Minimally Invasive Surgical Decompression of Occipital Nerves
In This Article
Summary
The manuscript presents a minimally invasive nerve and muscle-sparing surgical protocol to decompress occipital nerves aiming to improve occipital neuralgia.
Abstract
Occipital neuralgia (ON) stands out as one of the most distressing forms of headache disorders, distinguished by persistent pain at the base of the skull, recurring occipital headaches, and scalp dysesthesia or allodynia. ON is notorious for its unrelenting agony, severely impacting the lives of those afflicted. The incessant pain, often radiating upward from the base of the skull to the scalp, can be profoundly debilitating. Patients frequently endure excruciating occipital headaches, making even routine daily activities a formidable challenge. The added burden of scalp dysesthesia or allodynia, where seemingly innocuous stimuli elicit severe pain, compounds the suffering. This neuralgia primarily arises from the mechanical compression exerted on the occipital nerves along the nuchal line. In this paper, we present a minimally invasive nerve and muscle-preserving technique aimed at relieving this compression on the occipital nerves. Accurate diagnosis and effective treatment are paramount in providing relief for individuals battling this condition. Nerve blocks with local anesthesia have become a cornerstone of diagnosis, serving as both a confirmation of occipital neuralgia and a potential therapeutic intervention. These procedures offer crucial insights into the source of the pain while offering transient respite. However, the true breakthrough lies in the innovative technique we propose - a procedure that addresses the mechanical compression at the nuchal line, which is a prominent contributing factor to occipital neuralgia. By carefully decompressing the affected occipital nerves while preserving their integrity and surrounding muscle tissue, this minimally invasive approach offers patients a potential path to sustained relief. Remarkably, the procedure can be performed under local anesthesia, reducing the invasiveness of traditional surgeries and minimizing patient downtime.
Introduction
Occipital neuralgia (ON) is a chronic headache condition causing persistent dull pain in the back of the head1. The pain, which differs from typical migraines, is often resistant to standard migraine treatments due to mechanical compression on the occipital nerves2, particularly along their course through the nuchal line3. On the other hand, surgical options may be effective but involve invasive procedures and extended recovery times4,5. We present here a novel approach to the occipital nerves, allowing for minimally invasive decompression, minimal downtime, and preservation of muscle and sensitive nerve branches6.
Diagnosing ON relies on targeted nerve blocks, which temporarily reduce pain and help pinpoint the exact area of nerve compression7, guiding surgical decompression8,9. Unlike typical migraine management, our approach targets the root mechanical cause of ON, providing a viable therapeutic option beyond medication.
Numerous clinical and anatomical studies have led to the occipital nerve decompression technique as described in2,3,10,11,12,13. Although this technique has been proven safe and effective, the advantages of the minimally invasive technique presented here include reduced patient morbidity, abbreviated postoperative recovery periods, and lesser risks of iatrogenic-induced pain due to potential neuroma formation. In particular, the preservation of neural and muscular structures contributes to prompt and favorable outcomes. The greater and lesser occipital nerves can be exposed and decompressed via the described approach. For the purpose of this paper, only greater occipital nerve decompression is described to improve occipital neuralgia, which is due to lesser occipital neuralgia. The third occipital nerve is responsible for rare cases of occipital neuralgia in our practice, which are addressed with a separate approach due to its medial localization. The described technique includes the systematic exploration of the passage of the greater occipital nerve through the semispinalis capitis which may represent a compression point. Further research and clinical validation are warranted to ascertain the full scope of its efficacy and safety.
Protocol
The data collection was conducted as a retrospective quality assessment study and the analysis of the results was approved by the internal review board at University of Padua. All procedures were performed in accordance with the ethical standards of the national research committee and the 1964 Helsinki Declaration and its later amendments. All patients have signed an informed consent allowing the authors to anonymously use the retrospective data. For this study, 87 patients were included.
1. Selection of candidates
- Select patients based on a constellation of symptoms compatible with occipital neuralgia, including at least three of the following characteristics: aching, burning, and throbbing pain, starting in the pit between the insertion of the trapezius muscle and the sternocleidomastoid muscle (here defined as the occipital triangle); the pain travels in the scalp along the trajectory of the occipital nerves from the back of the head to the temples and front on one or both sides of the head; the pain can resemble an electrical shock; the pain can be elicited/worsened by particular positions of the head (hyperextension of the neck, rotation of the head, etc.) also while sleeping; the pain often is felt behind the eyes; the scalp can exhibit allodynia; patients may have migraines and cluster headaches in addition to occipital neuralgia.
- To be included, ensure patients respond with at least 50% decrease in pain after selective blocks of the occipital nerves.
- Use the following exclusion criteria: pain started after trauma like whiplash injury; pain started after surgery or radiotherapy with direct or indirect nerve injury; patients not responding to selective nerve blocks.
2. Nerve block procedure
- Prepare the infiltration mixture as 1.5 mL of 1% lidocaine with epinephrine (1% Rapidocain 10 mg/mL) and 1 cc of 40 mg Triamcinolone (40 mg/mL) in a 5 cc syringe prepared with a 30G needle.
- Transfer the mixture into a 5 mL syringe (Luer Lock) with a 30G needle (0.3 mm x 13 mm).
- Identify the site of injection by palpation. Identify the lateral edge of the proximal trapezius insertion and medial edge of the proximal sternocleidomastoid (SCM) muscle insertion, just below the nuchal line. The pit between these structures corresponds to the target injection point.
- Palpate the occipital artery passage above the nuchal line. Confirm the occipital neurovascular bundle (greater and lesser occipital nerve and occipital artery) position below the nuchal line using Doppler (10 MHz). Move the doppler probe caudally toward the occipital triangle and confirm the passage of the artery in this place by an arterial signal.
- Perform gentle aspiration with the syringe before injection (if blood is aspirated the needle is retracted a few mm) to prevent intravascular injection. If the patient feels electric shocks along the occipital nerve path, withdraw the needle a few mm to avoid intraneural injection and nerve damage.
- To ensure that the nerve block has been performed correctly, palpate the back scalp to allow the patient to confirm decreased sensation.
3. Preparation of the instrumentation table
- Drape the instrumentation table with laminar flow with sterile clothing. Prepare the following instruments: Surgical knife with blade No. 15, surgical Hudson forceps, needle holder, dissection scissors, bipolar forceps, lighted retractor, Nylon 5/0 suture, sterile gloves, Chlorhexidine disinfection, sterile paper tape.
4. Patient preparation
- Identify the most tender point with the patient sitting upright using palpation within the area where the nerve block was performed.
- Mark the incision site with a 2 to 3 cm oblique incision line across the tender area. Shave the area comprising the incision line and 1 cm around with a surgical shaver.
5. Surgeon preparation
- The surgeon wears 2.5x - 3.5x magnifying loops, surgical cap, and mask. Wash hands with soap and disinfect hands with antiseptic solution.
6. Surgical technique
- Patient positioning: Position the patients either laterally (in case of one-sided ON) or prone (for bilateral ON) on the surgical table.
- Local anesthesia: Administer local anesthesia, consisting of 5 mL of lidocaine with epinephrine, injected along the incision line via a 30G needle.
- Incision: Make an oblique, beveled incision, measuring 2.5 to 3.5 cm, centered in a region defined as the occipital triangle, bordered cranially by the nuchal line, medially by the lateral edge of the trapezius, and laterally by the medial edge of the sternocleidomastoid muscle using a No. 15 surgical blade.
- Nuchal line exposure: Incise the superficial layer of the nuchal line with the scalpel and dissect with dissection scissors to expose the greater occipital nerve (GON), occipital artery, and lymph nodes.
- Nerve exploration: Follow the GON meticulously along all points of possible compression using dissection scissors to create the space. Perform proximal release of the inferior fascia of the trapezius muscle with dissection scissors, semispinalis muscle fascia, and distal nuchal line fibers.
- Vascular and lymphatic structures: In instances where the occipital artery and lymph nodes come into contact with the nerves, reposition or excise these structures delicately with Hudson's surgical forceps. Gently disengage the adventitial and periarterial tissues with Hudson's surgical forceps, abundant in afferent and efferent autonomic nervous system fibers, in all cases (arteriolysis).
- Addressing neurovascular contact points: When a non-otherwise addressable conflict is found (such as a branch of the artery passing through the nerve fibers), divide this arterial segment (arteriotomy).
- Nerve blocks: Before closure, perform nerve blocks using 1% lidocaine with epinephrine sprayed directly on the nerve branches via a 30G needle. Ask the patient to move the head and talk to confirm complete decompression.
- Closure: Repair skin with single stitches of 5-0 nylon sutures. Dress the opening with moisture permeable spray dressing and sterile gauzes, held in place by paper tape.
7. Postoperative protocol
- Postoperative head movements: After the procedure, ask the patient to gently move the head in all directions at least 3x a day to prevent the formation of adhesions between the nerve fibers and the scar for a period of 2 to 3 weeks.
- Suture removal: Remove sutures 10 days after the procedure.
- Ask patients to continue their medications in case of headaches. Tell the patient to expect decreased sensation or anesthesia in the territory of the greater occipital nerve for a variable period between a few hours and a few days after the operation.
- Instruct patients to take ibuprofen 400-600 mg, 3x day for 3 days after the procedure.
Representative Results
At 1 year after the surgical decompression, there was a noteworthy reduction in chronic pain days, with a substantial decrease from an initial average of 25 days to 4.3 days (p <0.01), reflecting an 80.5% reduction (a 5.8-fold decrease) in chronic pain frequency (Figure 1)6. Furthermore, the number of pain crisis days per month exhibited a remarkable decline, plummeting from 19 days to 3.7 days (p <0.01), signifying an 82.8% reduction (a 5.1-fold decrease) in the frequency of pain crises (Figure 1 and Figure 2)6.
Patients reported an average background pain intensity of 3.7 on a scale of 10 before surgery, which substantially improved to 0.7 (p <0.01) post-surgery, corresponding to an impressive 76.1% reduction (a 5.2-fold decrease) in background pain intensity6. Moreover, the peak pain intensity experienced during crises significantly diminished from 8.8/10 to 2.1/10 after surgery (p <0.01), reflecting a substantial 81.1% reduction (a 4.2-fold decrease) in peak pain intensity (Figure 1 and Figure 2)6.
Remarkably, there was a significant reduction in the utilization of all types of drugs, including NSAIDs, triptans, and disease-modifying drugs, following the surgical intervention6 (not shown).
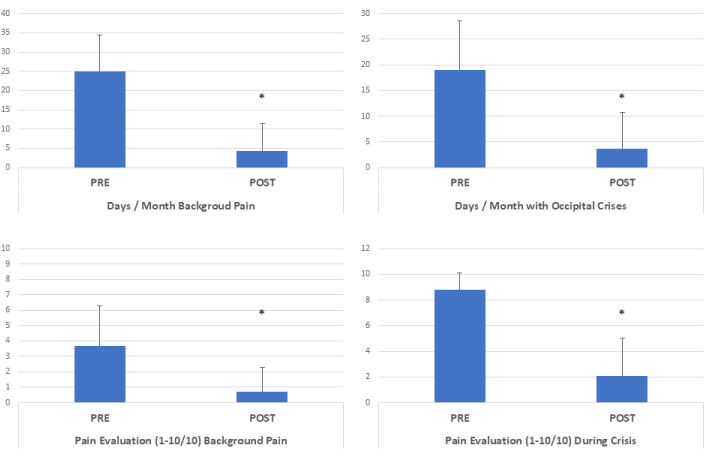
Figure 1: Clinical outcome after minimally invasive surgical decompression. After surgical decompression, chronic pain days decreased 5.8x. The pain crisis days/month decreased 5.1x. Background pain intensity decreased after surgery 5.2x, and pain intensity peaks during crises decreased 4.2x. (*p <0.01, Two-tailed paired t tests, n=87). This figure has been modified from6. Please click here to view a larger version of this figure.

Figure 2: Illustration of the anatomy of the occipital area pre- and post-decompression. In the pre-decompression picture, the external layer of the nuchal aponeurosis covers the occipital nerves and blood vessels. After decompression, the greater occipital nerve and occipital artery are visible. Please click here to view a larger version of this figure.
Discussion
Occipital neuralgia is one of the most debilitating forms of headaches, mainly due to the chronic pain that is unremitting. A study on the prevalence of facial pain in 2009, which is often used as a reference for occipital neuralgia, found an ON prevalence of 3.2 per 100,00014. These statistics largely underestimate the problem, knowing that ON is responsible for facial pain in only 8.3% of the cases and that up to 25% of the cases of emergency room admittance are for headaches due to occipital neuralgia15.
We find in our practice that ON alone or in combination with other migraines is one of the most prevalent forms of chronic headaches, possibly due to morbid posture with the neck in flexion in front of computers and smartphones several hours per day, sedentary lifestyle, and limited time outdoors.
The surgical approach outlined here offers a highly efficient means of accessing the occipital nerves under local anesthesia. Greater occipital neuralgia may coexist with lesser occipital neuralgia as these nerves have communicating branches and their territories overlap. By using the same surgical approach, both nerves can be explored and decompressed when indicated6. Patient acceptance of the procedure has been favorable, with an average duration of approximately 45 to 60 min required for completion per side.
The meticulous identification and preservation of nerve fibers constitute a hallmark of this approach. Thanks to the minimally invasive nature of the procedure that can be performed in local anesthesia, the operator assesses the efficacy of decompression at the end of the procedure by instructing the patient to engage in head movement and conversation, thereby ensuring the absence of residual compression points.
A crucial facet of this procedure lies in the emphasis on early and frequent head mobilization, conducted multiple times daily. This practice serves to deter the formation of adhesions between nerve fibers and the surgical scar, which may otherwise impede recovery.
It is essential to acknowledge that not all patients are suitable candidates for this technique. Notably, individuals with fragility or heightened anxiety levels may not tolerate the procedure comfortably under pure local anesthesia. In certain cases, patients may experience sudden discomfort, as even the slightest manipulation of an inflamed occipital nerve can trigger nerve firing. In these cases, local anesthesia is sprayed directly on the nerve fibers with immediate relief.
This surgical approach represents a less invasive alternative compared to previously proposed decompression techniques. Its capacity to spare both nerve and muscle fibers contributes to a notable reduction in complication rates. We posit that this minimally invasive, yet highly effective methodology will broaden the accessibility of surgical decompression as a definitive treatment option for occipital neuralgia, offering hope to a wider spectrum of patients.
Acknowledgements
The authors acknowledge the technical assistance of Alexandra Curchod, Yuliethe Martins, and the Filmatik Global team. This work was funded in its entirety by the Global Medical Institute.
Materials
| Name | Company | Catalog Number | Comments |
| 30G Needle | 0.3x13 mm, BD Microlance 3, Spain | ||
| Bipolar Forceps | McPerson, bipolar forceps, Erbe, Switzerland | 20195 | |
| Chlorhexidine | Hibidil, Chlorhexidini digluconas 0.5 mg/mL, Switzerland | 120099 | |
| dissection scissors | Jarit supercut, Integra Lifescience, USA | 323720 | |
| Doppler | Dopplex DMX Digital Doppler, High Sensitivity 10MHz probe, Huntleigh Healthcare, Wales, United Kingdom | ||
| Ethilon 5/0 Suture | Ethicon, USA | 698 G | |
| Lidocaine ephinephrine 1% | Rapidocain 1% 10 mg/mL, Sintetica, Switzerland | ||
| Lighted retractor | Electro Surgical Instrument Company, Rochester, NY | 08-0195 | |
| Magnifying loops | Design for vision, USA | ||
| Opsity spray | Smith & Nephew, USA | ||
| Sterile gloves | Sempermed sintegra IR, Ireland | ||
| Sterillium | Sterillium disinfectant, Switzerland | ||
| Surgical blade n.15 | Carbon steel surgical blades, Swann-Morton, England) | 205 | |
| Surgical drapes and gauzes | Halyard Universal pack, USA | 88761 | |
| Surgical instruments | Bontempi medical Italy | ||
| Surgical shaver | Carefusion, USA | ||
| Syringe 5cc | BBraun, Omnifix Luer Lock Solo, Switzerland | ||
| Triamcinolone 10mg | Triamcort depot 40 mg/mL, Zentiva Czech Republic |
References
- IHS. The international classification of headache disorders, 3rd edition. Cephalalgia. 38 (1), 1-211 (2018).
- Mosser, S. W., et al. The anatomy of the greater occipital nerve: implications for the etiology of migraine headaches. Plast Reconstr Surg. 113 (2), 693-697 (2004).
- Janis, J. E., et al. Neurovascular compression of the greater occipital nerve: implications for migraine headaches. Plast Reconstr Surg. 126 (6), 1996-2001 (2010).
- Guyuron, B., et al. Five-year outcome of surgical treatment of migraine headaches. Plast Reconstr Surg. 127 (2), 603-608 (2011).
- Blake, P., et al. Tracking patients with chronic occipital headache after occipital nerve decompression surgery: A case series. Cephalalgia. 39 (4), 556-563 (2019).
- Pietramaggiori, G., Scherer, S. Minimally invasive nerve- and muscle-sparing surgical decompression for occipital neuralgia. Plast Reconstr Surg. 151 (1), 169-177 (2023).
- Tobin, J., Flitman, S. Treatment of migraine with occipital nerve blocks using only corticosteroids. Headache. 51 (1), 155-159 (2011).
- Seyed Forootan, N. S., Lee, M., Guyuron, B. Migraine headache trigger site prevalence analysis of 2590 sites in 1010 patients. J Plast Reconstr Aesthet Surg. 70 (2), 152-158 (2017).
- Pietramaggiori, G., Scherer, S. . Minimally invasive surgery for chronic pain management. , (2020).
- Janis, J. E., et al. The anatomy of the greater occipital nerve: Part II. Compression point topography. Plast Reconstr Surg. 126 (5), 1563-1572 (2010).
- Ducic, I., Moriarty, M., Al-Attar, A. Anatomical variations of the occipital nerves: implications for the treatment of chronic headaches. Plast Reconstr Surg. 123 (3), 859-863 (2009).
- Junewicz, A., Katira, K., Guyuron, B. Intraoperative anatomical variations during greater occipital nerve decompression. J Plast Reconstr Aesthet Surg. 66 (10), 1340-1345 (2013).
- Scherer, S. S., et al. The greater occipital nerve and obliquus capitis inferior muscle: Anatomical interactions and implications for occipital pain syndromes. Plast Reconstr Surg. 144 (3), 730-736 (2019).
- Koopman, J. S., et al. Incidence of facial pain in the general population. Pain. 147 (1-3), 122-127 (2009).
- Mathew, P. G., et al. Prevalence of occipital neuralgia at a community hospital-based headache clinic. Neurol Clin Pract. 11 (1), 6-12 (2021).
This article has been published
Video Coming Soon
ABOUT JoVE
Copyright © 2024 MyJoVE Corporation. All rights reserved