Determination of Continuity Index Values in Atrial Fibrillation Ablation with Proactive Esophageal Cooling
In This Article
Summary
This protocol describes the methods used to determine the continuity index in patients undergoing pulmonary vein isolation procedures using radiofrequency ablation and demonstrates the differences in continuity index between ablation procedures using proactive esophageal cooling as compared to procedures using traditional luminal esophageal temperature monitoring.
Abstract
Radiofrequency (RF) ablation to perform pulmonary vein isolation (PVI) for the treatment of atrial fibrillation involves some risk to collateral structures, including the esophagus. Proactive esophageal cooling using a dedicated device has been granted marketing authorization by the Food and Drug Administration (FDA) to reduce the risk of ablation-related esophageal injury due to RF cardiac ablation procedures, and more recent data also suggest that esophageal cooling may contribute to improved long-term efficacy of treatment. A mechanistic underpinning explaining these findings exists through the quantification of lesion placement contiguity defined as the Continuity Index (CI). Kautzner et al. quantified the CI by the order of lesion placement, such that whenever a lesion is placed non-adjacent to the prior lesion, the CI is incremented by the number of segments the catheter tip has moved over.
To facilitate real-time calculation of the CI and encourage further adoption of this instrument, we propose a modification in which the placement of non-adjacent lesions increments the CI by only one unit, avoiding the need to count potentially nebulous markers of atrial segmentation. The objective of this protocol is to describe the methods of calculating the CI both prospectively during real-time PVI cases and retrospectively using recorded case data. A comparison of the results obtained between cases that utilized proactive esophageal cooling and cases that used luminal esophageal temperature (LET) monitoring is then provided.
Introduction
Pulmonary vein isolation (PVI) using radiofrequency (RF) catheter ablation has become one of the most common methods for restoring sinus rhythm in the rising number of atrial fibrillation (AF) cases worldwide1. Research has shown that indirect lesion quality markers, such as impedance decline, catheter-tissue contact force, catheter stability, and bipolar electrogram amplitude reduction serve as evidence of transmurality, which contributes to the effectiveness of PVI2. Despite these available markers, improving on successful isolation and ultimately, long-term freedom from arrhythmias remains a high priority for electrophysiologists. Clinical data have shown that the placement of adjacent, overlapping, and continuous lesions along the circumferential isolation line is associated with lower recurrence rates and a higher likelihood of achieving transmurality-associated unipolar electrogram (TUE)2,3.
Kautzner et al., in the EFFICAS II Study, developed the Continuity Index (CI) to quantify discontinuous lesion placement in efforts to further understand how the order of lesion placement during an ablation impacts both short and long-term efficacy (Figure 1)3. The CI refers to the number of positions the catheter tip has moved over to place subsequent lesions in non-adjacent positions after stopping RF power early due to local overheating. A higher CI implies more discontinuity in sequential lesion placement. This study suggested that a PVI with a low CI (CI < 6) resulted in a significant increase in successful isolation as a result of contiguous catheter movement allowing more effective electrical isolation compared to a CI ≥ 63. One possible mechanism for the observed decrease in long-term efficacy associated with a higher CI is the rapid edema formation that occurs around lesions, which has been thought to result in reversible PVI4,5. When subsequent lesions are delayed, rapid edema formation may prevent transmural or contiguous lesion formation at adjacent positions and may significantly alter or conceal local electrograms in the region of stunned tissue2,3. There exists a need to prevent esophageal thermal injury and potentially lethal atrioesophageal fistula (AEF) during PVI; however, the use of traditional luminal esophageal temperature (LET) monitoring often forces cessation of RF energy application as a result of local overheating detected in the esophagus6,7,8. This in turn causes the CI to increase significantly.
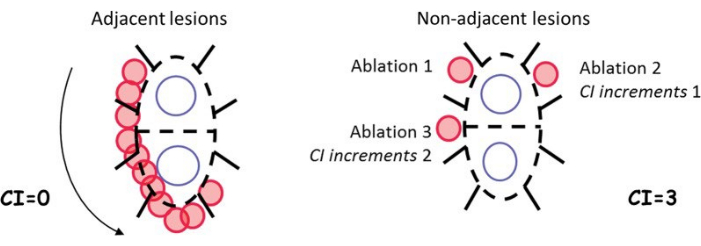
Figure 1: Example of continuity index calculation as originally defined for two examples of ablation patterns3. This figure was taken from Kautzner et al.3. Abbreviation: CI = continuity index. Please click here to view a larger version of this figure.
A proactive esophageal cooling device (see the Table of Materials) has been granted marketing authorization by the Food and Drug Administration (FDA) to reduce the likelihood of ablation-related esophageal injury resulting from radiofrequency cardiac ablation procedures, and data from over 25,000 patients suggest a significant reduction in AEF rate with cooling9. Long-term follow-up data also suggest improved freedom from arrhythmia when using cooling as opposed to LET monitoring10,11. The cooling device is a non-sterile, multi-lumen silicone tube placed in the esophagus, much like an orogastric tube, for the purpose of cooling or warming a patient. The tube acts as a heat sink for RF energy inadvertently delivered to the esophagus, thus minimizing esophageal tissue damage, while pericardial tissues prevent significant cooling of atrial tissue12. Device temperature is controlled by connecting the esophageal cooling device to an external heat exchanger that circulates distilled water within the device (Figure 2). The device can be placed by any provider cleared to place a standard orogastric tube (nurses, physicians, paramedics). For ablation procedures, the device is usually placed by the anesthesiologist or CRNA immediately following induction of anesthesia and intubation. Placement is confirmed by visualizing the radiopaque distal tip in the gastric space on fluoroscopy. The device can also be seen on intracardiac echocardiography (ICE) commonly used during ablations. During the procedure, the patient's temperature can be continuously measured by usual means (Foley, rectal, forehead, axillary, or tympanic membrane temperature probe), but not via esophageal probe. Recall that axillary temperature is typically 1.5° C lower than core temperature, and adding this to the axillary measurement is necessary to reflect patient core temperature13.
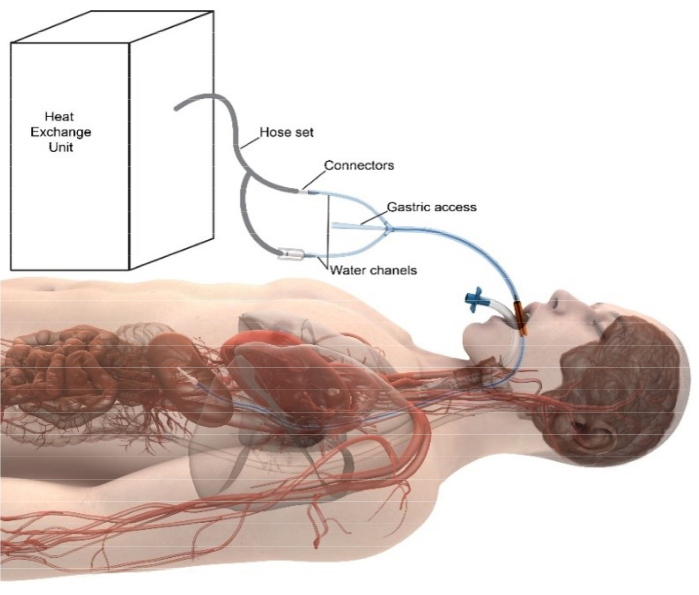
Figure 2: Diagram of the active esophageal temperature management system. The commercially available heat exchange unit generates temperature-controlled water, which is then delivered across standard tubing sets into the device placed in the esophagus. After circulating at a rate of ~1.5 L/min inside the device, the water returns to the heat exchange unit. The independent central lumen allows gastric decompression and suction. The radiopacity of the distal tip of the device allows for fluoroscopic visualization in the gastric space to confirm correct placement. Please click here to view a larger version of this figure.
Recent burn injury literature has found a strong association between cooling after thermal injury and a reduction in burn injury severity, with the mechanisms of this effect extending beyond dissipation of heat, to include the alteration of cellular behavior through (i) decreasing release of lactate and histamine, (ii) stabilizing thromboxane and prostaglandin levels, (iii) slowing local metabolism, (iv) altering membrane permeability, and (iv) inhibiting kallikrein activity14. The growing understanding of the local effects of hypothermia in burn injury provides a mechanistic underpinning for the significant safety benefit seen with the esophageal cooling device utilized in this study15. Proactive esophageal cooling allows for the contiguous placement of the sequential lesions without interruption and without the need to pause for local overheating conditions or temperature alarms, likely due to the mechanisms described above. This in turn decreases operator cognitive load, reduces procedure time, and allows a reduced CI which can increase long-term PVI success16,17.
Our aim in this protocol is to describe the methods of prospectively calculating a modified CI in real-time cases and describe the methods used to calculate a modified CI retrospectively in recorded cases. We then provide representative results for cases that utilized both real-time observations utilizing proactive esophageal cooling as well as retrospective data prior to the adoption of cooling. An advantage of this approach is that the CI can be measured easily both in real-time as well as retrospectively. By observing the CI in PVI cases with and without cooling, the impact of cooling on long-term efficacy and lesion continuity can be further quantified, and the use of the CI as a PVI quality measure can potentially be further promoted. Continuing research to explore CI and lesion quality in terms of RF ablation and clinical efficacy remains important, especially when pulsed field ablation appears to be associated with the risk of new adverse events without convincingly improving long-term outcomes 18.
Protocol
This research was reviewed and approved as exempt by the NorthShore University Health System Institutional Review Board.
1. Calculating CI for Prospective cases
- For live prospective cases, have a staff member monitor lesion placement in the control room by observing the order of lesions placed by the operator on the 3-D mapping software screen.
NOTE: Surpoint VISItag size may be set to a range of operator preference, for example, 2-3 mm. - Have the staff member quantify the CI in real time using the below-set parameters. Amplify lesion placement seen on the screen to confirm placement using the millimeter (mm) marker setting.
- Record a ZERO (0) increase in CI.
- Observe that the first lesion placed on each of the right or left veins does not increase CI.
- Lesions that overlap the previously placed lesion (as determined by the mapping software and visual determination) do not increase CI.
- A lesion that is placed that connects the path of continuous lesions to other lesions (such as closing the circle around the pulmonary veins) does not increase the CI.
- Do not increase the CI for lesions that are placed on top of the completed continuous line of lesions for extra burning/further isolation (touch-up lesions).
- Record a ONE (+1) increase in CI when a lesion is placed in a new location, not touching the previous lesion, for the vein on which the previous lesion was placed (this includes small gaps shown between VISItags).
- Record a TWO (+2) increase in CI when a new continuous set of lesions is placed in a new location, not touching any prior lesions, followed by another lesion placed to continue the previous line of lesions. Here, increase the CI by 1 for the area that is left the first time and 1 for moving away from the second area (possibly the same vein) (+1 for the initial discontinuity, +1 for the return).
- Record a ZERO (0) increase in CI.
- To do a summation of CI, have the staff member record in real time the discontinuity on each of the right and left pulmonary veins throughout the case and sum the CI (per vein and total) at the end of the case.
2. Calculating CI for Retrospective cases
- To access retrospective case files, install and open 3-D mapping software.
- Download past cases from the 3-D mapping system.Click on System | Study Archiver | Restore. Filter cases by selecting a range of dates using the dropdown menu in the From: and To: section at the top left of the screen.
EXAMPLE: From: 11 October 2018, To: 12 November 2018 - Type an asterisk * in either First Name, Last Name, OR Patient ID section at the top of the screen. Click on Query at the top right of the screen next to Patient ID.
- Select cases labeled as AF or Afib and click on the > button next to the list of cases on the screen to bring each selected case to the right side of the screen.
- Click on Restore to restore the data and access selected cases. Click on Exit | Ok when selected cases have been fully restored (will show as 100% restored on screen).
- Once the selected cases have been fully restored, have the staff member begin reviewing cases for discontinuity between lesions following the steps below.
- Click on Review Study from the main screen. A list of cases will appear on the screen. Change the order of sorting between patient name or study date to organize the review of cases by the specific patient or by the date that procedures were performed.
- Select the case of interest from the list of cases and click Ok. An image of all the lesions will appear on the screen as red bubbles. If lesions (VISItags) do not initially appear, then click on the VISItag toolbar to get a dropdown menu, click on the image of the VISItags from the menu, then at the bottom of the dropdown menu, select all NOT in view to make them appear on the screen as red bubbles.
- To observe the structure of the Left Atrium with the lesions, select an LA map from the map dropdown menu at the top of the left screen that has the most VISItags appear.
- Ensure the selected map is Active. To activate a certain map with all the VISItags, select the small circle (next to the small square) in the dropdown menu for the map that was previously selected. This will show the list of the sequential VISItags in the graph viewer section on the left side of the screen.
- Adjust the transparency as needed (by clicking the < or > buttons on the keyboard); more transparency on the map will allow the circle of lesions around the entire vein to be visible.
- Click on Window at the very top left corner of the screen | select Graph Viewer and drag it to the left side of the screen. The Graph Viewer screen will show a list of the lesions in the order that they were placed.
- Click on the first point (VISItag) at the top of the list of lesions in the graph viewer section on the left side of the screen. Right-click the VISItag number, then click on Select VISItag location.
- Observe, on the right side of the screen, the orange highlighted lesion of the left atrium. Rotate around the screen if the view is obstructed to see a clearer image of the highlighted lesion. Do this by holding down the center button on the mouse and dragging the mouse on the table surface.
- Repeat steps 2.9.-2.9.1. for every VISItag in sequential order on the graph view list of lesions.
- As the staff member highlights each VISItag lesion, ask them to begin recording the CI for the right and left pulmonary veins using the parameters defined below.
- Record a ZERO (0) increase in CI:
- The first lesion placed on each of the right or left vein does not increase CI.
- Lesions that overlap the previously placed lesion (as determined by the 3-D mapping software and visual determination) do not increase CI.
- A lesion that is placed that connects the path of continuous lesions to other lesions (such as closing the circle around the pulmonary veins) does not increase the CI.
- Do not increase the CI for lesions that are placed on top of the completed continuous line of lesions for extra burning/further isolation (touch-ups).
- Record a ONE (+1) increase in CI:
- Add one (+1) discontinuity for any lesion placement that is clearly not touching the last lesion placed.
- Add one (+1) discontinuity for every significant jump across each pulmonary vein (except in scenario 2.10.1.1-do not add discontinuity increment for the first lesion on a new vein after the first vein is isolated).
- Sum the CI once every VISItag has been selected and observed. The summation will be the total CI score. Score CI separately for both left and right pulmonary veins for more granular data. The sum of the two scores equals the total continuity index score.
- Record a ZERO (0) increase in CI:
- To complete data collection of additional relevant case information (i.e., ablating physician, date of procedure, patient gender, DOB), follow the steps below.
- After selecting each tag, select study from far to lefthand corner, then click on continue study.
- Click on Setup | study and record the additional data of interest.
- To exit the software, click on Study in the top left corner of the screen, then select Exit.
Representative Results
Data from a total of 75 patients treated with PVI using proactive esophageal cooling were recorded. The mean patient age was 69.8 ± 9.0 years, with 42.7% female, 37.3% paroxysmal, and 62.7% persistent AF. The mean ± SD CI for PVI was 2.6 ± 3.7 and was similar between the isolation of the left pulmonary veins (1.2 ± 1.7) and the right pulmonary veins (1.4 ± 2.3). Out of the 75 patients, only 5.3% (4) had a CI above 6 on either side, and only 22% (16) had a total CI above 6. Figure 3 shows the mean CI for left and right veins for the cohort. As a comparison, a representative case from the same lab using LET monitoring was reviewed, and found that the total CI was 29; 15 on the left side and 14 on the right side.
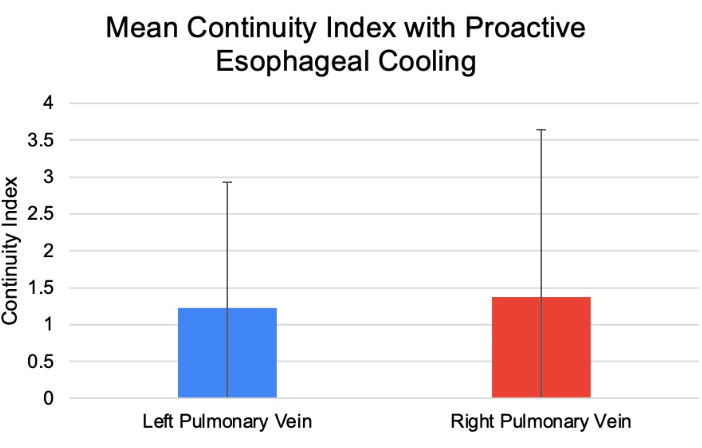
Figure 3: Mean CI of left and right pulmonary veins for a cohort of 75 patients analyzed using proactive esophageal cooling. Abbreviation: CI = continuity index. Please click here to view a larger version of this figure.
