Pelvic Exam II: Speculum Exam
Обзор
Source:
Alexandra Duncan, GTA, Praxis Clinical, New Haven, CT
Tiffany Cook, GTA, Praxis Clinical, New Haven, CT
Jaideep S. Talwalkar, MD, Internal Medicine and Pediatrics, Yale School of Medicine, New Haven, CT
Providing comfortable speculum placement is an important skill for providers to develop, since the speculum is a necessary tool in many gynecological procedures. Patients and providers are often anxious about the speculum exam, but it is entirely possible to place a speculum without patient discomfort. It's important for the clinician to be aware of the role language plays in creating a comfortable environment; for instance, a provider should refer to the speculum "bills" rather than "blades" to avoid upsetting the patient.
There are two types of speculums: metal and plastic (Figure 1). This demonstration utilizes plastic, as plastic speculums are most commonly used in clinics for routine testing. When using a metal speculum, it's recommended to use a Graves speculum if the patient has given birth vaginally, and a Pederson speculum if the patient has not. Pederson and Graves speculums are different shapes, and both come in many different sizes (medium is used most often). Prior to placing a metal speculum, it is helpful to perform a digital cervical exam to assess for the appropriate speculum size. The depth and direction of the cervix is estimated by placing one finger into the vagina. If the patient's cervix can be located while the patient is seated, it is likely that the patient has a shallow vagina, and therefore should be most comfortable with a short metal speculum.

Figure 1. A photograph of commercially available speculums in different sizes.
Plastic speculums are all shaped like Pederson metal speculums and come in different sizes. To assess the appropriate size for a plastic speculum, the examiner places two fingers in the patient's vagina, palm down, and tries to separate the fingers: if there is no space between the fingers, a small plastic speculum should be used; if there is space between the fingers, a medium one should be used. The exam should never be performed with a large speculum (as it is significantly longer) without first determining the length of the vaginal canal.
The speculum is used to perform the Papanicolaou test as part of cervical cancer screening examinations. Cervical cancer was once the leading cause of cancer deaths for women in the United States, but in recent decades the number of cases and deaths has declined significantly1. This change is credited to the discovery made by Georgios Papanicolaou in 1928 that cervical cancer could be diagnosed by vaginal and cervical smears. The Pap test, as it is now called, detects abnormal cells in the cervix, both cancerous and pre-cancerous. Current guidelines for recommended screening intervals can be found through the U.S. Preventive Services Task Force (USPSTF) website2.
The test can be performed using either 1) a conventional glass slide and fixative with a spatula and endocervical brush (the traditional "Pap smear") or 2) the more commonly utilized liquid-based cytology with a cervical broom or a spatula and endocervical brush (Figure 2). No matter what tools are used, the samples are collected from just inside the external os and the squamocolumnar junction, or transition zone around the os (Figure 3). This video demonstrates the spatula and endocervical brush with liquid-based cytology, as the liquid preparation is a more effective technique for the detection of cervical lesions, and the spatula and endocervical brush improve specimen collection.

Figure 2. Pap smear tools. Shown in sequence are: a liquid cytology canister, cervical broom, spatula, and endocervical brush.
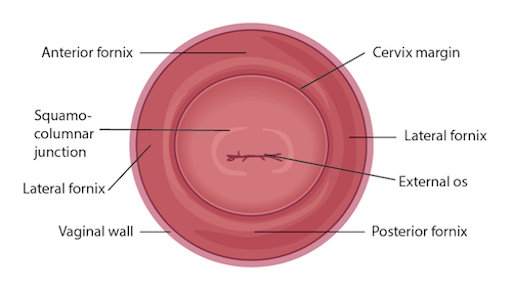
Figure 3. Diagram of the cervix withrelevant structures labeled.
Процедура
The speculum exam begins immediately after the end of the external genitalia exam; therefore, the patient already has provided a history and is in the modified lithotomy position. Make sure the patient is seated at the end of the table, as the speculum cannot be fully inserted any other way.
1. Preparation
- Lay out the supplies for the Pap test.
- Label the liquid cytology canister with the patient's information.
- Unscrew the lid of the canister until it is resting on top and can be lifted off.
- Place the speculum in your non-dominant hand and position your index finger above the bills, your middle finger below the bills, and your thumb on the back of the speculum (Figure 4).
- Use your dominant hand to spread the water-based lubricant (or warm water, otherwise) on the outside of the bills.
- Introduce the speculum and let the patient know what to expect: "This is a speculum. These are the bills, which I will be placing into your vagina to view your cervix and take some samples. This is the handle, which will not be inserted."
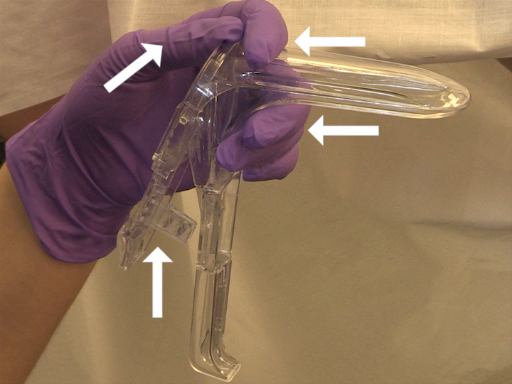
Figure 4. How to hold a plastic speculum.
2. Insertion
- As always, introduce your touch to the patient before beginning the exam.
- Let the patient know you are about to place the back of your hand on the patient's thigh and will then begin the exam.
- Place the back of your hand on the inside of the patient's thigh, over the drape, then begin to examine: this prepares the patient and starts with non-invasive contact, which may help put the patient at ease.
- Using the pads of the index and middle finger of your dominant hand, separate the labia minora just above the perineum to get a clear view of the vaginal introitus.
- Guide the patient through a relaxation technique: "I'm going to teach you how to make this more comfortable for yourself. Please take a deep breath in, and as you exhale, bear down as if you are making a bowel movement. (If the patient doesn't understand this, ask the patient to push against your fingers.)"
- As the patient bears down, the vaginal introitus opens. Let the patient know, "You'll feel me inserting the speculum."
- Smoothly insert the speculum about halfway into the vagina at an oblique angle (roughly 45°), angling the bills below where the cervix is expected to be (based on the digital exam) while maintaining posterior pressure.
- Use the first two fingers of your dominant hand to clear the labia on one side, so the labia are not tugged along with the speculum.
- Use your dominant hand to clear the labia on the other side.
- Bring your non-dominant hand to the bottom handle of the speculum, rotate the speculum flat, and insert fully, until the handle is flush against the patient's pelvis and perpendicular to the floor.
- Place one finger of your dominant hand inside the bills of the speculum, and use the finger to apply strong posterior pressure as your non-dominant hand pulls down on the handle of the speculum at the same time. Apply enough posterior pressure so space in the vagina can be seen above the speculum.
- Place the thumb of your non-dominant hand on the thumb lever, and smoothly depress.
- Do not continue to depress once resistance is met, or you may open the bills too far and cause the patient discomfort.
- Hold the speculum steady and check to see if the cervix has been located.
3. Pap test
- If there is enough discharge on the face of the cervix to obscure the os and interfere with specimen collection, use a large cotton-tipped swab to gently clear excess cervical mucous.
- Use your dominant hand to pick up the spatula (or have the chaperone hand it to you).
- Insert the spatula into the vagina, being careful not to let it touch the walls, until the long end rests in the os and the depression and short end are pressed against the squamocolumnar junction.
- Rotate 360°, maintaining consistent pressure and contact with the exocervix.
- Remove the spatula, being careful not to touch the walls of the vagina.
- Place the spatula into the open canister and thoroughly rinse by swirling vigorously in the liquid (different brands of liquid-based cytology recommend swirling for different lengths of time; be familiar with the manufacturer's recommendation before beginning).
- Discard the spatula, or place it back on the tray.
- Use your dominant hand to pick up the endocervical brush.
- Insert the endocervical brush into the vagina, being careful not to let it touch the walls, and gently insert it into the os until only the bottom bristles are exposed.
- Slowly rotate 180° in one direction. Do not over-rotate.
- If using a cervical broom, rather than an endocervical brush and spatula, insert the broom until the center bristles are in the os and the shorter bristles rest on the squamocolumnar junction, then rotate five full times in one direction before removing.
- Remove the brush, being careful not to touch the walls of the vagina.
- Place the endocervical brush into the open canister and thoroughly rinse by swirling vigorously and pressing it repeatedly against the sides of the canister to release material.
- Discard the endocervical brush.
- Replace and tighten the lid of the cytology canister.
4. Removing the speculum
- Place your non-dominant thumb on the thumb lever and maintain pressure while releasing the locking mechanism.
- Continue to hold the thumb lever down, and remove the speculum to about an inch out to allow the cervix to clear the tip of the bills.
- Completely remove your thumb from the lever and place it on the handle of the speculum.
- Rotate the speculum 45° while smoothly removing it the rest of the way out, allowing the vaginal walls to close the bills.
- Place your dominant hand underneath the speculum to catch any discharge.
- Discard the plastic speculum, if disposable.
Заявка и Краткое содержание
This video reviewed the techniques for performing a comfortable speculum exam and collecting the samples for a Pap test. Before the exam is started, the examiner should ensure all supplies are prepared and let the patient know what to expect. Being able to perform a comfortable speculum exam is an important skill for any practitioner, as it is used in a wide variety of gynecological procedures and can provide a wealth of information. When the speculum is inserted, it is possible to observe the cervix and vaginal walls for a variety of signs including tone, color, discharge, lesions, polyps, ulcerations, and more-all of which may be clinically significant and can help with the process of diagnosis. A well-inserted speculum also allows easy access to the cervical os, at which point samples may be taken for the Pap test (as well as for other screenings, like chlamydia and gonorrhea). It's necessary to use a speculum to access the cervix for many other procedures, including inserting or removing an intrauterine device (IUD), a loop electrosurgical excision procedure (LEEP), and more.
Many patients may feel anxiety about the speculum and experience it as the most invasive part of the gynecological exam. The provider can offer the patient general support and empathy, along with specific tools to make the exam more comfortable for themselves. Asking the patient to take a deep breath and then bear down as if having a bowel movement before insertion can open the vaginal introitus and greatly aid comfort. The examiner may offer a particularly anxious patient the opportunity to insert the speculum themselves by placing it upside-down with the handle pointing toward the ceiling as the provider talks them through opening it3. It is often easier to get a clear view of the cervix with an upside-down insertion, but it is not a technique practitioners should employ, because it places the examiner's hand directly against the patient's clitoris.
There are many things the practitioner can do to ensure the exam is comfortable. The speculum should be inserted at an oblique angle to avoid putting too much direct pressure on the urethra. When the speculum is inserted fully, the bills should be angled below where the cervix was located during the digital exam. The practitioner can then apply enough posterior pressure to the speculum, so there is space visible in the vagina over the bills; this allows the bills to be opened without putting pressure on the delicate anterior structures. The most important thing is to never insert or remove a speculum while the bills are open. This is very painful and risks injuring the patient. The examiner should not touch the thumb lever until the speculum is positioned fully and ready to be opened. The lock on the speculum should be released fully before removal, and any pressure maintained manually. Once the cervix is free, the thumb lever should be completely released and the speculum smoothly removed the rest of the way, allowing the vaginal walls to close the bills on the way out.
Ссылки
- Cervical Cancer Statistics. U.S. Preventive Services Task Force. Centers for Disease Control and Prevention (2014).
- Cervical Cancer: Screening. Recommendation Summary. U.S. Preventive Services Task Force (2012).
- Wright, D., Fenwick, J., Stephenson, P., Monterosso, L. Speculum 'self-insertion': a pilot study. Journal of Clinical Nursing. 14(9): 1098-1111 (2005).
Теги
Перейти к...
Видео из этой коллекции:

Now Playing
Pelvic Exam II: Speculum Exam
Physical Examinations II
150.4K Просмотры

Eye Exam
Physical Examinations II
77.1K Просмотры

Ophthalmoscopic Examination
Physical Examinations II
67.9K Просмотры

Ear Exam
Physical Examinations II
55.1K Просмотры

Nose, Sinuses, Oral Cavity and Pharynx Exam
Physical Examinations II
65.7K Просмотры

Thyroid Exam
Physical Examinations II
105.0K Просмотры

Lymph Node Exam
Physical Examinations II
387.3K Просмотры

Abdominal Exam I: Inspection and Auscultation
Physical Examinations II
202.6K Просмотры

Abdominal Exam II: Percussion
Physical Examinations II
248.2K Просмотры

Abdominal Exam III: Palpation
Physical Examinations II
138.5K Просмотры

Abdominal Exam IV: Acute Abdominal Pain Assessment
Physical Examinations II
67.3K Просмотры

Male Rectal Exam
Physical Examinations II
114.4K Просмотры

Comprehensive Breast Exam
Physical Examinations II
87.6K Просмотры

Pelvic Exam I: Assessment of the External Genitalia
Physical Examinations II
306.9K Просмотры

Pelvic Exam III: Bimanual and Rectovaginal Exam
Physical Examinations II
147.7K Просмотры
Авторские права © 2025 MyJoVE Corporation. Все права защищены