Interventional Diagnostic Procedure: A Practical Guide for the Assessment of Coronary Vascular Function
In This Article
Summary
The purpose of this practical guide is to provide information on the preparation and administration of an interventional diagnostic procedure in clinical practice. It discusses some key preparation and safety considerations, as well as tips for procedural success.
Abstract
Approximately 40% of patients undergoing invasive coronary angiography for investigation of angina are found to have no obstructive coronary artery disease (ANOCA). Abnormal coronary function underlies coronary vasomotion syndromes including coronary endothelial dysfunction, microvascular angina, vasospastic angina, post-PCI angina and myocardial infarction with no obstructive coronary arteries (MINOCA). Each of these endotypes are distinct subgroups, characterized by specific disease mechanisms. Diagnostic criteria and linked therapy for these conditions are now established by expert consensus and clinical guidelines.
Coronary function tests are performed as an adjunctive interventional diagnostic procedure (IDP) in appropriately selected patients during coronary angiography. This aids differentiation of patients according to endotype. The IDP includes two distinct components: a diagnostic guidewire test and a pharmacological coronary reactivity test. The tests last approximately 5 minutes for the former and 10-15 minutes for the latter. Patient safety and staff education are key.
The diagnostic guidewire test measures parameters of coronary flow limitation (fractional flow reserve [FFR], coronary flow reserve [CFR], microvascular resistance [index of microvascular resistance (IMR)], basal resistance index, and vasodilator function [CFR, resistive reserve ratio (RRR)]).
The pharmacological coronary reactivity test measures the vasodilator potential and propensity to vasospasm of both the main coronary arteries and the micro-vessels. It involves intra-coronary infusion of acetylcholine and glyceryl trinitrate (GTN). Acetylcholine is not licensed for parenteral use and is therefore prescribed on a named-patient basis. Vasodilatation is the normal, expected response to infusion of physiological concentrations of acetylcholine. Vascular spasm represents an abnormal response, which supports the diagnosis of vasospastic angina.
The purpose of this practical guide is to provide information on the preparation and administration of the IDP in clinical practice. It discusses some key preparation and safety considerations, as well as tips for procedural success. The IDP supports stratified medicine for a personalized approach to health and wellbeing.
Introduction
Approximately 40% of patients undergoing invasive coronary angiography for investigation of suspected angina are found to have no obstructive coronary artery disease (ANOCA)1. Anatomical imaging in coronary angiography has a spatial resolution of approximately 0.3 mm, which lacks sensitivity in visualizing the resistance arterioles that help to govern myocardial blood flow2. Supply/demand mismatch of myocardial blood flow relative to requirements may induce ischemia and drive angina symptom burden.
Coronary function testing provides information on the health of the coronary circulation, the presence and nature of abnormal coronary function. The goal of testing is therefore to aid in the diagnosis of coronary vasomotion disorders. These include coronary endothelial dysfunction, microvascular angina, vasospastic angina, post-percutaneous coronary intervention (PCI) angina and myocardial infarction with non-obstructive coronary arteries (MINOCA). These conditions are associated with impaired quality of life, higher morbidity and healthcare resource utilization3,4,5.
Coronary function tests are performed either as an adjunctive interventional diagnostic procedure (IDP) at the time of invasive coronary angiography, or non-invasively by cardiac MRI or transthoracic Doppler echocardiography. Its role within the diagnostic pathway has been discussed elsewhere6. Diagnostic criteria and linked therapy for the different endotypes of coronary vasomotion disorders are now established by expert consensus7 and clinical guidelines8,9.
Despite the advent of guidelines and objective testing, there remains variation in clinical practice for the diagnosis and management of this heterogenous group of patients. An alternative approach to coronary function testing is to institute a trial of therapy in all patients. Proponents of this approach cite a shorter procedural duration and reduced upfront cost from the procedural diagnostic guidewires and pharmacological testing agents.
However, stratifying patients by the differing disease mechanisms and personalizing their therapies is an approach that better aligns with the concept of precision medicine10. Indeed, the CorMicA trial served evidence that this approach may improve angina and quality of life in patients with ANOCA11,12.
Here, we present a protocol for an IDP to assess coronary vasomotor function. It is intended to enhance diagnostic power in the cardiac catheterization laboratory for patients with ANOCA.
General considerations for the IDP
The IDP includes two distinct components6: a diagnostic guidewire test and a pharmacological coronary reactivity test. A common approach is to perform these tests in sequence, with acetylcholine administered before the diagnostic guidewire is withdrawn. The benefit of this approach is that the guidewire will stabilize the guide catheter, which in turn helps to ensure selective intracoronary infusion of acetylcholine and GTN.
The multidisciplinary team should involve an interventional cardiologist with prior experience of the acetylcholine test protocol, supported by the catheter laboratory team, including nurses, a physiologist, and a radiographer. Involving a second cardiologist may be helpful. The tests last approximately 5 minutes for the diagnostic guidewire component and 10-15 minutes for the pharmacological component.
Patient selection
The IDP is performed at the time of invasive coronary angiography, either as a planned procedure or as an ad-hoc "follow-on" if no obstructive coronary artery disease is found, with the condition that informed consent has been obtained. The patient should be aware of the additional risks and benefits of the adjunctive interventional diagnostic procedure. Unless contraindicated, most patients undergoing investigation for possible angina may be considered. This is particularly helpful in patients who have had previous anatomical imaging (invasive or otherwise) to suggest the possibility of ANOCA.
Advanced renal dysfunction, where contrast media administration may be detrimental to renal function, is a relative contraindication to invasive angiography. Relative contraindications to acetylcholine testing include severe chronic obstructive pulmonary disease (COPD) and obstructive coronary artery disease (CAD). Vasoactive medications (such as beta-blockers, calcium channel blockers, and nitrates) and caffeine-containing drinks should be withheld for at least 24 hours pre-procedure.
The diagnostic guidewire
Current diagnostic guidewires utilize a combined technology of a pressure sensor with either: 1) a temperature sensor to estimate flow based on the principles of thermodilution, or 2) an ultrasound sensor to estimate flow based on the Doppler principle. Thermodilution-based wires are safe and straightforward to use11. Doppler/pressure wires may have higher accuracy and better correlation with non-invasive testing results, but at the expense of wire maneuverability13. This review focuses on thermodilution-based guidewires.
The pharmacological reactivity test
Pharmacological tests of coronary reactivity involve intracoronary infusion of acetylcholine and glyceryl trinitrate (GTN), to assess the vasodilator potential and propensity to vasospasm of the main coronary arteries and microcirculation. Vasodilatation is the normal, expected response to infusion of physiological concentrations of acetylcholine. Vascular spasm represents an abnormal response, which would support the diagnosis of vasospastic angina. Okumura et al. demonstrated that intracoronary acetylcholine had 90% sensitivity and 99% specificity for diagnosing epicardial spasm14.
Safety considerations
The half-life of acetylcholine is 1-2 seconds. Any physiological responses will cease within 5-10 seconds. More than three decades of experience with intracoronary acetylcholine tests support overall procedural safety. Self-limiting bradycardia and heart block are to be expected. These effects may be more profound if acetylcholine is infused into the dominant coronary artery, but should nonetheless be transient.
Atropine should be at hand, ready for administration, however the short half-life of acetylcholine means that it is rarely required. A simple cough maneuver by the patient is usually sufficient to restore sinus rhythm. Shortening of the atrial refractory period and increased propensity to atrial fibrillation (<10%) can occur, but this is typically short lived.
A review by Sueda et al. found a rate of 0.6% for major complications, such as ventricular tachycardia, cardiac tamponade and shock with intracoronary acetylcholine15. More recent experience in the CorMicA study11 did not reveal any serious adverse events secondary to the IDP. Together, these findings reinforce the importance of informed consent. Acetylcholine should be pre-ordered by a cardiologist on a named patient basis from the pharmacy.
Thromboprophylaxis and loading with antiplatelet therapy
Standard coronary angiography is associated with a small risk of thromboembolism. Subclinical micro-emboli may occur, as revealed by transcranial Doppler studies16. Further, guidewire-based coronary instrumentation carries a very small risk of vascular injury, which may in turn necessitate PCI. Therefore, platelet inhibition may be considered for thromboprophylaxis at the time of the procedure, and to optimize patient safety. Indeed, the pre-procedural clinical plan for some of these patients may already include antiplatelet therapy, due to the possibility of obstructive coronary artery disease and/or PCI at the time of angiography. Since radial artery access is routinely used, the risks of bleeding are considered minimal. There is no interaction anticipated between dual antiplatelet therapy, including a loading dose of aspirin and clopidogrel, and the coronary response to acetylcholine.
Protocol
The following protocol adheres to the guidelines of our institution's human research ethics committee. Methods from this protocol have been included within ethics committee-approved research studies in our institution17,18.
1. Coronary angiography
- Before starting, have the catheter laboratory team undertake a 'huddle' to review the clinical case and plan the procedure. This includes preparation for medication and/or equipment should adverse events occur (for instance the need for pacing).
- Consider adopting the following checklist: written informed consent, including the off-label use of acetylcholine, indication and potential risks of the procedure, history of allergy, and plan for procedural thromboprophylaxis, sedation and/or pain-control.
- Obtain arterial access using standard Seldinger technique. Radial artery access is recommended as per contemporary guidelines.
- Administer intra-arterial nitrate to reduce propensity to radial artery spasm. Modest doses of short-acting nitrate (e.g., 200 µg of GTN) are recommended. Avoid calcium channel antagonists.
- Give unfractionated heparin 5000 IU and actively manage the activated clotting time (ACT) to ~250 seconds.
- Perform standard coronary angiography to obtain orthogonal views of all main coronary artery branches.
- Record left ventricular end diastolic pressure (LVEDP), if feasible, to provide information on possible alternative explanations for symptoms (e.g., heart failure).
- Size the guide catheter selection according to the patient stature, e.g., 6 Fr and 3.5 size for the standard patient, or 5Fr and 3.0 size for those of smaller stature.
NOTE: Careful attention to the aortic pressure waveform will inform the operator about 'pressure damping' and the risk of coronary dissection. An 'Extra Back-Up' catheter may secure a more stable position in the left main coronary artery, but care is needed during manipulation to avoid vessel injury.
2. Diagnostic guidewire test (FFR, CFR, IMR, RRR)
- Engage the coronary artery with a guide catheter of choice.
- With the guide catheter engaged and co-axial, administer 200 µg of GTN to attenuate any epicardial coronary spasm.
- Ensure that the ACT is ~250 seconds before instrumentation of the coronary artery.
- While avoiding handling the diagnostic guidewire sensor, advance the sensor to the tip of the guide catheter.
- Flush the guide catheter to avoid contrast pressure damping. Allow 30 seconds for resting conditions to return before 'equalizing' pressure with the invasive aortic root pressure. Ensure that the catheter system is fully closed (e.g., introducer needle fully removed) and 'pressure damping' is not present. Meticulous setup reduces the risk of subsequent errors from 'signal drift'.
- Advance the diagnostic guidewire to the distal 1/3 of the coronary artery. In the absence of a clinical indication to select a specific coronary artery, select the left anterior descending (LAD) artery as the default due to the volume of myocardium subtended.
- If encountering difficulty advancing the diagnostic guidewire, consider use of a standard workhorse coronary guidewire as a 'buddy-wire'. Alternatively, a different coronary artery may be selected if vascular injury remains a concern.
- With the diagnostic guidewire in appropriate position within the vessel, flush the guide catheter with room-temperature normal saline and allow 30 seconds for resting physiology to return.
- Store a fluoroscopy image of the diagnostic guidewire to document position within the coronary artery.
- Record resting pressure indices, including resting Pd/Pa and RFR.
- Before recording resting thermodilution transit times, flush the guide catheter with room temperature saline to displace saline within the catheter that has been warmed by the patient's body temperature.
- Using a dedicated 3 mL syringe (or 5 mL syringe in large left dominant coronary arteries), administer brisk 3 mL boluses of room-temperature normal saline via the guide catheter.
CAUTION: Care should be taken to avoid injection of air into the coronary artery. Ensure guide catheter is co-axially intubated during injections to avoid hydro trauma. - Repeat the 3 mL boluses of room-temperature normal saline as required. Inspect the recorded transit times and replace any artefactual and/or outlier readings.
- Set up the linked diagnostic software to prepare for hyperemic measurements.
NOTE: For the coronary pressure/flow relationship to become linear, resistance should be minimized and stable. This can be achieved with IV adenosine (140-210 µg/kg/min). Contrast-FFR (ischemic threshold 0.83) is an alternative to FFR with IV adenosine but does not provide the stable hyperemic conditions necessary for thermodilution measurement. - Inform the patient of potential adenosine side-effects (transient dyspnea, flushing and chest discomfort).