Discussion
The CI is an additional measure that reflects the quality of isolation obtained in PVI cases. Kautzner et al., in the EFFICAS II study, developed the initial method for measuring this key variable and demonstrated the significant influence of CI on the completeness of isolation and the resultant freedom from arrhythmia3. In the protocol described here, the CI calculation was modified from the EFFICAS II study to further simplify the calculation and to provide a simpler means to calculate CI both prospectively in real-time live cases, as well as retrospectively from routinely obtained case recordings (Figure 4). Viewing the pulmonary veins and assessing which quadrant any given lesion was placed in during a live case can be challenging (due to the lack of formal demarcations of pulmonary vein segments and the resulting ambiguity of an appropriate number of index units to increment). The proposed modified method described here captures the underlying presumptions and methodology reported in EFFICAS II while offering a more feasible approach to obtaining the CI for each case that may in turn lend itself to automation in existing mapping systems.
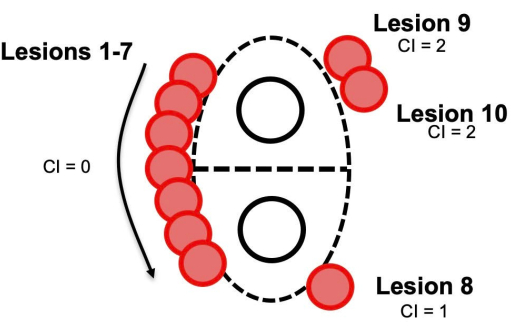
Figure 4: Example of modified continuity index calculation for real-time and retrospective calculation. These calculations involve incrementing each non-adjacent lesion by one unit only. Abbreviation: CI= continuity index. Please click here to view a larger version of this figure.
The critical piece to determining the CI in prospective cases is having a staff member available with the ability to follow lesion placement and record data during real-time procedures. The critical piece for retrospective case review is having a staff member with access to the CARTO 3 mapping software to be able to easily and efficiently access the case and record the data. The critical step of the protocol that details counting and summation of the CI (steps 2.9.7-2.10) for retrospective cases typically takes ~10-15 min. However, approximately 30 additional min are required to complete the prior steps, as downloading can take over 10 min per case.
Limitations in the method include the fact that calculating the CI during a live case requires an additional person to be in the room while a physician is ablating, and the time requirement for this effort. This individual typically spends an hour or longer in each case to ensure they are present from first through last lesion placement. Many labs and control rooms have limited space, and an additional person may be difficult to accommodate. Measuring the CI for a retrospective case also requires a dedicated person to be available. In this study, one representative retrospective case was provided as a comparison of CI in a LET-monitored PVI. Additional data are currently in collection to provide a more formal and adequately powered comparative analysis.
Additional limitations include that the data collected were from 4 operators at a single center for both the prospective and retrospective cases. While retrospective review likely minimized bias, it is possible that the electrophysiologist may have altered their lesion placement strategy to minimize CI while data were being obtained during the prospective cases. Additionally, the CI of each case was determined by one reviewer and not independently validated by a second reviewer.
Future applications or directions of the method would be automating the CI acquisition process. Similar to catheter-tissue contact force, CI would ideally be an auto-generated value calculated in real-time during the case, measured by lesion location placement via the catheter and the existing electroanatomical mapping capabilities. Physicians approaching 5-6 CI units during a case could then adjust their next planned lesion placement or adopt other methods to minimize lesion discontinuity/high CIs.
Proactive esophageal cooling utilizing the ensoETM (Attune Medical, Chicago) during RF ablation allows the attainment of a low CI. Previous publications suggest this may be a possible mechanism for the higher rates of long-term freedom from arrhythmia seen in PVI cases with proactive cooling10,11. A prospective randomized controlled trial (NCT04577859) comparing the effect of proactive esophageal cooling versus LET monitoring on long-term procedure efficacy is underway. This multi-center study has an enrollment target of 250 patients, and sites will include CI data. Further exploration of this variable within a randomized controlled trial is expected to provide stronger estimates of the influence of CI on long-term freedom from arrhythmia. Strong evidence of a significant influence may in turn support efforts from ablation catheter manufacturers to develop software to include this measure.
Acknowledgements
Research reported in this publication was supported in part by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number R44HL158375 (the content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health)
Materials
| Name | Company | Catalog Number | Comments |
| Blanketrol III hyper-hypothermia system | Gentherm Medical, Cincinnati, OH | Model 233 | Programmable heat exchanger for temperature regulation |
| Carto 3 System | Biosense Webster, Inc. (J&J MedTech), Irvine, CA | FG-5400-00 | 3-D mapping system with the integration, scalability and insights to help electrophysiologists make optimal treatment decisions. |
| ensoETM | Attune Medical, Chicago, IL | ECD02A | Active esophageal cooling device |
| Esophageal Stethoscope with Temperature Sensor Level 1 | Smiths Medical ASD Inc., Minneapolis, MN | ES400-18 | Luminal Esophageal Temperature (LET) monitoring system |
References
- Scott, M., et al. Contemporary trends in cardiac electrophysiology procedures in the United States, and impact of a global pandemic. Heart Rhythm O2. 4 (3), 193-199 (2023).
- Jankelson, L., et al. Lesion sequence and catheter spatial stability affect lesion quality markers in atrial fibrillation ablation. JACC Clin Electrophysiol. 7 (3), 367-377 (2021).
- Kautzner, J., et al. EFFICAS II: optimization of catheter contact force improves outcome of pulmonary vein isolation for paroxysmal atrial fibrillation. Europace. 17 (8), 1229-1235 (2015).
- Thomas, S., et al. Higher contact force during radiofrequency ablation leads to a much larger increase in edema as compared to chronic lesion size. J Cardiovasc Electrophysiol. 29 (8), 1143-1149 (2018).
- Ren, J. F., Callans, D. J., Schwartzman, D., Michele, J. J., Marchlinski, F. E. Changes in local wall thickness correlate with pathologic lesion size following radiofrequency catheter ablation: an intracardiac echocardiographic imaging study. Echocardiography. 18 (6), 503-507 (2001).
- Della Rocca, D. G., et al. Clinical presentation, diagnosis, and treatment of atrioesophageal fistula resulting from atrial fibrillation ablation. J Cardiovasc Electrophysiol. 32 (9), 2441-2450 (2021).
- Shen, K. R. Commentary: The rising storm of atrioesophageal fistulae after catheter ablation for atrial fibrillation. JTCVS Tech. 6, 169 (2021).
- Tan, M. C., et al. Causes of early mortality after catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 16 (5), e011365 (2023).
- Sanchez, J., et al. Atrioesophageal fistula rates before and after adoption of active esophageal cooling during atrial fibrillation ablation. JACC Clin Electrophysiol. 9 (12), 2558-2570 (2023).
- Wm Leung, L., et al. Effect of esophageal cooling on ablation lesion formation in the left atrium: insights from ablation index data in the IMPACT trial and clinical outcomes. J Cardiovasc Electrophysiol. 33 (12), 2546-2557 (2022).
- Joseph, C., et al. Improved 1-year outcomes after active cooling during left atrial radiofrequency ablation. J Interv Card Electrophysiol. 66 (7), 1621-1629 (2023).
- Mercado Montoya, M., et al. Proactive esophageal cooling protects against thermal insults during high-power short-duration radiofrequency cardiac ablation. International Journal of Hyperthermia. 39 (1), 1202-1212 (2022).
- Sessler, D. I. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 109 (2), 318-338 (2008).
- Griffin, B. R., Frear, C. C., Babl, F., Oakley, E., Kimble, R. M. Cool running water first aid decreases skin grafting requirements in pediatric burns: a cohort study of two thousand four hundred ninety-five children. Ann Emerg Med. 75 (1), 75-85 (2020).
- Bender, D., et al. The acute impact of local cooling versus local heating on human skin microcirculation using laser Doppler flowmetry and tissue spectrophotometry. Burns. 46 (1), 104-109 (2019).
- Cooper, J., et al. Active esophageal cooling during radiofrequency ablation of the left atrium: data review and update. Expert Rev Med Devices. 19 (12), 949-957 (2022).
- Joseph, C., et al. Reduced procedure time and variability with active esophageal cooling during radiofrequency ablation for atrial fibrillation. JoVE. (186), (2022).
- Bunch, T. J. Hope, hype, and reality of pulsed field ablation for atrial fibrillation. N Engl J Med. 389 (18), 1720-1721 (2023).
This article has been published
Video Coming Soon
ABOUT JoVE
Copyright © 2024 MyJoVE Corporation. All rights reserved