The Microscopic Transcanal Approach in Stapes Surgery Revisited
In This Article
Summary
This article describes the microscopic transcanal technique for stapes surgery, providing step-by-step surgical instructions for familiarizing surgeons with this approach.
Abstract
The microscopic transcanal (aka transmeatal) surgical approach was first described in the 60s, offering a minimally invasive means of reaching the external auditory canal, the middle ear, and epitympanon. Such an approach avoids a retroauricular or endaural skin incision; however, working through a narrow space needs angled microsurgical instruments and specific training in otologic surgery. The transcanal approach restricts the working space; however, it offers a binocular microscopic vision into the middle ear without extended skin incisions and thus, reducing post-operative pain and bleeding. In addition, this minimally invasive approach avoids scar tissue complications, hypoesthesia of the auricle, and potential protrusion of the pinna. Despite its numerous advantages, this method is still not routinely performed by otologic surgeons. Since this minimally invasive technique is more challenging, there is a need for extensive training in order for it to be widely adopted by otologic surgeons. This article provides step-by-step surgical instructions for stapes surgery and reports possible indications, pitfalls, and limitations using this microscopic transcanal technique.
Introduction
The advent of a binocular operating microscope in otologic surgery in 19511 paved the way for a less invasive microscopic transcanal approach. Alternatives were endaural incisions or retroauricular approaches, which are more invasive. The first transcanal stapes surgery was described by Rosen already in 19522,3, but at that time, the stapes was mobilized and not removed. In 1956, Shea revolutionized stapes surgery with the use of the first Teflon prosthesis4. The transcanal approach proved suitably adapted to this technique since it provided good 3D visualization of the posterior part of the ear canal, tympanic membrane, and middle ear. The indication for a transcanal microscopic method has widened over time, covering a large number of surgical otologic interventions: Tympanotomy5, tympanoplasty6,7,8, ossiculoplasty9, antrotomy10, cholesteatoma11,12,13, glomus tympanicum14, labyrinthectomy15, neurectomy16,17, intrameatal acoustic neuroma by transpromontory approach18,19,20 or even cochlea implantation21.
This challenging approach requires the use of specialized instrumentation for transcanal surgery (initially described in the 60s)22 and specific surgical training. It restricts working space but does, however, offer a binocular microscopic vision into the middle ear without the need for an extended skin incision and thus, reduces post-operative pain and bleeding. In addition, this minimally invasive approach avoids scar tissue complications, hypoesthesia of the auricle, and protrusion of the pinna. In this article, we provide step-by-step surgical instructions for stapes surgery and report possible indications, pitfalls, and limitations using this microscopic transcanal technique.
Protocol
The local review board of the Bern University (Kantonale Ethikkomission Bern) approved the present study, a formal informed consent was not required for this type of retrospective study.
1. Indications
- Use the transcanal approach if the diameter of the ear canal is ≥5.5 mm.
NOTE: The anatomy and shape of the outer ear canal might further limit the working space. - Assess the canal's diameter by placing a 5 mm diameter ear speculum. Ensure that the speculum sits comfortably in the canal.
- Do not use the transcanal approach in anterior perforations with a non-visible anterior rim.
- Use the inside-out-technique11 for middle ear pathologies such as cholesteatomas, which reach the epitympanon beyond the semicircular canal.
2. Preparation
- Positioning of the patient: Place the operating table at the lowest position, tilted in a reverse Trendelenburg position (Figure 1A) with the angle (α) of the headrest at its maximal reclination (without head hanging).
NOTE: This position is contraindicated in patients with atlantoaxial instability. Finally, rotate the head towards the contralateral side (β, Figure 1B). - Instruments: Use bent instruments to keep the working field open. Hold the instruments correctly with the fingers, thus preventing any blocked vision (Figure 2 and Figure 3).
NOTE: Black-colored instruments reduce light reflections. - Disinfection and cleaning of the ear canal: Clean the ear canal thoroughly to avoid any intraoperative infection. Disinfect the canal with diluted Povidone Iodine (2.5%-5% due to toxicity).
3. Local anesthesia
- Perform local anesthesia in two steps:
- Inject all four quadrants (23 G needle) with Carbostesin 0.25% (50 mg/20 mL) mixed with Adrenalin 1 mg/mL (final concentration 1:200,000 epinephrine).
- Inject within the ear canal using a small bent 27 G needle. Be careful when injecting in the anterior-inferior area to avoid facial paresis.
4. Tympanomeatal flap and speculum holder
- Perform a tympanomeatal flap using a u-shape incision with a sickle or a round knife starting at 6' o clock position (inferio-anterior). Detach the ear canal skin with a Rosen knife until the inferior annulus rim is reached.
- Install the speculum holder (Figure 4).
- Insert the largest possible ear speculum. Make sure that the orientation is correct.
NOTE: Letters indicating the size of the speculum should be placed superiorly. - Complete the tympanomeatal u-shaped flap by cutting the superior-posterior part with the Belucci scissor. Detach the ear canal skin with a Rosen knife until the superior annulus rim is reached.
- This step might cause bleeding.
- Use an absorbable gelatin sponge soaked with adrenaline to stop bleeding.
- Detach the whole flap until the edge of the annulus.
5. Middle ear dissection
- Make sure that facial nerve monitoring is working before entering the middle ear.
NOTE: The patient should have recovered from any neuromuscular block, which can be assessed by neuromuscular monitoring (4 TOF, train of four). - Enter the middle ear at the posterior-superior part of the annulus since it is easier to detach at this position.
NOTE: Large cholesteatomas or granulation tissue around the middle ear ossicles might hide any anatomical landmark. In this case, inferio-posterior entering of the middle ear might be advised to find other landmarks (CAVE: jugular bulb). - Dissect and visualize the anatomical middle ear structures. Visualize the chorda tympani, promontory, incudostapedial joint, stapedial tendon, and the facial nerve (tympanic segment).
- Widen the posterior-superior part of the ear canal with a bone curette or a 2 mm rough diamond drill (low speed) if any of the above structures are not sufficiently exposed. Put an absorbable gelatin sponge in the middle ear to prevent the entrance of bone dust into the middle ear.
6. Stapes suprastructure removal
- Disconnect the incudostapedial joint with a small 0.3-0.6 mm hook or a sickle knife and make an anterior movement to prevent breaking of the footplate.
- Test the mobility of all the three ossicles by touching each ossicle with a needle to confirm isolated ankylosis of the stapes.
- Use protection glasses or filters integrated into the microscope.
- Dissect the stapedial tendon with the laser (e.g., diode laser, CO2-Laser). Test the strength of the laser during this procedure. Use a FOX laser with 2.5-3 W energy in pulse mode (30-50 ms); however, this value depends on the device and its probe.
- Dissect the posterior crus of stapes near the attachment of the footplate ± anterior crus if the footplate is too mobile.
- Remove the stapes suprastructure. Brake the stapes away from the facial nerve towards the promontory if the anterior crus is still intact. Keep the footplate intact.
NOTE: The footplate should not move while breaking the suprastructure. There is a risk of a longitudinal fracture of the footplate during this procedure.
7. Footplate perforation
- Use the FOX laser to carbonize/weaken the footplate (2 W, 30 ms pulse mode) by making a rosette pattern.
- Use a perforator microdrill (skeeter 0.6 mm) to perforate the last shell of the footplate in the posterior third section.
- If the footplate is too thick, use a diamond microdrill to thin out the footplate until a blue shimmering structure is visible (also known as blue lining).
- Do not use the suction in the area of the footplate once the footplate is open.
8. Stapes prosthesis insertion
- Measure the distance between the long process of the incus and the footplate using a measurement instrument with a 4 mm measuring mark. Use a 0.25 mm longer prosthesis than measured.
- Hold the prosthesis hook with a small alligator ear forceps using a predefined angle of orientation (~20°) prior to insertion.
- Crimp the stapes hook on the long process of the incus.
NOTE: The front tine of the crimping instrument moves while the back tine remains stable on the incus. - Check the movement of the prosthesis by moving the malleus handle.
- Avoid the prosthesis from touching the promontory or the facial nerve.
- Consider using otologic cement if there is an interplay between prosthesis and incus process.
- Avoid over-crimping since there is a risk for incus necrosis in the long term.
- Seal the perforated footplate with small water-soaked absorbable gelatin sponge.
9. Wound closure/dressing
- Reposition the tympanomeatal flap, adapt with silk dressing, and pack with absorbable gelatin sponge soaked with a solution of hydrocortisone 10 mg (1%)/neomycin 3.5 mg/polymyxin B sulfates 10,000 Units.
- Use a 10 cm ribbon gauze soaked with the same solution for ear canal packing.
Representative Results
We present here a retrospective cross-sectional analysis (01/2018 to 05/2021) from 66 patients (37 males, 29 females) aged 9-68 years (mean 46.3y, SD ±13.4y), who underwent stapes surgery (48 standard surgeries, 18 revisions, Table 1 and Table 2). All patients were operated by the same surgeon (GM). The instruments were bent and black (Figure 3). The mean speculum size was 6.1 mm (range 5-8 mm, n = 51, Figure 2) which allowed an adequate visualization of the operating field. Only 1 out 66 cases needed a retroauricular incision (9 years old child with a canal diameter <5 mm). A posterior canaloplasty was necessary for 37 of 66 patients. Figure 2 illustrate how to hold the bent instruments with the first three fingertips while stabilizing the hand on the speculum or head of the patient with the remaining two fingers. A speculum holder consists of a mobile extension mounted on the operation table (Figure 4). Light exposure is limited and needs to be adjusted by the position of the microscope and the angled instruments (Figure 5). The ergonometric position of the sitting surgeon and optimized angle of the hands (Figure 6) allow a stable microsurgical performance. Fifty-eight patients received a Richards' piston prosthesis, one patient a Matrix Slim Line KURZ prosthesis, and five patients a malleo-vestibulo-pexy (MVP) prosthesis (ball joint prosthesis). The mean size of the prosthesis was 4.4 mm (range 4-5 mm, SD ± 0.2 mm), mean diameter was 0.46 mm (range 0.4-0.6 mm, SD ± 0.08 mm, Table 1). The prosthesis was additionally fixed with otologic cement in 33 of 66 cases. The Chorda tympani was preserved in 55 out of 65 cases.

Figure 1: Positioning of the patient. (A) The operation table at the lowest position tilted in the reverse Trendelenburg position. (B) The head/body rotation in a side-lying position towards the healthy ear. Please click here to view a larger version of this figure.
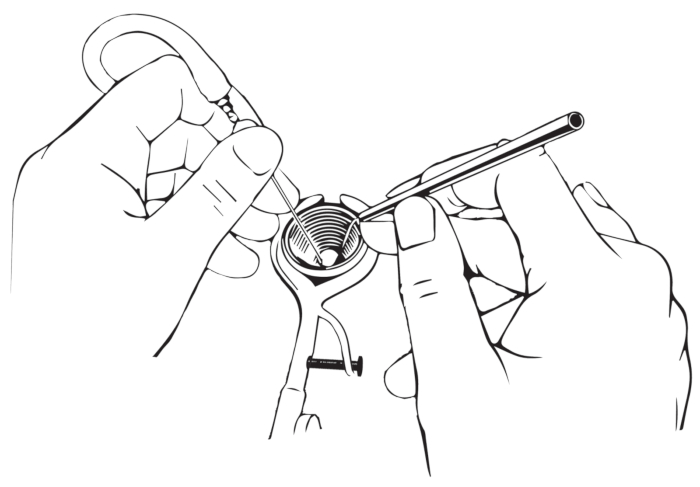
Figure 2: How to hold the instruments. The instruments must be held like a pencil; the ring finger should be supported at the edge of the speculum. Please click here to view a larger version of this figure.