- Commence IV adenosine (140 µg/kg/min) infusion via a large peripheral venous cannula.
- Keep manifold manipulation to a minimum to avoid movement-induced pressure trace artefacts.
- Monitor for signs of hyperemia: 'ventriculization' and disappearance of the dicrotic notch in the distal pressure waveform, separation of the aortic and distal pressure waveforms, and symptoms (chest discomfort, dyspnea). Changes in heart rate and blood pressure are less reliable indicators of hyperemia.
- If the initial adenosine infusion fails to achieve steady-state hyperemia, consider increasing the rate to 210 µg/kg/min.
- Document FFR at stable hyperemia. An FFR reading of ≤0.80 is taken as significant for flow-limiting epicardial disease.
- With the adenosine infusion still running, switch the linked diagnostic software to complete the hyperemic thermodilution measurements.
- Repeat rapid 3 mL boluses of room-temperature normal saline via the guide catheter to record hyperemic thermodilution transit times.
- Perform the same data quality assurance checks as for the resting readings. Replace any artefactual or outlier data.
- Stop the IV adenosine infusion. The total duration of adenosine infusion will be approximately 2-3 minutes.
- Review data recordings to ensure the software-selected readings are free from artefact. Manual fine-tuning may be required. CFR <2.0 ('grey zone' 2.0-2.5), IMR ≥25 and RRR <2.0 are indicative of coronary microvascular dysfunction.
3. Pharmacological reactivity test
- Keep the pre-prepared acetylcholine from pharmacy at 4 °C in the catheterization laboratory until use. Product shelf life is 30 hours from manufacture. The expiry date/time should be detailed on the label. Acetylcholine will be prepared at three doses:
Solution 1 Acetylcholine Chloride 0.182 µg/mL (10-6M)
Solution 2 Acetylcholine Chloride 1.82 µg /mL (10-5M)
Solution 3 Acetylcholine Chloride 18.2 µg /mL (10-4M) - Choose an angiographic projection that allows visualization of the coronary artery with minimal foreshortening and overlap. Acquire a resting angiogram.
- Check that the guide catheter is still co-axially intubated for the acetylcholine infusion.
NOTE: If choosing to infuse using a dedicated intracoronary microcatheter, position at this stage with the aid of a coronary guidewire. We advocate direct infusion via the guide catheter to minimize coronary instrumentation and procedural cost. - Connect a long, sterile IV line to a 3-way tap and flush the system with normal saline. Connect the sterile IV line to the acetylcholine syringe which will be administered using an automated infusion pump.
CAUTION: Acetylcholine can temporarily interrupt cardiac conduction. Keep atropine 1 mg and alternative means of pacing available. This is more relevant for dominant coronary arteries. Coughing is effective for heart rate recovery. Inform the patient that this may be needed. - Connect Solution 1 (60 mL syringe; 10-6M).
- Purge the IV line and guide catheter with 4 mL of acetylcholine solution to minimize any 'dead space' effect when the infusion is commenced.
- With the guide catheter still co-axial, commence the infusion at 2 mL/min for 2 minutes.
- Have the cardiac catheterization laboratory physiologist start the digital stopwatch on the monitor to ensure accurate time keeping.
- Monitor the patient, vital signs and ECG for effects of acetylcholine. If encountering any safety concerns, stop the acetylcholine infusion immediately.
- After the 2 minute infusion is complete, acquire an ECG and assess the patient for symptoms.
- Gently purge the guide catheter system with contrast to avoid a sudden bolus of acetylcholine with next contrast injection.
- Repeat the coronary angiogram in the same projection as at rest. This should be sufficiently long to assess myocardial blush and TIMI frame counts, i.e., >3 heart beats.
- Connect Solution 2 (60 mL syringe; 10-5 M).
- Purge the IV line and guide catheter with 4 mL of acetylcholine solution to minimize any 'dead space' effect when the infusion is commenced.
- With the guide catheter still co-axial, commence the infusion at 2 mL/min for 2 minutes.
- Have the cardiac catheterization laboratory physiologist start the digital stopwatch on the monitor to ensure accurate time keeping.
- Monitor the patient, vital signs and ECG for effects of acetylcholine. If encountering any safety concerns, stop the acetylcholine infusion immediately.
- After the 2 minute infusion is complete, acquire an ECG and assess the patient for symptoms.
- Gently purge the guide catheter system with contrast to avoid a sudden bolus of acetylcholine with next contrast injection.
- Repeat the coronary angiogram in the same projection as at rest. This should be sufficiently long to assess myocardial blush and TIMI frame counts, i.e., >3 heart beats.
- Connect Solution 3 (60 mL syringe; 10-4M).
- Purge the IV line and guide catheter with 4 mL of acetylcholine solution to minimize any 'dead space' effect when the infusion is commenced.
- With the guide catheter still co-axial, commence the infusion at 2 mL/min for 2 minutes.
- Have the cardiac catheterization laboratory physiologist start the digital stopwatch on the monitor to ensure accurate time keeping.
- Monitor the patient, vital signs and ECG for effects of acetylcholine. If encountering any safety concerns, stop the acetylcholine infusion immediately.
- After the 2 minute infusion is complete, acquire an ECG and assess the patient for symptoms.
- Gently purge the guide catheter system with contrast to avoid a sudden bolus of acetylcholine with next contrast injection.
- Repeat the coronary angiogram in the same projection as at rest. This should be sufficiently long to assess myocardial blush and TIMI frame counts, i.e., >3 heart beats.
- Manual administration (bolus) of acetylcholine. The dose is usually 100 µg (5.5 mL of Solution 3) into a left coronary artery. This should be halved if infusing into a dominant coronary artery.
- With the guide catheter still co-axial, commence manual infusion of the desired dose over 20 seconds.
- Have the cardiac catheterization laboratory physiologist start the digital stopwatch on the monitor to ensure accurate time keeping.
- Monitor the patient, vital signs and ECG for effects of acetylcholine. If encountering any safety concerns, stop the acetylcholine infusion immediately.
- After the infusion is complete, acquire an ECG and assess the patient for symptoms.
- Gently purge the guide catheter system with contrast to avoid a sudden bolus of acetylcholine with next contrast injection.
- Repeat the coronary angiogram in the same projection as at rest. This should be sufficiently long to assess myocardial blush and TIMI frame counts, i.e., >3 heart beats.
- Administer 300 mcg of intracoronary GTN and allow 30 seconds to take effect.
- Acquire an ECG and assess the patient for symptoms.
- Repeat the coronary angiogram in the same projection as at rest. This should be sufficiently long to assess myocardial blush and TIMI frame counts, i.e., >3 heart beats.
- Finally, perform a 'pullback' of the diagnostic guidewire and ensure 'signal drift' ≤0.03. Consider a final angiogram to exclude distal guidewire injury.
4. Multivessel assessment
- Coronary function may vary between different coronary territories. The variation reflects differences in heart muscle mass subtended by individual coronary arteries, as well as disease (e.g., fibrosis). Therefore, while the IDP is usually performed in a single coronary artery, repeat testing or investigation of additional coronary arteries may be undertaken as felt to be clinically appropriate. A typical scenario would be when the initial test results are normal despite a strong clinical history; hence, assessing a second artery would be intended to avoid a false negative result. Similarly, vasospasm may vary between coronary arteries, so multi-vessel pharmacological testing may be considered if a high index of suspicion persists despite an initial negative response.
Representative Results
The ultimate goal of the IDP is to be able to differentiate patients according to their respective clinical endotypes and institute appropriate management. The main endotypes to consider are: microvascular angina, vasospastic angina, mixed (both), or non-cardiac symptoms. The individual endotypes and diagnostic criteria are summarized in Table 1. Figure 1 further illustrates how these criteria are applied at each step of the IDP, with examples of abnormal results.
Diagnostic guidewire test
The diagnostic guidewire test measures parameters of coronary flow limitation (fractional flow reserve [FFR], coronary flow reserve [CFR], microvascular resistance [index of microvascular resistance (IMR)], basal resistance index, and vasodilator function [CFR, resistive reserve ratio (RRR)]). Abnormal results are defined below:
FFR ≤0.80 is indicative of obstructive epicardial disease.
CFR <2.0 (2.0-2.5 = 'grey zone') in the absence of obstructive epicardial disease is indicative of microvascular angina.
IMR ≥25 is indicative of microvascular angina.
RRR<2.0 is indicative of microvascular angina.
