Eye Exam
Source: Richard Glickman-Simon, MD, Assistant Professor, Department of Public Health and Community Medicine, Tufts University School of Medicine, MA
Proper evaluation of the eyes in a general practice setting involves vision testing, orbit inspection, and ophthalmoscopic examination. Before beginning the exam, it is crucial to be familiar with the anatomy and physiology of the eye. The upper eyelid should be slightly over the iris, but it shouldn't cover the pupil when open; the lower lid lies below the iris. The sclera normally appears white or slightly buff in color. The appearance of conjunctiva, a transparent membrane covering the anterior sclera and the inner eyelids, is a sensitive indicator of ocular disorders, such as infections and inflammation. The tear-producing lacrimal gland lies above and lateral to the eyeball. Tears spread down and across the eye to drain medially into two lacrimal puncta before passing into the lacrimal sac and nasolacrimal duct to the nose.
The iris divides the anterior from the posterior chamber. Muscles of the iris control the size of the pupil, and muscles of the ciliary body behind it control the focal length of the lens. The ciliary body also produces aqueous humor, which largely determines intraocular pressure (Figure 1). Cranial nerves II and III control pupillary reaction and lens accommodation; cranial nerve III controls upper lid elevation; cranial nerves III, IV, and VI control eye movement. The six cardinal directions of gaze are controlled by six extraocular muscles (Figure 2) innervated by cranial nerves III, IV, and VI.
Visual testing is an essential part of the ophthalmological exam and is also performed as a part of cranial nerve II assessment during the neurological exam. A focused image is projected onto the retina after its light passes through the cornea, pupil, lens, and vitreous body. The projection is upside down and reversed right to left, which means that light entering from the lower temporal field of vision strikes the upper nasal quadrant of the retina. Photosensitive cells of the retina respond by generating electrical impulses, which are relayed to the optic nerve and passed to the visual cortex through the optic tracts. The right and left visual cortices process images entering from the left and right visual fields, respectively.
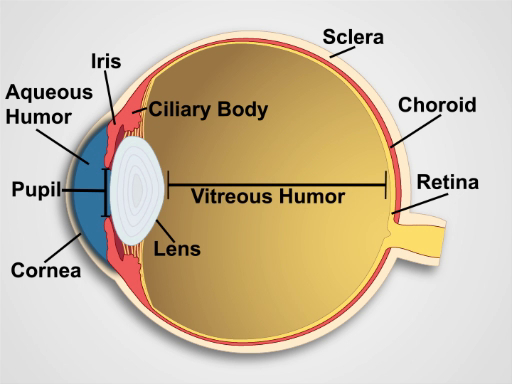
Figure 1. Anatomy of the Eye. A diagram showing a sagittal view of the human eye with the structures labeled.
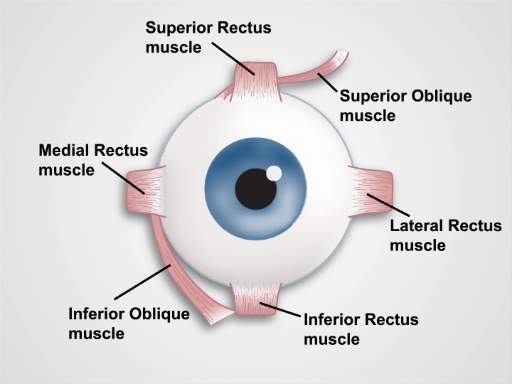
Figure 2. Muscles of the Eye. A cartoon showing a frontal view of the human eye and the extraocular muscles (labeled).
1. Vision
Visual acuity is recorded as two numbers (e.g., 20/40 corrected). The top number indicates the distance the patient stood from the chart (20 ft), and the bottom number indicates the distance from which a person with normal vision (20/20) could see the smallest line of print accurately read by the patient (40 ft with glasses). In the US, a patient with vision of 20/200 or worse is considered legally blind.
- If available, use a well-lit, wall-mounted Snellen chart.
- Position the patient 20 ft from the chart with non-reading glasses on (if normally used).
- Have the patient cover one eye with a card, and ask the patient to read the smallest line of print possible; give credit for correctly identifying half or more of the letters.
- Record the visual acuity indicated to the side of this line, noting whether it was with correction or not.
- Repeat with the other eye.
- If a wall-mounted chart is unavailable, conduct the same procedure with a specially designed card the patient can hold 14 inches away ( Figure 4), which simulates the view of a Snellen chart from 20 ft away. The card can also be used to test for presbyopia, or impaired near vision, common in people as they reach middle age; in presbyopia, vision improves when the card is held further away.
- In the absence of a chart or card, screen for visual acuity using any fine print.
- Peripheral vision.
- Begin by asking the patient to use both eyes to stare at your eyes without looking anywhere else.
- Place your hands, with two fingers raised, lateral to the patient's ears, about 2 ft apart.
- Wiggle your fingers and bring them slowly forward, curving slightly inward toward the center of vision.
- Ask the patient to tell you when the movement of your fingers can be seen in the periphery. Normally, this occurs when your fingers are even with the patient's temples or about 90° from the center of gaze on either side.
- Increase the accuracy of this exam by slowly moving a 5-mm, red-topped pin inward along the lines projecting from the four corners of the patient's visual field, noting when the patient can first see the color in each of the four quadrants.
2. Eye Inspection
- Stand in front of the patient and ask the patient to stare directly at you.
- Observe the eyes for any asymmetry or protrusions.
- Inspect the eyebrows for sparseness or scaliness and the eyelids for adequate closure, ptosis, entropion, ectropion, retraction, discoloration, lesions, swelling, masses, or discharge.
- Check for dryness or excessive tearing, and examine the lacrimal gland and sac for swelling or tenderness.
- Expose the conjunctiva and sclera by having the patient look upward while gently pulling downward on the lower lids with your thumbs. Note color, vascular dilations, nodules, swelling, or discharge.
- Shine a penlight obliquely across the cornea, noting any surface irregularities or opacities. Inspect the iris for rings, shadows, or ciliary injection, and inspect the lens for opacities.
- Inspect the pupils for their size, shape, and symmetry. Pupils are normally 3-4 mm in diameter. In anisocoria, the pupil diameters are unequal by at least 4 mm. The terms myosis and mydriasis refer to abnormally constricted or dilated pupils, respectively.
- Have the patients stare at a penlight held about 20 cm away. Note the position of the corneal reflections, which should be symmetrically located just nasal to the center of the pupils.
- Check for pupillary reaction to light by asking the patient to stare off into the distance in a slightly darkened room. Observe the patient's right pupil while swinging the penlight from right to left across the patient's right eye. It should constrict. Now, do the same maneuver while observing both eyes, taking care not to allow any light to fall on the patient's left eye. Both pupils should consensually constrict. Repeat this testing for the left eye.
- Examine the extraocular motion by asking the patient to look at your index finger and follow it as you trace the shape of a large "H" at a comfortable distance in full light. Make sure the patient's head remains still. Both eyes should symmetrically move through all cardinal directions of gaze.
- Momentarily hold the patient's gaze at the extreme upper, lateral positions, and observe for nystagmus, which appears as involuntary rhythmic oscillations of the eyes.
- Check for lid lag by looking for an abnormal rim of sclera over the iris on downward gaze.
- Finally, have the patient stare at your finger as it moves toward the bridge of the patient's nose, and watch for equal convergence of the eyes medially and equal pupillary constriction.
- If the pupils don't react, hold your finger about 10 cm away and ask the patient to alternately stare at your finger and into the distance beyond it. The pupils should constrict while focused on your finger.
Many systemic and ocular pathologies have manifestations that can be identified during an eye examination. Simple visual acuity testing with a Snellen chart, or an adequate substitute, allows screening for myopia and presbyopia - impaired far and near vision, respectively. Limitations in peripheral vision raise the possibility of glaucoma, as well as other serious conditions, and should always prompt further ophthalmologic evaluation. Localized swelling of the eyelids commonly results from infected sties or nodular chalazions caused by obstructed glands. Conjunctival paleness may be a sign of anemia, whereas hyperemia and discharge suggest conjunctivitis. A painless, localized, homogenous area of scleral redness suggests a subconjunctival hemorrhage. An acutely painful, red eye with ciliary injection around the iris may indicate corneal injury or infection, acute iritis, or acute angle closure glaucoma, all requiring urgent ophthalmologic evaluation. Jaundice first presents as a yellowing of the sclera. Eye protrusion and lid lag are late signs of long-standing hyperthyroidism. Anisocoria, or unequal pupils, may be caused by blunt trauma, glaucoma, or disruptions in the sympathetic or parasympathetic nerve supply to the irises through cranial nerve III. Development disorders usually account for dysconjugate gaze in childhood, whereas acquired cranial nerve palsies from infections, neurologic diseases, or trauma tend to be the cause in adults. Ptosis usually results from a cranial nerve III palsy, and nystagmus is seen in cerebellar and vestibular disorders.
Skip to...
Videos from this collection:

Now Playing
Eye Exam
Physical Examinations II
75.8K Views

Ophthalmoscopic Examination
Physical Examinations II
66.7K Views

Ear Exam
Physical Examinations II
53.7K Views

Nose, Sinuses, Oral Cavity and Pharynx Exam
Physical Examinations II
64.6K Views

Thyroid Exam
Physical Examinations II
103.5K Views

Lymph Node Exam
Physical Examinations II
381.1K Views

Abdominal Exam I: Inspection and Auscultation
Physical Examinations II
200.6K Views

Abdominal Exam II: Percussion
Physical Examinations II
245.5K Views

Abdominal Exam III: Palpation
Physical Examinations II
137.5K Views

Abdominal Exam IV: Acute Abdominal Pain Assessment
Physical Examinations II
66.4K Views

Male Rectal Exam
Physical Examinations II
112.5K Views

Comprehensive Breast Exam
Physical Examinations II
85.5K Views

Pelvic Exam I: Assessment of the External Genitalia
Physical Examinations II
299.7K Views

Pelvic Exam II: Speculum Exam
Physical Examinations II
148.2K Views

Pelvic Exam III: Bimanual and Rectovaginal Exam
Physical Examinations II
145.4K Views
Copyright © 2025 MyJoVE Corporation. All rights reserved