Signal Acquisition, Score Interpretation, and Economics of a Non-Invasive Point-of-Care Test for Coronary Artery Disease
In This Article
Summary
The methodology to acquire the physiological signal for a Coronary Artery Disease (CAD) test is presented. A method is proposed to interpret the CAD score concerning test positivity and negativity, including the granularities of each. The economics of the test are discussed in the context of the current standard of care.
Abstract
A point-of-care non-invasive test for Coronary Artery Disease (CAD) (POC-CAD) has been previously developed and validated. The test requires the simultaneous acquisition of orthogonal voltage gradient (OVG) and photoplethysmogram signals, which is the primary methodology described in this paper. The acquisition of the OVG, a biopotential signal, necessitates the placement of electrodes on the prepared skin of the patient's thorax (arranged similarly to the Frank lead configuration, comprising six bipolar electrodes and a reference electrode) and a hemodynamic sensor on the finger (using a standard transmission modality). The signal is uploaded to a cloud-based system, where engineered features are extracted from the signal and supplied to a machine-learned algorithm to yield the CAD Score. The physician must then interpret the value of the CAD Score in the context of their patient's pre-test probability of CAD, resulting in a post-test probability of CAD. This interpretation can be performed at the level of test positivity and test negativity or at a finer level of granularity; methodologies for each are proposed here based on likelihood ratios. Using the post-test probability, the physician must determine the appropriate next step in the treatment of their patient; several scenarios are used to illustrate this process. Test adoption is only feasible if economically viable; a discussion of the integration of the test into the CAD diagnostic flow and the resultant cost savings to the healthcare system is provided. The economic model demonstrates that cost savings to the healthcare system can be achieved by preventing delayed treatment, which, if left unaddressed, results in disease progression requiring more advanced (and expensive) care.
Introduction
Ischemic heart disease (IHD) is currently the leading cause of death globally1. Coronary artery disease (CAD) is the anatomical precursor to IHD, characterized by the presence of significant lesions within the coronary arteries. Significance can be defined anatomically by an occlusion of at least 70%, or 50% in the left main artery2. Significance can also be defined based on the functional impact of the lesion by measuring its effect on blood flow. Specifically, fractional flow reserve (FFR) and instantaneous flow reserve (iFR) assess the change in flow caused by the lesion, and lesions are defined as significant at FFR < 0.80 or iFR < 0.892. The gold standard for confirming the presence of significant CAD is invasive coronary angiography (ICA) by left heart catheterization (LHC). Significant CAD warrants revascularization through the placement of a stent or coronary artery bypass grafting, which alleviates myocardial ischemia and corresponding anginal symptoms and stabilizes the plaque (in the case of stenting).
Current non-invasive testing for CAD often requires radiation exposure, stress, and contrast injection (with renal impacts)1. The most commonly used diagnostic tests are myocardial perfusion imaging (MPI), also known as single photon emission computed tomography (SPECT), and coronary computed tomographic angiography (CCTA). SPECT involves the injection of a radioisotope to track perfusion during rest and stress (exercise or pharmaceutical). CCTA images the coronary arteries using multiple X-rays. Positron Emission Tomography (PET) and cardiac magnetic resonance imaging (CMR) are also occasionally used for CAD testing1. All these modalities require significant capital investment in equipment, trained personnel to perform the tests, and, in some cases, the availability of medical isotopes. Due to these requirements, these modalities are often not broadly available, especially in rural settings, which introduces delays in patient care and escalates associated risks.
Therefore, the goal was to design a non-invasive, point-of-care test for CAD (POC-CAD): the CorVista system3. This system is an FDA-cleared test for functionally significant CAD, with performance comparable to CCTA4. The test can be used without patient stress and without the need for capital investment in equipment or specialized staff. It is ideally suited for use in rural and resource-constrained environments where access to current imaging technologies is often not available.
The development3 and validation4 of POC-CAD have been published previously. Briefly, POC-CAD begins with the simultaneous acquisition of orthogonal voltage gradient and photoplethysmogram signals using the Capture device, as described in Protocol step 1. The orthogonal voltage gradient is a biopotential signal acquired using a lead placement similar to the Frank lead configuration5, comprising six bipolar electrodes and a reference electrode attached to the torso. The photoplethysmogram is obtained using the standard transmission modality, where red and infrared light is transmitted through the fingertip and strikes a sensor6. Once the signal is acquired, it is automatically uploaded to the cloud-based system, where engineered features are extracted from the signal and supplied to a machine-learned algorithm to yield the CAD score, which is presented in the web portal. In Protocol steps 2 and 3, the methodology to interpret the CAD Score returned by the test is described. Specifically, either published data or other sources relevant to the physician can be used to estimate the probability of CAD prior to the patient taking the test. Likelihood ratios can be calculated from the test performance and used to update the probability of CAD from pre-test to post-test, using either the binary test result (step 2) or more granular values of the CAD score (step 3). Finally, the modeling of the economics of POC-CAD in comparison to the current standard of care is discussed.
Protocol
The study was approved by the Western Institutional Review Board and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all subjects for participation. Briefly, to be included, subjects must have been at least 18 years of age with cardiovascular symptoms but without known coronary artery disease and scheduled to undergo ICA or CCTA. Exclusion criteria included prior documented history of myocardial infarction, prior coronary artery bypass grafting, and prior heart valve replacement, among others. Complete study inclusion and exclusion criteria can be found on clinicaltrials.gov, under National Clinical Trial (NCT) number NCT03864081. The equipment and the software used are listed in the Table of Materials.
1. Signal acquisition
- Prepare the skin by shaving any hair from the electrode site. Ensure that there is no remaining residue on the skin by cleaning with soap and water and employing a clean and dry gauze or non-alcoholic wipe if needed.
- Connect the leads to electrodes and place them in accordance with Table 1.
NOTE: Electrode quality may affect the signal quality; it is recommended to use diagnostic quality or high-performance electrodes. - Place the hemodynamic (photoplethysmogram, PPG) sensor on the subject's finger, ensuring that the finger is as far into the sensor as possible, with the sensor cable positioned along the top of the hand.
- Utilize the index finger unless a wound or other clinically relevant reason precludes its use. Advise the patient not to move the sensor once it is placed.
- Position the patient flat on their back in a comfortable resting position. Ensure that the PPG sensor cable and electrode cables do not overlap.
- Use cushioning (e.g., a rolled blanket or towel, along with a pillow) if needed to prevent the patient from placing direct pressure on the blue electrode on the back.
- To limit signal noise and maximize signal quality, to the degree possible, turn off all electronic devices (monitors, televisions, cell phones, etc.) or remove them from the room. Turn off the room lighting.
- Enter the patient information and confirm correctness: patient's first name, patient's last name, gender at birth, height in inches, weight in pounds, date of birth, and medical record number (all required, may be entered in any order).
- Ensure that the patient is comfortable, and remind them to be still and quiet (e.g., no talking during the acquisition).
- Place the device on a flat surface and confirm the placement in the application. Press Start to commence the signal acquisition.
- Monitor the device for any error messages, and if they appear, follow the directions on the screen to resolve them.
- After the signal acquisition is complete, requiring 3 min and 35 s, the device will automatically transmit the data to the cloud for signal quality assessment. Keep the patient attached to the device until confirmation of passing signal quality is received.
- Detach the electrodes from the patient and remove the PPG sensor.
- Access the portal to view the test results (will be available about 10 min after the signal has been uploaded to the cloud).
Table 1: Lead placement. Description of the anatomical locations at which each of the seven electrodes should be placed. Please click here to download this Table.
2. Interpreting the test results given test-positive vs . test-negative
- Determine the patient's pre-test probability of disease (e.g., using the European Society of Cardiology (ESC) guidelines7).
- Determine whether the patient's test is positive or negative by comparing the CAD score to 0: if greater than or equal to zero, then the patient's result is test-positive, or if less than zero, then the result is test-negative.
- Read the CAD Score value from the report and compare it to the distributions of negative and positive patients in the validation cohort shown at the bottom of the report.
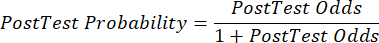
- Calculate the sensitivity and specificity8, then the likelihood ratios (LR) using equation 1 and equation 29.
NOTE: A worked example is shown, given that the test sensitivity is 88% (calculated using subjects positive from ICA, which is the sole group of subjects with disease) and specificity is 51% (calculated using subjects negative from CCTA at a 94% weight and subjects negative from ICA at a 6% weight, to represent the overall population via the PROMISE study10).
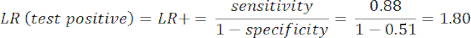 (eqn 1)
(eqn 1)
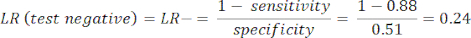 (eqn 2)
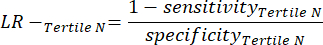
(eqn 2) - Calculate the patient's post-test probability given the following equations 3-511, where LR+ is used in the case of a positive test and LR- is used in the case of a negative test:
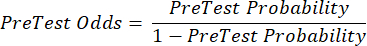 (eqn 3)
(eqn 3)
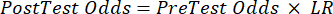 (eqn 4)
(eqn 4)
 (eqn 5)
(eqn 5) - With the updated probability of CAD, given the results of the test, determine the appropriate next step in patient care (e.g., using the ESC guideline7 recommendations shown in Table 2).
Table 2: ESC guidelines by probability of CAD. For four levels of probability of CAD, the European Society of Cardiology guidelines are for the appropriate interpretation of that probability, including the next test (if necessary). Please click here to download this Table.
3. Interpreting the test results given at finer granularity
- Increase the granularity of the test-positive and test-negative results by considering ranges of the CAD score observed in the population used to validate the test, specifically division into tertiles (equal number of subjects in three bins) in the test-positive and test-negative ranges, as shown in Table 3.
NOTE: To simplify the calculations, the 6% contribution of the subjects negative from catheterization is excluded from this analysis, the inclusion of which will not change the outcomes significantly. - Within each tertile in the test-negative range, calculate the number of True Negatives (TN), which are subjects that truly do not have the disease, and the number of False Negatives (FN), subjects who truly do have the disease.
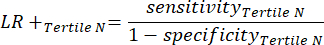
- Apply the following equations 6-811 to determine the LR- of each test-negative tertile (LR+ from negative tertiles not relevant).
NOTE: The equations assume that the performance profile of the tertile represents the full test-negative range to calculate performance statistics (necessitating the correction factor of three, corresponding to the number of tertiles, to achieve the original test-negativity frequency with respect to test positivity).
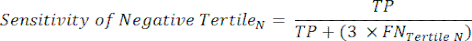 (eqn 6)
(eqn 6)
 (eqn 7)
(eqn 7)
 (eqn 8)
(eqn 8)
- Apply the following equations 6-811 to determine the LR- of each test-negative tertile (LR+ from negative tertiles not relevant).
- Within each tertile in the test-positive range, calculate the number of True Positives (TP), which are subjects that truly have the disease, and the number of False Positives (FP), subjects who truly do not have the disease.
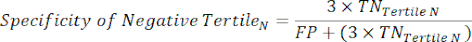
- Apply equations 9-11 to determine the LR+ of each test-positive tertile (LR- from positive tertiles not relevant)11.
NOTE: The equations assume that the performance profile of the tertile represents the full test-positive range for the purpose of calculating performance statistics (necessitating the correction factor of three, corresponding to the number of tertiles, to achieve the original test-positivity frequency with respect to test negativity).
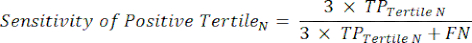 (eqn 9)
(eqn 9)
 (eqn 10)
(eqn 10)
 (eqn 11)
(eqn 11)
- Apply equations 9-11 to determine the LR+ of each test-positive tertile (LR- from positive tertiles not relevant)11.
- Determine which tertile the patient's CAD score lies within, and given the LRs in Table 3, calculate the post-test probability given the procedure shown in step 2.
NOTE: As may be expected, the LR- values decrease with more negative CAD scores, and the LR+ values increase with more positive CAD scores, meaning that a more negative CAD score more effectively reduces the pre-test probability, and a more positive CAD score more effectively increases the pre-test probability. - As an alternative to performing the calculations listed in steps 2.4-3.4, use Table 4 to translate the pre-test probability into a post-test probability using the patient's CAD score7.
Table 3: Likelihood ratios. For three ranges of scores within test-positive and test-negative, the corresponding positive likelihood ratios and negative likelihood ratios, respectively. Please click here to download this Table.
Table 4: Pre-test to post-test probability mapping. For 10 levels of pre-test probability, the corresponding post-test probability given a CAD score in each of the three negative tertiles, and each of the positive tertiles. Green coloring corresponds to <15% disease probability (ESC guideline states that CAD can be ruled out); yellow coloring corresponds to 15%-65% disease probability (ESC guidelines state that imaging-based non-invasive testing is preferable); orange corresponds to 66%-85% disease probability (ESC guidelines states that imaging-based non-invasive testing should be performed); red corresponds to >85% disease probability (ESC guideline states that CAD can be ruled in). See Table 2 for further guideline information. Note that a CAD score of 0 is considered test-positive. Please click here to download this Table.
Representative Results
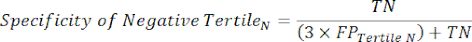
An example signal can be seen in Figure 1, and report in Figure 2, as would appear to a physician using the test. Below are several patient cases provided to demonstrate the application of the methodology in interpreting the CAD score's significance.
Case 1
A 67-year-old man presented complaining of symptoms of chest pain at rest, with radiating arm pain, along with diaphoresis and nausea. Based on the ESC guidelines7, his age, sex, and symptoms are consistent with an initial probability of disease of 84%. The ESC guidelines suggest that such a patient requires non-invasive testing to make a diagnosis of CAD to warrant referral to cardiac catheterization and any needed intervention (Table 2). POC-CAD was performed, returning a CAD score of 0.32, which is a test-positive result and falls in the highest tertile of positive CAD Scores, with an LR+ of 2.888 (Table 3). Therefore, the patient's post-test probability is 94%, and per the ESC guidelines (Table 2), the patient can safely be assumed to have CAD, and invasive cardiac catheterization is an appropriate course of action.
Case 2
A 39-year-old woman presents with chest pain at rest, radiating to both the left and right side. Based on the ESC guidelines7, her age, sex, and symptoms are consistent with an initial probability of disease of 28%, and the guidelines suggest that a non-invasive test would be the preferable next step to gain a greater understanding of the probability of CAD. However, the guidelines also state that in young patients (such as this 39-year-old woman), the physician should be conscious of radiation exposure, which is necessary to administer a test such as SPECT, requiring an injected radioisotope. Another option for such a test is CCTA, but that requires many X-rays. Therefore, POC-CAD is a logical choice, as it doesn't require radiation. The test was performed, returning a value of -0.12, within the bounds of the first tertile of the negative range, with an LR- of 0.129 (Table 3). The resultant post-test probability is 4%, which falls to the level where CAD can be safely ruled out per the ESC guidelines, with no further testing required for CAD.
Case 3
A 74-year-old female presents with non-anginal chest pain and dyspnea. Based on the ESC guidelines7, her age, sex, and symptoms are consistent with an initial probability of disease of 24%, and the guidelines suggest that a non-invasive test would be the preferable next step to gain a greater understanding of the probability of CAD. The patient is hesitant to travel from the rural clinic where she is being treated to the large urban center where all the testing modalities (PET, SPECT, CCTA, CMR) are available, so the physician offers POC-CAD. The CAD score is 0.07, falling into the first tertile of the positive range with an LR+ of 1.446, resulting in a post-test probability of 33%. Based on the positive result and the increase in the probability of disease, the patient agrees to travel to the city for a PET scan. The PET was also indicative of disease, with an LR+ of 6.0412, and augments the 33% to 75% post-PET.
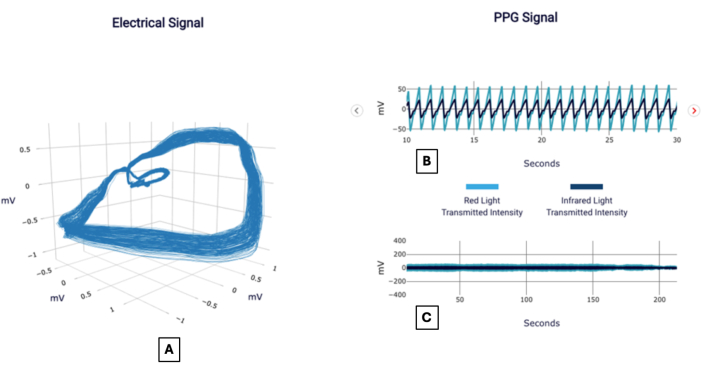
Figure 1: Example signals. Exemplar POC-CAD report showing visualizations of the orthogonal voltage gradient, also referred to as the electrical signal (A), and the photoplethysmogram signal focused on a 20 s interval (B) and full duration (C). Please click here to view a larger version of this figure.
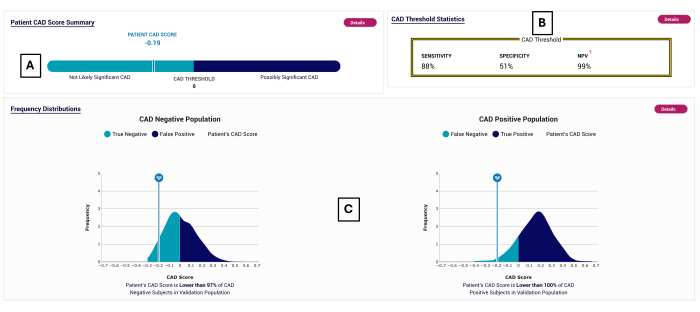
Figure 2: Example CAD report. Exemplar POC-CAD report, showing a CAD Score of -0.19 (A), which falls into the test-negative range (<0). The test performance is shown in (B). The distribution of CAD scores is displayed for the subjects on which POC-CAD was validated in (C). Please click here to view a larger version of this figure.
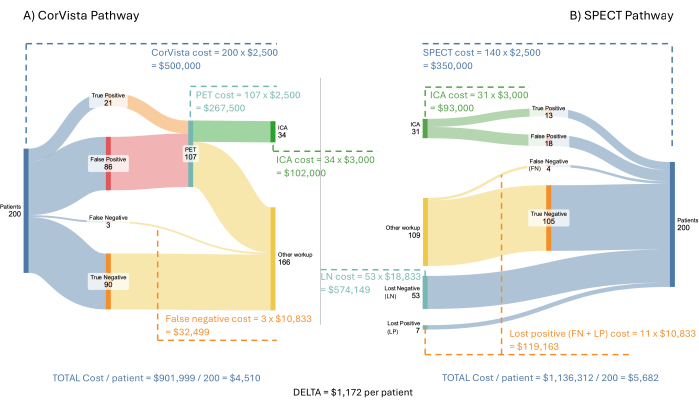
Figure 3: Cost economic model flow. A hypothetical incoming population of 200 patients is run through the POC-CAD>PET pathway (A) and the SPECT pathway (B). The costs to the healthcare system are shown for each branch of each pathway, along with the average saving per patient when the POC-CAD>PET pathway is implemented. Please click here to view a larger version of this figure.
Discussion
The primary focus of this section is the economics of the test; however, it is useful to discuss the aspects of the assessment of pre-test probability for CAD first. As described in Protocol steps 2 and 3, the estimation of the pre-test probability of CAD is a critical step in contextualizing the CAD Score and determining the post-test probability of CAD. We have used the ESC 2013 guidelines, which base the probability of CAD on three characteristics: gender, age, and symptoms (within groups of typical angina, atypical, and non-anginal pain)7. However, it is important to note that the physician may apply their clinical judgment in the selection of any quantitative or qualitative method. Further, there are other published quantitative methods available for such estimation, including Diamond-Forrester13, which requires the same input characteristics as ESC 2013. More comprehensive variations have also been published, such as which extends14 Diamond-Forrester with estrogen status for females (to compensate for age variation in menopause, as well as any hysterectomy), as well as diabetes, hypertension, hyperlipidemia, smoking, family history of coronary disease, and obesity. However, be aware that some methodologies may define CAD at 50% luminal narrowing, whereas 70% represents the current ACC guidelines (barring the left main artery at 50%).
The economics of POC-CAD and how the test interacts with the care pathway represent crucial characteristics in determining whether the test is truly suitable for clinical use. For the diagnosis of CAD, the most often used test is MPI, often known as a nuclear stress test or SPECT. As of 2019, MPI was used in approximately 85% of assessments for CAD15. An estimated 7-8 million SPECT-MPI studies are performed in the USA annually16. In approximately 5% of patient cases, CCTA is used to diagnose CAD. CCTA has been recognized as having superior diagnostic performance in ruling out significant CAD. Two other imaging modalities, PET and cardiac MRI, make up the bulk of the remaining assessments. For all of these tests, an imaging camera and a qualified team are required to run and interpret the test. Such cameras are expensive pieces of capital equipment. Consequently, these tests are often limited in availability to urban healthcare settings, where there is sufficient volume to justify both the initial expense plus operating costs.
In 2021, the American College of Cardiology (ACC) published its guidelines for patients with no known CAD or former tests and with intermediate risk of CAD2,17where both MPI and CCTA were recognized as front-line diagnostic options. In contrast to CCTA and MPI, POC-CAD may be used in any point-of-care setting, such as a physician's office, critical access hospital, tribal care center, and tertiary care centers, rather than being restricted, as CCTA and MPI are, to only those centers with expensive imaging equipment and the teams required to operate them.
Typically, patients who are suspected of CAD following a front-line test will be referred for ICA; as described, this is considered the gold standard diagnostic for CAD. ICA is an invasive procedure undertaken in an outpatient hospital setting by invasive cardiology specialists.
A recent study of an appointment attendance rate for radiological examinations at a large tertiary academic center showed that 24% of scheduled appointments were not attended by the patient due to either cancellation or no-show18. Radiological modalities studied included CAD diagnostics. The figure reported in that study aligns with a discussion with the financial officer of a healthcare system, who assumes a no-show rate of 20%. Further, in multiple discussions with rural physicians, where significant travel time may be required to reach the test, up to 50% of patients might not proceed to both make an appointment and attend the appointment. In the following model, conservatively for the rural market, this is assumed to be 30% (i.e., 70% attend the appointment).
There is a direct impact on the diagnostic yield of downstream tests where significant numbers of patients do not proceed to the recommended test. Assuming that the rate is consistent across individuals with and without significant coronary artery disease, the sensitivity of detecting the condition across the referred population would be 70% of the expected sensitivity. In the case of SPECT, which has a reported sensitivity for detecting functionally significant CAD of 73%, the effective sensitivity is just 53% (= 0.7 x 73%)12, i.e., almost half of those patients in the referred population with functionally significant CAD would be missed. These missed patients do not cost the healthcare system zero. The positive patients with functionally significant CAD will likely be seen later and incur significant additional costs due to the progression of their disease. For example, if the patient subsequently presents at the emergency department, the average cost of the visit for a patient with signs of acute coronary syndrome has been calculated as $30,00019.
Furthermore, even for those patients without significant CAD, if they do not follow their physician's referral for imaging, they are less likely to return to that physician, and thus, there is limited opportunity to determine what else might be causing their symptoms. This can also be costly to both the patient, in terms of the progression of the underlying condition, and the healthcare system. For example, a delay in diagnosis of heart failure has been shown to add an incremental $8,000 per year to the cost of treating that patient20.
The cost economic model presented here aims to capture these impacts, comparing the scenario where POC-CAD is used as the front-line test for significant CAD to a scenario in which SPECT is used. As POC-CAD is a rule-out test, a larger number of false positive results are expected than for SPECT. It is unreasonable to expect that all positives from the test would proceed to ICA. In many cases, it would be ideal to employ a second test. When analyzing the rule-in and rule-out performances of various non-invasive tests for functionally significant CAD, Knuuti et al. recommend following CCTA with a functional test, such as SPECT12. However, this again runs the risk of failing to identify a relatively large proportion of the positive patients. A better functional test would be cardiac PET, which has a sensitivity of 89% and specificity of 85%12. Cardiac PET is increasingly being used in the USA, is currently most often prescribed by cardiologists, and is already used more often than CCTA15,21. In this model, positives from PET are then assumed to proceed to ICA. As the sensitivity of PET is similar to the sensitivity of POC-CAD, all positives in the incoming PET population are assumed to be correctly classified as positive by PET. In the model in which SPECT is used as the front-line test, positives are assumed to proceed to ICA. Assuming an incoming prevalence of 12%, this results in a positive yield at ICA of 41%, which is close to that observed in the PROMISE study10.
