A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Minimal Erythema Dose (MED) Testing
In This Article
Summary
This article describes how to conduct minimal erythema dose (MED) testing in order to determine the lowest dose of ultraviolet radiation that will cause erythema (burning) when administered to an individual.
Abstract
Ultraviolet radiation (UV) therapy is sometimes used as a treatment for various common skin conditions, including psoriasis, acne, and eczema. The dosage of UV light is prescribed according to an individual's skin sensitivity. Thus, to establish the proper dosage of UV light to administer to a patient, the patient is sometimes screened to determine a minimal erythema dose (MED), which is the amount of UV radiation that will produce minimal erythema (sunburn or redness caused by engorgement of capillaries) of an individual's skin within a few hours following exposure. This article describes how to conduct minimal erythema dose (MED) testing. There is currently no easy way to determine an appropriate UV dose for clinical or research purposes without conducting formal MED testing, requiring observation hours after testing, or informal trial and error testing with the risks of under- or over-dosing. However, some alternative methods are discussed.
Protocol
1. Preparing for UV Exposure
- Explain to the participant how MED testing works ("I'm going to expose some skin on your arm to UV light over the course of about 20 min, and tomorrow, we're going to check that section of your skin in order to determine how sensitive you are to the light. You may experience a sunburn in the small areas that we expose to UV. If the sunburn is painful or bothers you, you can treat it like you would any other sunburn.")
- Staff and participant should wear UV protective glasses.
- The participant should be wearing a short-sleeved shirt or roll her sleeve up.
- Have the participant put on a glove to protect the skin on her hand.
- Remove the Daavlin patch1 backing on the left and right sides of the patch, and place it on the inner lower arm just adjacent to the glove, avoiding any existing skin blemishes.
- Cover any additional skin on the arm with the participant's shirt or other material.
- Place the arm so that the holes in the patch will be exposed to the UV light source. No other skin should be exposed to the UV light.
- Tell the participant she will feel warmth but her arm will not be burning during the test.
2. Conducting UV Exposure
- Patch holes (e.g. 6) should be exposed to UV at intervals throughout the exposure period.
- Start with hole 1 open.
- Select the total duration of the exposure based on the manufacturer specifications for the light source and the participant's Fitzpatrick skin type I-VI (very fair to very dark; Fitzpatrick, 1988).2 Fairer skin is more likely to burn.
- Set a timer for the total duration of exposure (e.g. 20 min). A second backup timer may also be used. Start the timer(s).
- For example, open hole 2 after 2 min, open hole 3 after 4 min, open hole 4 after 8 min, open hole 5 after 12 min, and open hole 6 after 16 min. Thus, the skin UV exposure times will be 20 min for hole 1, 18 min for hole 2, 16 min for hole 3, 12 min for hole 4, 8 min for hole 5, and 4 min for hole 6.
- In order to more easily identify the exposed areas after 24-48 hr, mark the skin exposed on the far edge of the first and last holes of the patch and ask the participant to not wash off the marks until after the skin is examined.
- Have the participant remove the glove and patch.
- Reiterate to the participant that the skin must be reexamined in 24-48 hr.
3. Assessing the MED
- After 24-48 hr, examine the exposed areas of skin. Red or pink skin indicates erythema or burning. Erythemetous skin exposed to the shortest duration of UV is defined as the minimal erythema dose or MED.
- Future exposures to UV should be for durations shorter than the MED to avoid burning.
- If the areas of exposure are difficult to identify, you may want to put the patch back on using the marks to align with the exposed skin. This is also helpful if using a skin color measurement device such as a spectrophotometer.
- Spectrophotometers provide measures of L* (darkness) and b* (hue). a* refers to the redness of the skin. A higher a* value indicates redder skin.
- If using a skin color measurement device such as a spectrophotometer, place the spectrophotometer aperture in the center of the hole to be measured.
- Measure each of the 6 exposure areas in numerical order and one unexposed area near the others for comparison. Try to measure the center of each hole but not a freckle or mole or other non-UV discolorations. Label each of the measurements. The measurement from the unexposed area should be labeled 0 min and be listed next to area 6 (the shortest exposure area - 4 min).
- Increases in a* values should correspond with increases in UV exposure duration. Try re-measuring values that are not in corresponding order.
- A 2.5 point difference in the a* of unexposed skin compared to exposed skin indicates a significant difference in redness, suggesting potential burning.
- Add 2.5 to the lowest a* value. Anything at or above this value would be considered potentially burning. The lowest exposure time above this value is considered the MED.
Results
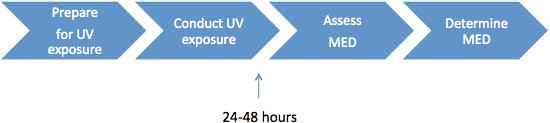
Figure 1. The four steps of conducting MED testing: preparing for UV exposure, conducting UV exposure, assessing the MED, and determining the MED.

Discussion
Ultraviolet radiation (UV) therapy is sometimes used as a treatment for various common skin conditions, including psoriasis, acne, and eczema. The dosage of UV light is prescribed according to an individual's skin sensitivity, which is determined as a function of the individual's Fitzpatrick skin type I through VI (very fair to very dark).2 Human skin varies in its sensitivity to UV radiation because of varying degrees of skin pigmentation, thickness, and other factors. Thus, to establish the proper dosage of ...
Disclosures
We have nothing to disclose.
Acknowledgements
This work was funded by R21CA134819 (CH), T32CA009035 (SD),and P30CA006927 (Cancer Center Core Grant). The authors would like to thank Elizabeth Culnan for her assistance with participant recruitment, Lia Boyle, Eva Panigrahi, and Kate Menezes for their assistance in the development of procedures, and Jeanne Pomenti with her assistance with manuscript preparation. We also thank the journal reviewers for their helpful suggestions.
References
- Fitzpatrick, T. B. The validity and practicality of sun-reactive skin types I through VI. Archives of Dermatology. 124, 869-871 (1988).
- Bodekaer, M., Akerstrom, U., Wulf, H. C. Accumulation of sunscreen in human skin after daily applications: a study of sunscreens with different ultraviolet radiation filters. Photodermatol. Photoimmunol. Photomed. 28, 127-132 (2012).
- Kwon, I. H., Kwon, H. H., Na, S. J., Youn, J. I. Could colorimetric method replace the individual minimal erythemal dose (MED) measurements in determining the initial dose of narrow-band UVB treatment for psoriasis patients with skin phototype III-V?. J. Eur. Acad. Dermatol. Venereol. , (2012).
- Youn, J. I., Park, J. Y., Jo, S. J., Rim, J. H., Choe, Y. B. Assessment of the usefulness of skin phototype and skin color as the parameter of cutaneous narrow band UVB sensitivity in psoriasis patients. Photodermatol. Photoimmunol. Photomed. 19, 261-264 (2003).
- Henriksen, M., Na, R., Agren, M. S., Wulf, H. C. Minimal erythema dose after multiple UV exposures depends on pre-exposure skin pigmentation. Photodermatol. Photoimmunol. Photomed. 20, 163-169 (2004).
- Kraemer, C. K., Menegon, D. B., Cestari, T. F. Determination of the minimal phototoxic dose and colorimetry in psoralen plus ultraviolet A radiation therapy. Photodermatol. Photoimmunol. Photomed. 21, 242-248 (2005).
- Sachdeva, S. Fitzpatrick skin typing: applications in dermatology. Indian J. Dermatol. Venereol. Leprol. 75, 93-96 (2009).
- Webb, A. R., Kift, R., Berry, J. L., Rhodes, L. E. The vitamin D debate: translating controlled experiments into reality for human sun exposure times. Photochem. Photobiol. 87, 741-745 (2011).
- Otman, S. G., Edwards, C., Gambles, B., Anstey, A. V. Validation of a semiautomated method of minimal erythema dose testing for narrowband ultraviolet B phototherapy. Br. J. Dermatol. 155, 416-421 (2006).
- Taylor, D. K., Anstey, A. V., Coleman, A. J., Diffey, B. L., Farr, P. M., Ferguson, S., et al. Guidelines for dosimetry and calibration in ultraviolet radiation therapy: a report of a British Photodermatology Group workshop. Br. J. Dermatol. 146, 755-763 (2002).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved