Aby wyświetlić tę treść, wymagana jest subskrypcja JoVE. Zaloguj się lub rozpocznij bezpłatny okres próbny.
Method Article
Manual Muscle Testing: A Method of Measuring Extremity Muscle Strength Applied to Critically Ill Patients
W tym Artykule
Podsumowanie
Survivors of acute respiratory distress syndrome (ARDS) and critical illness frequently develop long-lasting muscle weakness. Manual muscle testing (MMT) is a standardized clinical examination commonly used to measure strength of peripheral skeletal muscle groups. This video demonstrates MMT using the 6-point Medical Research Council scale.
Streszczenie
Survivors of acute respiratory distress syndrome (ARDS) and other causes of critical illness often have generalized weakness, reduced exercise tolerance, and persistent nerve and muscle impairments after hospital discharge.1-6 Using an explicit protocol with a structured approach to training and quality assurance of research staff, manual muscle testing (MMT) is a highly reliable method for assessing strength, using a standardized clinical examination, for patients following ARDS, and can be completed with mechanically ventilated patients who can tolerate sitting upright in bed and are able to follow two-step commands. 7, 8
This video demonstrates a protocol for MMT, which has been taught to ≥43 research staff who have performed >800 assessments on >280 ARDS survivors. Modifications for the bedridden patient are included. Each muscle is tested with specific techniques for positioning, stabilization, resistance, and palpation for each score of the 6-point ordinal Medical Research Council scale.7,9-11 Three upper and three lower extremity muscles are graded in this protocol: shoulder abduction, elbow flexion, wrist extension, hip flexion, knee extension, and ankle dorsiflexion. These muscles were chosen based on the standard approach for evaluating patients for ICU-acquired weakness used in prior publications. 1,2.
Protokół
1. Introduction
During manual muscle testing (MMT), each muscle group is tested bilaterally. For demonstration purposes, only one side is tested in this video for each of the 6 muscle groups. One hand of the examiner applies resistance or palpates the muscle or tendon for contraction while the other hand stabilizes the extremity being tested to keep it in the test position. The test is repeated if the patient does not understand the instructions or is not applying maximum effort.
2. Grading follows the Medical Research Council (MRC) system (Table 1).1
Figure 1 illustrates an algorithm for the MRC muscle strength scoring system. If the subject is missing a limb, has a cast, or is unable to be placed in the correct testing position, muscle strength is graded as "unable to assess". If the patient has a fixed contracture, but can otherwise perform the test, the muscle is graded. Medical devices, such as catheters and drains, and mechanical ventilation usually do not impede muscle testing, unless a joint is immobilized to ensure proper functioning of a device.
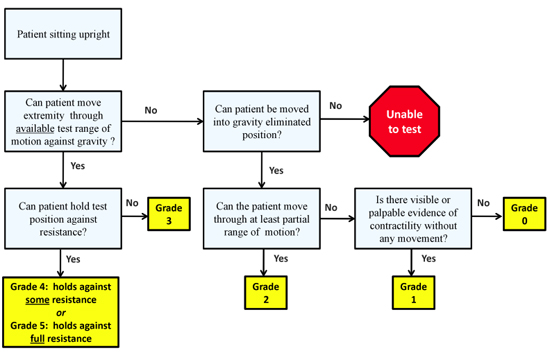
Figure 1. Manual Muscle Testing Algorithm
3. Procedure
- For each muscle tested, the examiner stands to the side being tested, and the patient is sitting upright and positioned to allow full movement of the joint against gravity. The examiner demonstrates the desired movement against gravity. The examiner then requests the patient to repeat the motion.
- If the patient can move through the desired range of motion against gravity, the examiner attempts to apply resistance in the testing position while stating "Hold it, don't let me push it down" or "Hold it, don't let me bend it" (Figure 2). If the patient tolerates no resistance, the muscle score is Grade 3. If the patient tolerates some resistance, the score is Grade 4, and full resistance, Grade 5.
- If the patient cannot move against gravity, the patient is repositioned to allow movement of the extremity with gravity eliminated. If supporting the limb, the examiner provides neither assistance nor resistance to the patient's voluntary movement. This gravity-eliminated positioning will vary for each muscle tested. If the patient cannot complete at least partial range of motion with gravity eliminated, the muscle or tendon is observed and/or palpated for contraction.
- For a bedridden patient who cannot sit up in a bed placed in the chair position or on the edge of the bed, alternate positions for testing the lower extremity are included in this protocol.
4. Shoulder Abduction
- Testing position - arm out from the side at shoulder level. The examiner demonstrates the motion, then states "Lift your arm out to the side to shoulder level." The hand giving resistance is contoured over the patient's arm just above the elbow. The other hand stabilizes the shoulder above the shoulder joint. The examiner states "Hold it, don't let me push it down." To assess grades 3, 4, or 5, please see section 3.2 above.
- If weaker than Grade 3, the patient lies supine with arms at the side. The examiner supports the arm just above the elbow and at the wrist to assure that the shoulder does not externally rotate (turn outward). The patient attempts to move the arm out to the side. The examiner states: "Try to move your arm out to the side". Grade 2 is assigned if the patient moves with gravity eliminated.
- If weaker than Grade 2, the examiner states " Try to move your arm out to the side " and palpates the middle deltoid muscle, as demonstrated, for contraction, and scores as Grade 1 or 0 as previously defined.
- Shoulder MMT can be performed with central venous catheters (e.g., subclavian and jugular) in place, including those used for dialysis. (Figure 2)
The remaining assessments will be completed similarly to above using specific test positions for the patient and examiner, and specific instructions for the patient's movement.
5. Elbow Flexion
- Test position - forearm supinated and flexed slightly more than 90 degrees. Verbal instructions: "Bend your elbow slightly more than 90 degrees". The hand giving resistance is contoured over the flexor surface of the forearm proximal to the wrist. The examiner's other hand applies counterforce by cupping the palm over the anterior superior aspect of the shoulder. The examiner then states: "Hold it. Don't let me push it down" and scores Grades 3, 4, or 5 as previously described.
- If weaker than Grade 3, the shoulder is abducted to 90 degrees. The examiner supports the arm under the elbow and, if necessary, the wrist as well. The forearm is turned with the thumb facing the ceiling. With the elbow extended, the patient attempts to flex the elbow. The examiner states: "Try to bend your elbow." Grade 2 is assigned if the patient can flex the elbow.
- If weaker than Grade 2, the forearm is supinated and positioned at the side in approximately 45 degrees of elbow flexion. The examiner states "Try to bend your elbow", palpates the biceps tendon and scores as either Grade 1 or 0.
6. Wrist Extension
- Test position - arm at the side, elbow flexed to 90 degrees with the forearm pronated and the wrist fully extended. Verbal instructions: "Bend your wrist up as far as possible." The examiner's hand giving resistance is placed over the back of the patient's hand just distal to the wrist. The examiner's other hand supports the patient's forearm. The examiner then states: "Hold it. Don't let me push it down" and scores Grades 3, 4 or 5.
- If weaker than Grade 3, the elbow is flexed to 90 degrees and forearm turned with thumb facing the ceiling. The forearm and wrist are supported by the examiner. The examiner states: "Bend your hand toward me". Grade 2 is assigned if the patient can extend the wrist.
- If weaker than Grade 2, the examiner states "Bend your wrist toward me" and palpates the two extensor tendons, one on each side of the wrist, as demonstrated, and scores as Grade 1 or 0. The examiner is careful not to palpate the tendons in the middle of the wrist.
- This test is not performed if there is an ipsilateral radial arterial catheter in place.
7. Hip Flexion
- Test position - sitting with the hip fully flexed and knee bent. The patient may place their hands on the bed or table for stability. Verbal instructions: "Raise your knee up as high as it will go." The examiner's hand giving resistance is placed on top of the thigh just proximal to the knee. The other hand provides stability at the side of the hip. The examiner then states: "Hold it. Don't let me push it down" and scores Grades 3, 4 or 5.