Figure 3 depicts the model and results using a hypothetical incoming population of 200 patients with symptoms of cardiovascular disease. Each of SPECT, PET, and POC-CAD is assumed to be reimbursed at the same rate: $2,500 per test. ICA is assumed to be reimbursed at $3,000. The cost of any treatment during ICA, or subsequently, is not included in the model as this is beyond the diagnostic pathway that the model represents. The costs of lost negative and lost positive patients are more difficult to estimate. Given that these patients are defined as having not followed their physician's direction to proceed with an imaging test, it is assumed that their next interaction with the healthcare system is to present at an emergency department with symptoms of cardiovascular disease. In a study of emergency department presentations with such symptoms, Pope et al. determined that 17% met the criteria for acute cardiac ischemia, 6% had stable angina, 21% had nonischemic cardiac problems, and 56% had noncardiac problems22. The costs for initial presentation at the emergency department have been calculated by O'Sullivan et al. as $34,200 for non-fatal myocardial ischemia and $17,300 for angina without coronary revascularization23. Using solely the costs at the initial presentation is a conservative approach as the acute phase (3-year) costs incurred for the event are substantially higher, at $73,300 and $36,000, respectively. The cost of an emergency department visit for 53% of visits for chest pain, but with no resultant cardiac problem identified, has been estimated as $2,988 using information reported by United Healthcare24. Finally, for the 21% with a nonischemic cardiac issue, the cost has been estimated as $2,988, plus an incremental cost caused by delay in treating the cardiac condition. As stated above, for a patient with heart failure, the incremental annual cost of delayed diagnosis has been calculated at $8,00020. Therefore, the cost for the 21% has been assumed to be $10,988, assuming that the majority of these patients will have either heart failure or pulmonary hypertension and a similar delayed treatment cost for both. Once again, using just one year of incremental cost is a conservative approach as this would, in fact, apply to each subsequent year. Overall, the weighted average of these costs, as used in the model, is $10,833.
The cost economic model demonstrates a potential average saving of $1,172 per patient to the health care system due, in summary, to the cost of delayed treatment resulting in disease progression requiring more advanced care. Additionally, adopting this pathway would increase the yield at ICA to 62%, compared to the 41% currently observed and modeled in the SPECT pathway.
If extrapolated out to the incoming rural population of 2.25 million patients presenting per year with symptoms of cardiovascular disease in the USA, the total potential savings of implementing POC-CAD as a front-line test for significant CAD would be approximately $2.64 billion. As discussed above, a large component of these savings is derived from not missing patients with functionally significant CAD due to a higher sensitivity and higher diagnostic yield than SPECT. Additionally, the higher yield that could be achieved at ICA is a crucial benefit as more ICAs would be performed under the POC-CAD>PET pathway than the SPECT pathway. A higher yield at ICA would be beneficial to patients, who are often currently frustrated by negative ICA results25, the interventional cardiologist, and the healthcare system.
One possible objection to this model is that everyone should be referred directly to PET rather than using the POC-CAD test first. This approach, especially when considering the rural population, could be fraught with the same issue that is currently observed with all imaging tests - that of loss to follow-up. If the same assumptions for the model were maintained, the effective yield of PET would have a sensitivity of just 62% (= 0.7 x 89%), thereby still missing many of the truly positive patients in this population. Conversely, it is observed that having a positive test from POC-CAD can encourage patients to follow up with their referral for subsequent diagnostic tests (such as ICA), and hence, this is not expected to be an issue in the POC-CAD>PET pathway. One might also argue that SPECT is the predominant pathway and, hence, is most likely to be the test used in practice following POC-CAD. In this case, the savings of the resultant POC-CAD>SPECT pathway would be slightly higher than those shown above, but the effective yield at ICA would be slightly lower (58%) as there would be an additional three missed positive patients (false negatives) of two hundred in the flow.
In conclusion, POC-CAD provides a promising addition to the diagnostic pathway. The primary advantage of this test is that it can be used at point-of-care, without the use of radiation, stress, or contrast, and yet delivers results comparable to those of CCTA for ruling out functionally significant CAD26. Further, results are available within the same visit, allowing the physician to discuss the next steps in care with the patient without scheduling another visit. Since the test can be administered at point-of-care, and the results are rapidly available, POC-CAD addresses the significant problem of loss to follow-up observed, especially in rural areas, representing approximately one-fourth of the US population. Given the robust rule-out profile of the test, with a negative result, the physician can rapidly explore other explanations of the patient's symptoms. When the costs of the resultant delay in diagnosis of the patient are modeled, the use of POC-CAD as a front-line test would provide significant advantages to patients, physicians, and the payor. Furthermore, the existing imaging modalities would not see either a significant increase or decrease in volume, which is a concern for many imaging centers. The cost savings are realized through more timely diagnosis and treatment of the patient's condition.
Acknowledgements
The authors would like to thank Cody Wackerman and Hugh Dubberly of Dubberly Design Office (San Francisco) for their help in visualizing the pathways shown in Figure 3.
Materials
| Name | Company | Catalog Number | Comments |
| CorVista CAD | CorVista | n/a | System comprising signal acquisition, cloud processing, and delivery of a report containing the CAD Score via a web portal |
| Electrodes | Various (see comments) | Diagnostic quality or high performance electrodes are recommended. For example: Conmed ClearTrace 1700-007 Skintact FS-TB1 Vermed A10005 |
References
- . The top 10 causes of death [Internet]. 2020 [cited 2024 Jun 27] Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (2020)
- Lawton, J. S., et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 79 (2), e21-e129 (2022).
- Burton, T., et al. Development of a non-invasive machine-learned point-of-care rule-out test for coronary artery disease. Diagnostics. 14 (7), 719 (2024).
- Stuckey, T. D., et al. Clinical validation of a machine-learned, point-of-care system to IDENTIFY functionally significant coronary artery disease. Diagnostics. 14 (10), 987 (2024).
- Frank, E. An accurate, clinically practical system for spatial vectorcardiography. Circulation. 13 (5), 737-749 (1956).
- Park, J., Seok, H. S., Kim, S. S., Shin, H. Photoplethysmogram analysis and applications: An integrative review. Front Physiol. 12, 808451 (2022).
- Montalescot, G., et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 34 (38), 2949-3003 (2013).
- Baratloo, A., Hosseini, M., Negida, A., El Ashal, G. Part 1: Simple definition and calculation of accuracy, sensitivity and specificity. Emergency. 3 (2), 48-49 (2015).
- Ranganathan, P., Aggarwal, R. Understanding the properties of diagnostic tests-Part 2: Likelihood ratios. Perspect Clin Res. 9 (2), 99-102 (2018).
- Douglas, P. S., et al. Outcomes of anatomical versus functional testing for coronary artery disease. New Eng J Med. 372 (14), 1291-1300 (2015).
- Safari, S., Baratloo, A., Elfil, M., Negida, A. Evidence based emergency medicine; part 4: Pre-test and post-test probabilities and Fagan's nomogram. Emergency. 4 (1), 48 (2016).
- Knuuti, J., et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J. 39 (35), 3322-3330 (2018).
- Diamond, G. A., Forrester, J. S. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. New Eng J Med. 300 (24), 1350-1358 (1979).
- Morise, A. P. Comparison of the Diamond-Forrester method and a new score to estimate the pre-test probability of coronary disease before exercise testing. Am Heart J. 138 (4), 740-745 (1999).
- Pelletier-Galarneau, M., Vandenbroucke, E., Lu, M., Li, O. Characteristics and key differences between patient populations receiving imaging modalities for coronary artery disease diagnosis in the US. BMC Cardiovasc Disord. 23 (1), 251 (2023).
- Li, J., et al. Factors that impact a patient's experience when undergoing single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) in the US: A survey of patients, imaging center staff, and physicians. J Nuclear Cardiol. 28 (4), 1507-1518 (2021).
- Lawton, J. S., et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 79, e21-e129 (2022).
- Aijaz, A., et al. Sociodemographic factors associated with outpatient radiology no-shows versus cancellations. Acad Radiol. S1076 - 6332 (24), 00228-00229 (2024).
- Cowper, P. A., et al. Acute and 1-year hospitalization costs for acute myocardial infarction treated with percutaneous coronary intervention: Results From the TRANSLATE-ACS registry. J Am Heart Assoc. 16 (8), 8 (2019).
- Thomas, A., et al. Forgone medical care associated with increased health care costs among the U.S. heart failure population. JACC Heart Fail. 9 (10), 710-719 (2021).
- Reeves, R. A., Halpern, E. J., Rao, V. M. Cardiac imaging trends from 2010 to 2019 in the Medicare population. Radiol Cardiothorac Imaging. 3 (5), (2021).
- Pope, J. H., et al. Missed diagnoses of acute cardiac ischemia in the Emergency Department. New Eng J Med. 342 (16), 1163-1170 (2000).
- OʼSullivan, A. K., et al. Cost estimation of cardiovascular disease events in the US. Pharmacoeconomics. 29 (8), 693-704 (2011).
- Emergency visit cost with and without insurance in 2024. Mira Available from: https://www.talktomira.com/post/how-much-does-an-er-visit-cost (2024)
- Patel, M. R. Low diagnostic yield of elective coronary angiography. New Eng J Med. 362 (10), 886-895 (2010).
- Browning, S. . CorVista System 510(k) Summary (K232686). , (2024).
Explore More Articles
This article has been published
Video Coming Soon
ABOUT JoVE
Copyright © 2024 MyJoVE Corporation. All rights reserved