Figure 3: Bent instruments for transcanal microscopic approach. The figure illustrates bent instruments such as a hook, a suction, or an ear speculum (from left to right). Please click here to view a larger version of this figure.
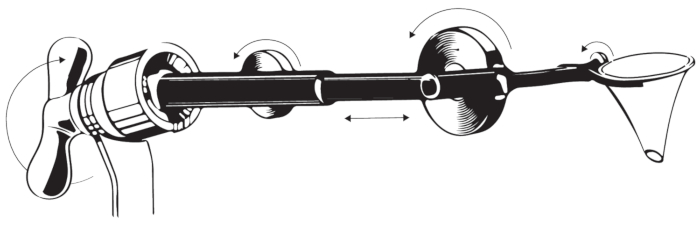
Figure 4: Ear speculum holder. The figure illustrates the design of the speculum holder. Please click here to view a larger version of this figure.
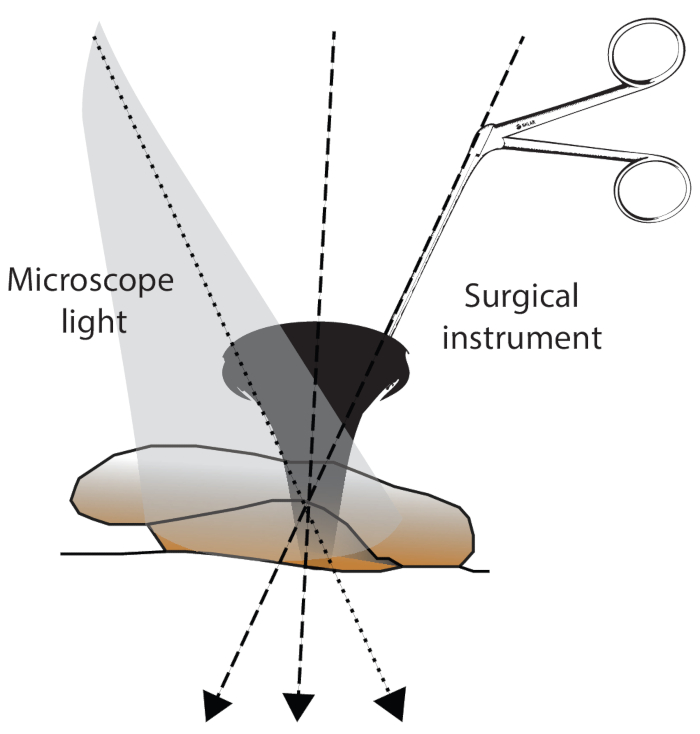
Figure 5: Surgical field exposure. The exposure of the surgical field can be influenced by 1) the angle of the microscope light, 2) the angle of the introduced instrument, and 3) the angle of the ear canal/head position. Please click here to view a larger version of this figure.
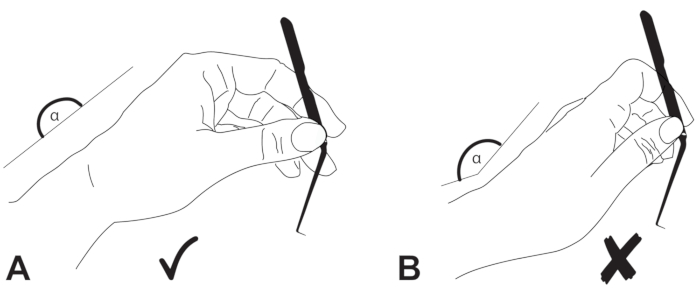
Figure 6: Positioning of the hands. The wrist of the surgeon should be in (A) neutral position and (B) not extended. Please click here to view a larger version of this figure.