- If weaker than Grade 3, the patient lays down on the side not being tested. For example, the patient lays on the right side to test the left hip. The examiner stands behind the patient with one arm cradling the leg being tested with the hand supporting under the knee. The opposite hand maintains alignment of the trunk at the hip. The examiner states:"Bring your knee toward your chest." Grade 2 is assigned if the patient can flex the hip.
- If weaker than Grade 2, the patient is supine. The examiner asks, "May I touch your leg here?" (pointing to the inner aspect of the hip joint). With the patient's permission, the examiner states "Bend your hip" and palpates the iliopsoas tendon, as demonstrated, and scores as Grade 1 or 0.
- In a bedridden patient, grades 5, 4, and 3 are tested with the bed in the chair position, or the head of the bed elevated as far as possible. Pillows are placed under the knee to flex the hip to 90 degrees. The examiner assures that the foot is lifted off the bed when asking the patient to raise the knee off the bed. Grades 2 and 1 are scored as previously described.
- This test can be performed in patients with intact and well secured femoral intravascular catheters.
8. Knee Extension
- Test position - sitting upright with the knee fully extended to 0 degrees. Avoid knee hyperextension. Verbal instructions; "Straighten your knee". The hand giving resistance is contoured on top of the leg just proximal to the ankle. The other hand is placed under the thigh above the knee. The examiner then states "Hold it. Don't let me bend it" and scores Grades 3, 4 or 5.
- If weaker than Grade 3, the patient lays on the non-testing side. The examiner stands behind the patient at knee level. The leg not being tested may be flexed for stability. One arm cradles the leg being tested around the thigh with the hand supporting the underside of the knee. The other hand holds the leg just above the ankle. The examiner states: "Straighten your knee." Grade 2 is assigned if the patient can extend the knee (Figure 3).
- If weaker than Grade 2, the patient is supine and the examiner states:"Push the back of your knee down" or "Tighten your knee cap" and palpates the quadriceps tendon, and scores as Grade 1 or 0.
- For the bedridden patient, in scoring Grades 3, 4,and 5, the patient is positioned in the same manner as for hip flexion and graded as described above for knee extension (Figure 4).
9. Ankle Dorsiflexion
- Test position - sitting, with the heel on floor, foot in full dorsiflexion, and shoes and socks removed. Verbal instructions: "Bend your foot up as far as possible." The toes are relaxed during the test. The hand giving resistance is cupped over the top of the foot proximal to the toes. The other hand is contoured around the front of the leg just proximal to the ankle. The examiner then states "Hold it, don't let me push it down" and scores Grade 3, 4 or 5.
- If weaker than Grade 3, but there is partial range of motion against gravity, assign Grade 2.
- If weaker than Grade 2, palpate the tibialis anterior tendon, and score as Grade 1or 0.
- The bedridden patient is tested supine, with the leg extended and a pillow placed under the knee.
- This test can usually be applied with an intact and secured pedal intravascular catheter. Be careful not to dislodge the catheter.
10. Representative Results:
MMT using this protocol has excellent inter-rater reliability when applied with both ARDS survivors and simulated patents. Quality assurance of 19 trainees examining 12 muscle groups demonstrated an intraclass correlation coefficient (95% confidence interval [CI]) of 0.99 (0.97-1.00).8 Agreement (kappa; 95% CI) for detecting clinically significant weakness (i.e., composite MRC score <80% of maximum) was 1.00 (0.55-1.00). Previous studies have shown high inter-rater reliability with stroke, amyotrophic lateral sclerosis (ALS), Guillain-Barre, and other critically ill patients.12-14

Figure 2. ICU patient with a left shoulder abduction contracture. MMT with a left radial arterial line, cardiac monitoring, and continuous dialysis through a right internal jugular catheter. The patient is positioned for shoulder abduction MMT Grades 3, 4 and 5.