Acetylcholine provocation test
A clinical response is reflected by concomitant symptoms (i.e., chest pain), changes on the ECG (i.e., ST-segment deviation) and/or angiogram (Figure 1). Abnormalities on the coronary angiogram include: reduction in coronary artery diameter when assessed visually or measured by quantitative coronary analysis (QCA), transient impairment in antegrade coronary flow (TIMI flow), and a reduced myocardial blush.
Vasospastic angina symptoms typically occur at rest, may exhibit marked diurnal variation, and may be precipitated by hyperventilation19. The European Association of Percutaneous Cardiovascular Interventions (EAPCI)9 and Japanese Circulation Society (JCS)19 have proposed standardized criteria for the diagnosis of vasospastic angina. These are summarized in Table 1. Recognition of vasospastic angina is important due to its associated increased risk of myocardial infarction19.
Vasospastic angina is diagnosed when there is ≥90% reduction in coronary luminal diameter, along with reproduction of anginal symptoms and ischemic ECG changes.
Microvascular spasm is diagnosed with the reproduction of angina, ST-segment deviation, <90% change in epicardial lumen diameter, and/or TIMI flow reduction.
Table 1: Diagnostic criteria for each endotype (disease sub-group). Please click here to download this Table.
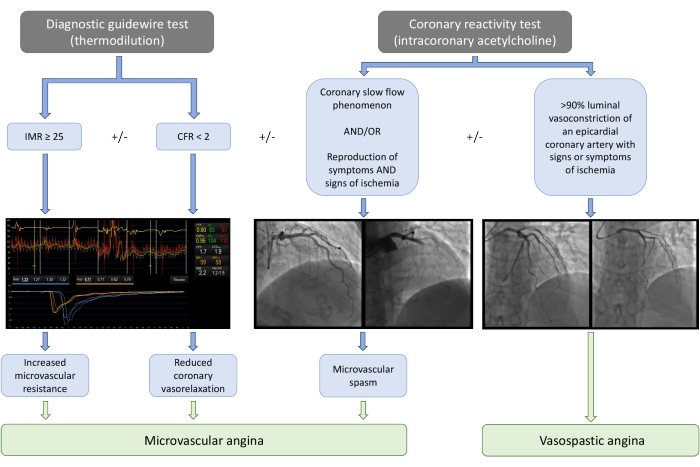
Figure 1: Summary flow-chart for interpretation of IDP results, with illustrative examples. IMR, index of microvascular resistance; CFR, coronary flow reserve. Please click here to view a larger version of this figure.
Discussion
Nitrate administration after radial artery cannulation reduces the propensity towards peripheral vasospasm that might hamper catheter manipulation. Intracoronary nitrates prior to diagnostic guidewire testing serves to negate any confounding epicardial spasm. Bearing the subsequent pharmacological provocation test in mind, only short-acting nitrates (e.g., GTN) are used. With a short half-life of approximately 2 minutes, the majority of this drug is metabolized prior to the later commencement of acetylcholine infusion20. In our experience, this has not led to false negative pharmacological test results.
Guide catheter choice should be personalized to achieve the best balance between support and patient tolerability. The benefits of good catheter support include: reduced variation in volume delivered from each saline bolus, reduced risk of vessel injury due to less recoil of the catheter during rapid saline injections, and reduced transit time variability by stabilizing the diagnostic guidewire position within the vessel. 'Balloon-tracking', or alternatively 'catheter-assisted tracking' by advancing a 5 Fr diagnostic pigtail catheter within a 6 Fr guide, can help overcome issues with shearing injury and radial spasm6.
Provision of a dedicated 3 mL syringe may assist with thermodilution injections. When inspecting results for artefact and outliers, a ≤10% (or ≤0.1 s) variation between thermodilution transit times represent good consistency. Thermodilution deflection waveforms should be of similar shape and overlap.
If significant signal drift repeatedly occurs during measurement, check that all elements within the catheter and manifold system are secure. 'Pressure bleed' can occur from loose connections to the pressure transducer.
Acknowledgements
The authors are grateful to the patients, colleagues and institutions that have contributed to the body of knowledge in this field. No specific funding was received for this work.
Materials
| Name | Company | Catalog Number | Comments |
| Coroflow software | Coroventis | N/A | https://www.coroventis.com/coroflow/measurements-indepth/ |
| Miochol-E, 20 mg, Powder and Solvent for instillation solution for intraocular use. | Bausch & Lomb U.K Limited | Unlicensed for parenteral use | https://www.medicines.org.uk/emc/product/4795/smpc#gref |
| PressureWire Receiver | Abbott Vascular | C17040 | https://www.cardiovascular.abbott/us/en/hcp/products/percutaneous-coronary-intervention/pressurewireX-guidewires-physiology/ht-tab/ordering-info.html |
| PressureWire X Guidewire, 175 cm | Abbott Vascular | C12059 | https://www.cardiovascular.abbott/us/en/hcp/products/percutaneous-coronary-intervention/pressurewireX-guidewires-physiology/ht-tab/ordering-info.html |
References
- Patel, M. R., et al. Low Diagnostic Yield of Elective Coronary Angiography. Engl J Med. 362 (10), 886-895 (2010).
- Ford, T. J., Corcoran, D., Berry, C. Stable coronary syndromes: Pathophysiology, diagnostic advances and therapeutic need. Heart. 104 (4), 284-292 (2018).
- Tavella, R., Cutri, N., Tucker, G., Adams, R., Spertus, J., Beltrame, J. F. Natural history of patients with insignificant coronary artery disease. European Heart Journal - Quality of Care and Clinical Outcomes. 2 (2), 117-124 (2016).
- Maddox, T. M., et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA - Journal of the American Medical Association. 312 (17), 1754-1763 (2014).
- Jespersen, L., et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. European Heart Journal. 33 (6), 734-744 (2012).
- Ang, D. T. Y., Berry, C. What an Interventionalist Needs to Know About INOCA. Interventional Cardiology: Reviews, Research, Resources. 16, (2021).
- Ong, P., et al. International standardization of diagnostic criteria for microvascular angina. International Journal of Cardiology. 250, 16-20 (2018).
- Neumann, F. J., et al. ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal. 41 (3), 407-477 (2020).
- Kunadian, V., et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International. European heart journal. 41 (37), 3504-3520 (2020).
- . Stratified medicine methodology framework - Research - Medical Research Council Available from: https://mrc.ukri.org/research/initiatives/precision-medicine/stratified-medicine-methodology-framework/ (2018)
- Ford, T. J., et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. Journal of the American College of Cardiology. 72 (23), 2841-2855 (2018).
- Ford, T. J., et al. 1-Year Outcomes of Angina Management Guided by Invasive Coronary Function Testing (CorMicA). JACC: Cardiovascular Interventions. 13 (1), 33-45 (2020).
- Williams, R. P., et al. Doppler Versus Thermodilution-Derived Coronary Microvascular Resistance to Predict Coronary Microvascular Dysfunction in Patients With Acute Myocardial Infarction or Stable Angina Pectoris. The American Journal of Cardiology. 121, 1-8 (2017).
- Okumura, K., et al. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. Journal of the American College of Cardiology. 12 (4), 883-888 (1988).
- Sueda, S., et al. complications during spasm provocation tests with an intracoronary injection of acetylcholine. The American journal of cardiology. 85 (3), 391-394 (2000).
- Stygall, J., Kong, R., Walker, J. M., Hardman, S. M. C., Harrison, M. J. G., Newman, S. P. Cerebral Microembolism Detected by Transcranial Doppler During Cardiac Procedures. Stroke. 31 (10), 2508-2510 (2000).
- Ford, T. J., et al. Rationale and design of the British Heart Foundation (BHF) Coronary Microvascular Angina (CorMicA) stratified medicine clinical trial. American Heart Journal. 201, 86-94 (2018).
- Sidik, N. P., et al. Rationale and design of the British Heart Foundation (BHF) Coronary Microvascular Function and CT Coronary Angiogram (CorCTCA) study. American Heart Journal. 221, 48 (2020).
- Japanese Circulation Society. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circulation journal: official journal of the Japanese Circulation Society. 78 (11), 2779-2801 (2014).
- . Glyceryl Trinitrate 5 mg/ml Sterile Concentrate - Summary of Product Characteristics (SmPC) - (etc) Available from: https://www.medicines.org.uk/emc/product/3792/smpc#gref (2022)
This article has been published
Video Coming Soon
ABOUT JoVE
Copyright © 2024 MyJoVE Corporation. All rights reserved