Table 1: Summary of the study. The table summarizes the patient and operation characteristics Please click here to download this Table.
Table 2: Patient and operation characteristics. The table shows individual patient details and operation characteristics. Please click here to download this Table.
Discussion
The current article provides detailed insider information about the transcanal microscopic approach for stapes surgery. We could demonstrate that microsurgery is feasible using a key-hole technique avoiding a retroauricular or endaural incision in the majority of cases.
Some prerequisites, however, have to be met for achieving a successful surgery. The dissectors should be curved. The knives, hooks, and the needle are angled (Figure 1) to improve the visualization and light conditions in such a narrow space22. In addition, instruments should be black-colored, avoiding any microscopic light reflections. Patient positioning is crucial for the transcanal approach since the ear canal is curved, and the light beam of the microscope must be fully aligned with the longitudinal axis of the canal (Figure 2). In addition, it is crucial to hold the instruments correctly (Figure 3) and to keep a suitable ergonomic posture of the hands (Figure 5) for a successful transcanal surgery.
A speculum holder, as shown in Figure 3, allows a two-handed technique and a straight access route to the tympanic membrane/middle ear. The speculum might additionally serve as an instrument guide. Finally, the angle of the fingers/instruments and the angle of the microscope light should be adjusted and optimized. In view of all these parameters, extensive training of transcanal otologic surgery is needed to improve surgical performance.
Alternative approaches include the endaural and retroauricular incision or the endoscopic transcanal approach. The retroauricular incision is advised for inaccessible anterior perforations of the tympanic membrane or subtotal perforations. Such cases, however, might still be accessible through endoscopic approach23, provided that the ear canal diameter is large enough (>5 mm). The retroauricular approach remains the gold standard if there is a need to open the mastoid cavity. For combined cholesteatoma surgeries (transmeatal and retroauricular transmastoidal approach), we recommend the inside-out technique, which was first described by Roth and Häusler11. This technique suggests as a first step a transcanal access to the middle ear identifying all anatomical structures following the extension of the disease (cholesteatoma) by epitympanectomy. As a second step, a retroauricular incision might follow in cases where transmastoidal access is indicated based on the extension of the cholesteatoma. There is a considerable advantage of this two-step approach since there is a non-negligible proportion of patients who will not need a retroauricular incision (second step) based on a limited extension of the disease.
The transcanal endoscopic approach uses the same route of access and is also limited to an ear canal diameter of >5 mm. Similarly, this approach is minimal-invasive and offers a closer wide-angle view of anatomical structures. In addition, an endoscopic approach offers an angled view of 45° or 70°, which is valuable for the removal of cholesteatomas in the retrotympanum24, the attic region25 or for anterior perforations23. In cholesteatoma surgery, similarly to the above-mentioned inside-out technique, a transcanal endoscopic cholesteatoma removal is performed, followed by clearance of the disease from the mastoid as necessary. In this context, novel exclusive endoscopic techniques were recently described using a constant suction bone-drilling technique26. Endoscopic surgery, however, is a one-handed technique and challenging in inflamed conditions with associated bleeding. Therefore, the management of bleeding plays a key role in the endoscopic approach to the middle ear27. In addition, endoscopy provides a limited depth of field since it does not offer a binocular view. New 3D endoscopes might improve the depth of field28; however, such endoscopes have a larger diameter of 4 mm.
Compared to the retroauricular approach, the microscopic transcanal approach is minimal-invasive and has several advantages such as avoidance of retroauricular pain, scar tissue complications, hypoesthesia of the auricle, and protrusion of the ear.
The transcanal approach also has limitations. The main limitation is the diameter of the ear canal, which should be at least 5 mm. Any disease without direct or with limited access through the meatus is not suitable for a transcanal approach alone. The approach can be extended by using an endoscope or a combined transmastoidal access.
The transcanal/transmeatal microscopic approach has been a proven technique for more than 70 years; however, this method is still not routinely performed by otologists despite the advantages of this minimally invasive approach. Since the performance of this minimally invasive technique is more difficult and challenging, there is a need for extensive training in order to promote its use by otologic surgeons. This illustrative teaching video offers one additional tool to familiarize otologists with this surgical technique.
Disclosures
L.A. is a consultant for Stryker ENT. None of the other investigators has any relevant financial interests, activities, relationships, or affiliations that represent a relevant financial conflict of interest with respect to this work.
Acknowledgements
G.M. is supported by the Swiss National Science Foundation #320030_173081.
Materials
| Name | Company | Catalog Number | Comments |
| Adrenalin | Sintetica | ||
| Belucci microscissors | Olympus (former Richards) | 8178100FX | |
| Betadine solution (Povidon iodine) | Mundipharma Medical Company | ||
| Carbostesin | Sintetica | Bupivacain 2.5 mg/mL | |
| Cup forceps | Olympus (former Richards) | ||
| Curette | Olympus (former Richards) | 13-0147 | |
| Curved suction tubes | Spiggle & Theis | 302007NV und6066500100 | |
| Drill | Bienair | 2 mm rough diamond drill | |
| FOX laser | A.R.C. Laser GmbH | ||
| Gelfoam (absorbable gelatine compressed sponge) | Pfizer Injectables | GS-010DP | absorbable gelatin sponge |
| Gloves | Sempermed | Appropriate size | |
| Hooks | Olympus (former Richards) | 13-0201, 13-0202, 13-0204, 13-0206 | 0.3–0.6 mm |
| Hydrocortison/neomycin/polymyxin otic /Cortisporin Otic Solution | Pfizer | ||
| Needle | Olympus (former Richards) | 13-0207 | 27 G |
| Operating Microscope | Leica | E 114637 | |
| Otologic dissectors | Olympus (former Richards) | ||
| Ribbon gauze | |||
| Round knifes | Olympus (former Richards) | 13-0211 13-0212 | |
| Silk dressing | Otosilk | ||
| Speculum | Olympus (former Richards) | OK 082R | |
| Surgical Mask | Halyard | 48247 | |
| Water to rinse | Ringer |
References
- Mudry, A. The history of the microscope for use in ear surgery. Otology & Neurotology. 21 (6), 877-886 (2000).
- Rosen, S. The development of stapes surgery after five years: Mobilization-Fenestra Ovalis. AMA Archives of Otolaryngology. 67 (2), 129-141 (1958).
- Rosen, S., Bergmant, M. Improved hearing after mobilization of the stapes in otosclerotic deafness. The Journal of Laryngology & Otology. 69 (5), 297-308 (1955).
- Nazarian, R., McElveen, J. T., Eshraghi, A. A. History of otosclerosis and stapes surgery. Otolaryngologic Clinics of North America. 51 (2), 275-290 (2018).
- Jackson, M. Transmeatal tympanotomy. South African Medical Journal. 34, 983-984 (1960).
- Austin, D. F. Transcanal tympanoplasty. Otolaryngologic Clinics of North America. 5 (1), 127-143 (1972).
- de Savornin Lohman, E. A. J., Borgstein, J. Transmeatal tympanoplasty of subtotal and anterior perforations: a single-institution experience including 94 patients. Clinical Otolaryngology: Official Journal of ENT- UK; Official Journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 42 (4), 920-923 (2017).
- Seidman, M. D. Anterior transcanal tympanoplasty: A novel technique to repair anterior perforations. Otolaryngology-Head and Neck Surgery: Official Journal of American Academy of Otolaryngology- Head and Neck Surgery. 138 (2), 242-245 (2008).
- Aslan, A., Tanyeri Toker, G., Ozgur, E. Transcanal approach for Type 2 tympanoplasty with incus interposition ossiculoplasty: Our experience on 134 patients. Clinical Otolaryngology. 43 (4), 1135-1139 (2018).
- Holt, J. J. Transcanal antrotomy. Laryngoscope. 118 (11), 2036-2039 (2008).
- Roth, T. N., Haeusler, R. Inside-out technique cholesteatoma surgery: a retrospective long-term analysis of 604 operated ears between 1992 and 2006. Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Socient [and] European Academy of Otology and Neurotology. 30 (1), 59-63 (2009).
- Roth, T. N., Ziglinas, P., Haeusler, R., Caversaccio, M. D. Cholesteatoma surgery in children: long-term results of the inside-out technique. International Journal of Pediatric Otorhinolaryngology. 77 (5), 843-846 (2013).
- Shah, N. Cholesteatoma surgery; transcanal approach. Advances in Oto-Rhino-Laryngology. 29, 216-223 (1983).
- Cannon, S. J. Glomus tympanicum removal by transmeatal approach. Laryngoscope. 72, 193-200 (1962).
- Gacek, R. R. Transcanal labyrinthectomy. Laryngoscope. 88 (10), 1707-1708 (1978).
- Jones, R., Silverstein, H., Smouha, E. Long-term results of transmeatal cochleovestibular neurectomy: an analysis of 100 cases. Otolaryngology-Head and Neck Surgery: Official Journal of American Academy of Otolaryngology- Head and Neck Surgery. 100 (1), 22-29 (1989).
- Kos, M. I., et al. Transcanal approach to the singular nerve. Otology & Neurotology. 27 (4), 542-546 (2006).
- Isaacson, B., Tolisano, A. M., Patel, A. R., Barnett, S. L. Transcanal microscopic transpromontorial approach for vestibular schwannoma. Journal of Neurological Surgery, Part B: Skull Base. 80, 279-280 (2019).
- Mazzoni, A., et al. Transmeatal microsurgery for intralabyrinthine and intrameatal schwannomas: a reappraisal. Acta Otorhinolaryngologica Italica. 40 (5), 390-395 (2020).
- Presutti, L., et al. Expanded transcanal transpromontorial approach to the internal auditory canal: Pilot clinical experience. Laryngoscope. 127 (11), 2608-2614 (2017).
- Kiratzidis, T., Arnold, W., Iliades, T. Veria operation updated. I. The trans-canal wall cochlear implantation. ORL; Journal for Oto-Rhino-Laryngology and its Related Specialties. 64 (6), 406-412 (2002).
- Dworacek, H. Instruments for transmeatal middle ear surgery. AMA Archives of Otolaryngology. 70, 510-511 (1959).
- Tseng, C. C., Lai, M. T., Wu, C. C., Yuan, S. P., Ding, Y. F. Endoscopic transcanal myringoplasty for anterior perforations of the tympanic membrane. JAMA Otolaryngology-Head & Neck Surgery. 142 (11), 1088-1093 (2016).
- Bonali, M., et al. Correlation of radiologic versus endoscopic visualization of the middle ear: implications for endoscopic ear surgery. Otology & Neurotology. 41 (9), 1122-1127 (2020).
- Presutti, L., et al. The impact of the transcanal endoscopic approach and mastoid preservation on recurrence of primary acquired attic cholesteatoma. Otology & Neurotology. 39 (4), 445-450 (2018).
- Gao, Z., Jia, X. H., Yuan, Y. S. Endaural endoscopic atticoantrotomy (retrograde mastoidectomy) using a constant suction bone-drilling technique. Journal of Visualized Experiments: JoVE. (171), e62450 (2021).
- Anschuetz, L., et al. Management of bleeding in exclusive endoscopic ear surgery: Pilot clinical experience. Otolaryngology-Head and Neck Surgery. 157 (4), 700-706 (2017).
- Molinari, G., et al. Surgical implications of 3D vs 2D endoscopic ear surgery: a case-control study. European Archives of Oto-Rhino-Laryngology. 277 (12), 3323-3330 (2020).
This article has been published
Video Coming Soon
ABOUT JoVE
Copyright © 2025 MyJoVE Corporation. All rights reserved