Figure 3. ICU bedridden patient with a right internal jugular catheter for continuous dialysis. The patient is positioned on the right side for knee extension MMT Grade 2.

Figure 4. ICU bedridden patient with a left knee flexion contracture. The patient is positioned supine with a pillow under the knee for knee extension MMT Grades 3, 4 and 5.
| Table 1. Manual Muscle Test 3 | |
| Grade | Manual Muscle Test |
| 5 | Movement against gravity plus full resistance |
| 4 | Movement against gravity plus some resistance |
| 3 | Completes the available test range of motion against gravity, but tolerates no resistance |
| 2 | The patient completes full or partial range of motion with gravity eliminated |
| 1 | Slight contractility without any movement |
| 0 | No evidence of contractility (complete paralysis) |
Dyskusje
Depending on the diagnostic criteria, 9 – 87% of ICU patients develop neuromuscular complications, which are associated with prolonged mechanical ventilation, increased hospital stay and rehabilitation time, and potentially associated with increased mortality.1,2,16-18 Periodic reassessment of muscle strength, using a reliable method which minimizes inter-rater variability is helpful to detect changes over time. An important limitation of MMT using the MRC score system is the 6-point ordinal scale. M...
Ujawnienia
No conflicts of interest declared.
Podziękowania
Supported by NIH grant # R01HL088045. Drs. Eddy Fan and Michelle Kho are each supported by a Fellowship Award from the Canadian Institutes of Health Research.
Odniesienia
- De Jonghe, B. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 288, 2859-2867 (2002).
- Ali, N. A. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 178, 261-268 (2008).
- Angel, M. J., Bril, V., Shannon, P., Herridge, M. S. Neuromuscular function in survivors of the acute respiratory distress syndrome. Can. J. Neurol. Sci. 34, 427-432 (2007).
- Cheung, A. M. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 174, 538-544 (2006).
- Stevens, R. D. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 33, 1876-1891 (2007).
- Herridge, M. S. One-year outcomes in survivors of the acute respiratory distress syndrome. N. Engl. J. Med. 348, 683-693 (2003).
- Medical Research Council. . Aids to the Investigation of the Peripheral Nervous System. , (1976).
- Fan, E. Inter-rater reliability of manual muscle strength testing in ICU survivors and simulated patients. Intensive Care Med. 34, 1038-1043 (2010).
- Hislop, H. J., Montgomery, J. M. . Daniels and Worthingham's Muscle Testing. , (2007).
- Reese, N. B. . Muscle and Sensory Testing. , (2005).
- Kendall, F. P. . Muscles; Testing and Function with Posture and Pain. , (2005).
- Lieu, B. K., Hough, C. L. Assessment of Weakness in Critically Ill Patients Using Physical Examination. Am J Respir Crit Care Med. 175, A218-A218 (2007).
- Gregson, J. M. Reliability of measurements of muscle tone and muscle power in stroke patients. Age Ageing. 29, 223-228 (2000).
- Great Lakes ALS Study Group. . A comparison of muscle strength testing techniques in amyotrophic lateral sclerosis. Neurology. 61, 1503-1507 (2003).
- Kleyweg, R. P., van der Meche, F. G., Schmitz, P. I. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barre syndrome. Muscle Nerve. 14, 1103-1109 (1991).
- Zink, W., Kollmar, R., Schwab, S. Critical illness polyneuropathy and myopathy in the intensive care unit. Nat. Rev. Neurol. 5, 372-379 (2009).
- Sharshar, T. Presence and severity of intensive care unit-acquired paresis at time of awakening are associated with increased intensive care unit and hospital mortality. Crit. Care Med. 37, 3047-3053 (2009).
- Griffiths, R. D., Hall, J. B. Intensive care unit-acquired weakness. Crit. Care Med. 38, 779-787 (2010).
- Bohannon, R. W. Measuring knee extensor muscle strength. Am J Phys Med Rehabil. 80, 13-18 (2001).
- Needham, D. M. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 300, 1685-1690 (2008).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone