).
- Stromnes, I. M., et al. T Cells Engineered against a Native Antigen Can Surmount Immunologic and Physical Barriers to Treat Pancreatic Ductal Adenocarcinoma. Cancer Cell. 28 (5), 638-652 (2015).
- Byrne, K. T., Vonderheide, R. H. CD40 Stimulation Obviates Innate Sensors and Drives T Cell Immunity in Cancer. Cell Reports. 15 (12), 2719-2732 (2016).
- Winograd, R., et al. Induction of T-cell Immunity Overcomes Complete Resistance to PD-1 and CTLA-4 Blockade and Improves Survival in Pancreatic Carcinoma. Cancer Immunology Research. 3 (4), 399-411 (2015).
- Keenan, B. P., et al. A Listeria vaccine and depletion of T-regulatory cells activate immunity against early stage pancreatic intraepithelial neoplasms and prolong survival of mice. Gastroenterology. 146 (7), 1784-1794 (2014).
- Jiang, H., et al. Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy. Nature Medicine. 22 (8), 851-860 (2016).
- Maddipati, R., Stanger, B. Z. Pancreatic Cancer Metastases Harbor Evidence of Polyclonality. Cancer Discovery. 5 (10), 1086-1097 (2015).
- Foster, D. S., Jones, R. E., Ransom, R. C., Longaker, M. T., Norton, J. A. The evolving relationship of wound healing and tumor stroma. Journal of Clinical Investigation Insight. 3 (18), (2018).
- Kasper, M., et al. Wounding enhances epidermal tumorigenesis by recruiting hair follicle keratinocytes. Proceedings of the National Academy of Sciences. 108 (10), (2010).
- Stuelten, C. H., et al. Acute Wounds Accelerate Tumorigenesis by a T Cell-Dependent Mechanism. Cancer Research. 68 (18), (2008).
- Qiu, W., Su, G. H. Development of orthotopic pancreatic tumor mouse models. Methods of Molecular Biology. 980, 215-223 (2013).
- Moreno, J. A., Sanchez, A., Hoffman, R. M., Nur, S., Lambros, M. P. Fluorescent Orthotopic Mouse Model of Pancreatic Cancer. Journal of Visualized Experiments. (115), (2016).
- Erstad, D. J., et al. Orthotopic and heterotopic murine models of pancreatic cancer and their different responses to FOLFIRINOX chemotherapy. Disease Models and Mechanisms. 11 (7), (2018).
- Huynh, A. S., et al. Development of an orthotopic human pancreatic cancer xenograft model using ultrasound-guided injection of cells. Public Library of Science One. 6 (5), e20330 (2011).
- Thomas, T. T., et al. Utilization of Ultrasound-guided Tissue-directed Cellular Implantation for the Establishment of Biologically Relevant Metastatic Tumor Xenografts. Journal of Visualized Experiments. (135), (2018).
- Jager, W., et al. Minimally invasive establishment of murine orthotopic bladder xenografts. Journal of Visualized Experiments. (84), e51123 (2014).
- Aiello, N. M., Rhim, A. D., Stanger, B. Z. . Orthotopic injection of pancreatic cancer cells. , (2016).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved