Aby wyświetlić tę treść, wymagana jest subskrypcja JoVE. Zaloguj się lub rozpocznij bezpłatny okres próbny.
Method Article
Quantification of Global Diastolic Function by Kinematic Modeling-based Analysis of Transmitral Flow via the Parametrized Diastolic Filling Formalism
W tym Artykule
Podsumowanie
Accurate, causality-based quantification of global diastolic function has been achieved by kinematic modeling-based analysis of transmitral flow via the Parametrized Diastolic Filling (PDF) formalism. PDF generates unique stiffness, relaxation, and load parameters and elucidates 'new' physiology while providing sensitive and specific indexes of dysfunction.
Streszczenie
Quantitative cardiac function assessment remains a challenge for physiologists and clinicians. Although historically invasive methods have comprised the only means available, the development of noninvasive imaging modalities (echocardiography, MRI, CT) having high temporal and spatial resolution provide a new window for quantitative diastolic function assessment. Echocardiography is the agreed upon standard for diastolic function assessment, but indexes in current clinical use merely utilize selected features of chamber dimension (M-mode) or blood/tissue motion (Doppler) waveforms without incorporating the physiologic causal determinants of the motion itself. The recognition that all left ventricles (LV) initiate filling by serving as mechanical suction pumps allows global diastolic function to be assessed based on laws of motion that apply to all chambers. What differentiates one heart from another are the parameters of the equation of motion that governs filling. Accordingly, development of the Parametrized Diastolic Filling (PDF) formalism has shown that the entire range of clinically observed early transmitral flow (Doppler E-wave) patterns are extremely well fit by the laws of damped oscillatory motion. This permits analysis of individual E-waves in accordance with a causal mechanism (recoil-initiated suction) that yields three (numerically) unique lumped parameters whose physiologic analogues are chamber stiffness (k), viscoelasticity/relaxation (c), and load (xo). The recording of transmitral flow (Doppler E-waves) is standard practice in clinical cardiology and, therefore, the echocardiographic recording method is only briefly reviewed. Our focus is on determination of the PDF parameters from routinely recorded E-wave data. As the highlighted results indicate, once the PDF parameters have been obtained from a suitable number of load varying E-waves, the investigator is free to use the parameters or construct indexes from the parameters (such as stored energy 1/2kxo2, maximum A-V pressure gradient kxo, load independent index of diastolic function, etc.) and select the aspect of physiology or pathophysiology to be quantified.
Wprowadzenie
Pioneering studies by Katz1 in 1930 revealed that the mammalian left ventricle initiates filling by being a mechanical suction pump, and much effort since then has been devoted to unraveling the workings of diastole. For many years, invasive methods were the only options available for clinical or research assessment of diastolic function (DF)2-16. In the 1970s, however, technical advancements and developments in echocardiography finally gave cardiologists and physiologists practical tools for noninvasive characterization of DF.
Without a unifying causal theory or paradigm for diastole regarding how the heart works when it fills, researchers proposed numerous phenomenologic indexes based on correlation with clinical features. The curvilinear, rapidly rising and falling shape of the transmitral blood flow velocity contour during early, rapid filling, for example, was approximated as a triangle and diastolic function indexes were defined from geometric features (height, width, area, etc.) of that triangle. Technical advancements in echocardiography have allowed tissue motion, strain, and strain rate during filling to be measured, for example, and each technical advancement brought with it a new crop of phenomenological indexes to be correlated with clinical features. However, the indexes remain correlative and not causal and many indexes are different measures of the same underlying physiology. It’s not surprising, therefore, that currently employed clinical indexes of DF have limited specificity and sensitivity.
To overcome these limitations the Parametrized Diastolic Filling (PDF) formalism, a causal kinematic, lumped parameter model of left ventricular filling that is motivated by and incorporates the suction-pump physiology of diastole was developed and validated17. It models diastolic function (as manifested by the curvilinear shapes of transmitral flow contours) in accordance with the rules of damped harmonic oscillatory motion. The equation for damped harmonic oscillatory motion is based on Newton’s Second Law and can be written, per unit mass, as:
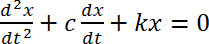 Equation 1
Equation 1
This linear 2nd order differential equation has three parameters: k- chamber stiffness, c- viscoelasticity/relaxation, and xo- the oscillator’s initial displacement/preload. The model predicts that the different clinically observed diastolic filling patterns are the result of variation in the numerical value of these three model parameters. Based on the PDF formalism and classical mechanics, E-waves can be classified as being determined by under-damped or over-damped regimes of motion. Numerous studies17-21 have validated that clinically recorded E-wave contours and PDF model predicted contours show superb agreement and have elucidated the hemodynamic/physiologic analogues of the three PDF parameters21. The process for extracting model parameters from clinically recorded E-wave data is detailed in the methods below.
Unlike typical indexes of DF in current clinical use, the PDF model’s three parameters are causality based. As discussed in the methods below, additional indexes of diastolic physiology can be derived from these fundamental parameters and from application of the PDF formalism to aspects of diastole other than transmitral flow. In this work, methods of PDF-based analysis of transmitral flow and the physiologic relations that can be drawn from the PDF approach, its parameters and the derived indexes are described. Additionally, it is shown that the PDF parameters or indexes derived from them can tease apart intrinsic chamber properties from the external effects of load can provide correlates to traditional invasively defined parameters and can differentiate between normal and pathologic groups.
Access restricted. Please log in or start a trial to view this content.
Protokół
The procedure for acquiring echocardiographic images and analyzing them to obtain the PDF parameters is detailed below. Although cardiac catheterization is mentioned in the subject selection portion below, the methodology described applies only to the echocardiographic portion. The description of the catheterization portion was included for independent validation of model based predictions and is unrelated to the analysis of E-waves via the PDF formalism. Prior to data acquisition, all subjects provide signed, informed consent for participation in the study in accordance with the Institutional Review Board (Human Research Protection Office) at Washington University School of Medicine.
NOTE: All software programs (along with tutorials on how to use them) described in this section can be downloaded from http://cbl1.wustl.edu/SoftwareAgreement.htm
1. Subject Selection
NOTE: All subjects in the Cardiovascular Biophysics Laboratory Database had simultaneous echocardiography and cardiac catheterization performed and were referred by their physicians for diagnostic cardiac catheterization. The database inclusion criteria are: 1) absence of any significant valvular abnormalities, 2) absence of wall motion abnormalities or bundle branch block on ECG, 3) presence of a satisfactory echocardiographic window with clearly identifiable E- and A-waves.
2. Echocardiographic Data Acquisition
- Record a complete 2D/echo-Doppler study for all subjects in accordance with American Society of Echocardiography criteria16. NOTE: The screening echocardiograms were recorded on a standard clinical imager by a sonographer. If desired, additional transthoracic echocardiographic recording can be performed for verification purposes after a suitable, high fidelity catheter is advanced into the LV to measure LV hemodynamics simultaneously.
- Image subjects in the supine position. In a nonresearch setting, standard left lateral positioning can be used without loss of generality of the method. Obtain apical four-chamber views using a 2.5 MHz transducer, with the sample volume gated at 1.5-5 mm directed between the tips of the mitral valve leaflets and orthogonal to the MV plane (to minimize alignment effects as seen on color M-mode Doppler), the wall filter set at 1 (125 Hz) or 2 (250 Hz), the baseline adjusted to take advantage of the full height of the display and the velocity scale adjusted to exploit the dynamic range of the output without aliasing.
- Perform Doppler tissue imaging with the sample volume gated at 2.5 mm and positioned at the lateral and septal potions of the mitral annulus.
- Save Doppler examinations in DICOM format in the echo machine and record on DVD with simultaneously recorded electrocardiogram (ECG).
3. Doppler Image Processing and Conventional Analysis
NOTE: This section describes two custom MATLAB programs. The first program is described in step 3.1 and the second program is described in steps 3.2-3.5. All software programs (along with tutorials on how to use them) can be downloaded from http://cbl1.wustl.edu/SoftwareAgreement.htm
- Convert images from the DICOM format and video to bitmap (.bmp) files (using a custom MATLAB program). NOTE: The procedure described below to fit Doppler E-waves and tissue Doppler E’-waves is shown in Figure 1.
- Load the bitmap image files on another custom MATLAB program to measure conventional transmitral flow parameters such as Epeak, Apeak, Edur, E’peak, A’peak, etc. and crop the images for PDF analysis. Select images with discernible transmitral flow contour and complete cardiac cycle as indicated by ECG for analysis.
- Mark the time sampling rate (measured in pixels/s on the horizontal axis) and velocity sampling rate (measured in pixels/(m/sec) along the vertical axis) in the images. Identify the complete cardiac cycle by noting and marking consecutive R peaks (or any distinct feature of the ECG) on the image.
- Mark the transmitral Doppler E- and A-wave or tissue Doppler E’- and A’- wave in the selected cardiac cycle.
- Select the Doppler E-wave peak point i.e. Epeak, (or E’peak) and mark the start of the wave using the line connecting the peak to the start as a guide to match the acceleration slope of the E-wave (or E’-wave). The start of the wave is used to calculate the interval from start to peak flow denoted as the E-wave (or E’-wave) acceleration time (AT).
- Mark the end of the E-wave (or E’-wave) using the line connecting the peak to the end as a guide to match the deceleration slope. This is used to calculate the interval from the peak to the baseline denoted as the deceleration time (DT). The interval from start to end of the wave is the duration of the E-wave (Edur = AT+DT). The program guides the user through the entire process with appropriate instructions.
- Mark the A-wave using a similar procedure as the E-wave. With both the E- and A-waves marked the program calculates the Epeak/Apeak ratio.
NOTE: The program saves the marked waves as cropped images containing the E- and A-waves only. The program also creates a data file with the cropping and measured parameters for each beat.
4. Automated Fitting of Transmitral Flow Using the PDF Formalism
- The automated fitting of Doppler E- and A-wave and tissue Doppler E’- and A’- wave contours is done using a custom LabView program18,19.
- Load the cropped image, and the program automatically calculates the maximum velocity envelope (MVE). Select the MVE by setting the threshold such that MVE approximates transmitral flow as shown in Figure 1. The onset and termination of the points that define the MVE can be selected along the time-axis by the operator such that only MVE points that provide good correspondence to the actual selected portion of the wave are used as input for the subsequent fitting.
- NOTE: The user-selected MVE points are the input to the computer program that automatically fits the PDF model solution for velocity as a function of time using a Levenberg- Marquardt (iterative) algorithm. The fitting is accomplished with the requirement that the mean square error between the clinical (input) data (MVE) and the PDF model predicted contour be minimized. Since the model is linear, a unique set of parameters is obtained for each Doppler E-wave derived MVE used as input. Thus numerically unique k, c, and xo values are generated for each E-wave and k’, c’, and xo’ for each E’-wave.
- In the event the fit is obviously suboptimal when the fit is superimposed on the E-wave (or E’-wave) image (i.e. the algorithm attempted to fit noise included in the MVE for example) modify the MVE by using more/less points, thereby modifying the model predicted contour with consequent modification of PDF parameters to achieve a better fit.
Save the data when the appropriate PDF fit has been generated. NOTE: The program is written to automatically save the data in image and text files containing the PDF parameters and the contour information.
The PDF parameters obtained from the procedure described above can be used to elucidate new physiology and distinguish between normal and pathological physiology as detailed in the Representative Results section below.
Access restricted. Please log in or start a trial to view this content.
Wyniki
Doppler waveforms representative of the four different types of filling patterns (normal, pseudonormal, delayed relaxation, constrictive-restrictive) using the method detailed above are shown in Figure 2. Figure 2A shows the normal pattern, which, by itself is indistinguishable from the pseudonormal pattern. Figure 2B shows a delayed relaxation and Figure 2C shows a constrictive-restrictive pattern associated with severe diastolic dysfunction. For c...
Access restricted. Please log in or start a trial to view this content.
Dyskusje
In keeping with our methodologic focus, the key aspects of the methods that facilitate obtaining accurate and meaningful results are highlighted.
ECHOCARDIOGRAPHY
The American Society of Echocardiography (ASE) has guidelines for the performance of transthoracic studies16. During an echo exam, there are a multitude of factors that affect image quality. Factors that are beyond the control of the sonographer include: technical capabilities of the imager bein...
Access restricted. Please log in or start a trial to view this content.
Ujawnienia
The authors have no competing financial interests.
Podziękowania
This work was supported in part by the Alan A. and Edith L. Wolff Charitable Trust, St. Louis, and the Barnes-Jewish Hospital Foundation. L. Shmuylovich and E. Ghosh were partially supported by predoctoral fellowship awards from the Heartland Affiliate of the American Heart Association. S. Zhu received partial support from the Washington University Compton Scholars Program and the College of Arts and Sciences’ Summer Undergraduate Research Award. S. Mossahebi received partial support from the Department of Physics.
Access restricted. Please log in or start a trial to view this content.
Materiały
| Name | Company | Catalog Number | Comments |
| Philips iE33 | Philips (Andover, MA) | ||
| LabView 6.0 | National Instruments | Version 6.0.2 | |
| MATLAB | MathWorks | Version R2010b |
Odniesienia
- Katz, L. N. The role played by the ventricular relaxation process in filling the ventricle. Am. J. Physiol. 95, 542-553 (1930).
- Frais, M. A., Bergman, D. W., Kingma, I., Smiseth, O. A., Smith, E. R., Tyberg, J. V. The dependence of the time constant of left ventricular isovolumic relaxation on pericardial pressure. Circulation. 81, 1071-1080 (1990).
- Weiss, J. L., Frederiksen, J. W., Weisfeldt, M. L. Hemodynamic determinants of the time-course of fall in canine left ventricular pressure. J. Clin Invest. 58, 751-760 (1976).
- Weisfeldt, M. L., Weiss, J. L., Frederiksen, J. W., Yin, F. C. P. Quantification of incomplete left ventricular relaxation: Relationship to the time constant for isovolumic pressure fall. Eur. Heart J. 1, 119-129 (1980).
- Thompson, D. S., et al. Analysis of left ventricular pressure during isovolumic relaxation in coronary artery disease. Circulation. 65, 690-697 (1982).
- Ludbrook, P. A., Bryne, J. D., Kurnik, P. B., McKnight, R. C. Influence of reduction of preload and afterload by nitroglycerin on left ventricular diastolic pressure-volume relations and relaxation in man. Circulation. 56, 937-943 (1977).
- Tyberg, J. V., Misbach, G. A., Glantz, S. A., Moores, W. Y., Parmley, W. W. A mechanism for shifts in the diastolic, left ventricular, pressure-volume curve: The role of the pericardium. Eur. J. Cardiol. 7, 163-175 (1978).
- Suga, H. Theoretical analysis of a left-ventricular pumping model based on the systolic time-varying pressure/volume ratio. IEEE Trans. Biomed. Eng. 24, 29-38 (1977).
- Raff, G. L., Glantz, S. A. Volume loading slows left ventricular isovolumic relaxation rate. Circ. Res. 48, 813-824 (1981).
- Suga, H., et al. Systolic pressure-volume area (PVA) as the energy of contraction in Starling’s law of the heart. Heart Vessels. 6, 65-70 (1991).
- Murakami, T., Hess, O., Gage, J., Grimm, J., Krayenbuehl, H. Diastolic filling dynamics in patients with aortic stenosis. Circulation. 73, 1162-1174 (1986).
- Baan, J., et al. Continuous measurement of left ventricular volume in animals and humans by conductance catheter. Circulation. 70, 812-823 (1984).
- Falsetti, H. L., Verani, M. S., Chen, C. J., Cramer, J. A. Regional pressure differences in the left ventricle. Catheter Cardiovasc. Diag. 6, 123-134 (1980).
- Kass, D. A. Assessment of diastolic dysfunction. Invasive modalities. Cardiol. Clin. 18 (3), 571-586 (2000).
- Suga, H. Cardiac energetics: from EMAX to pressure-volume area. Clin. Exp. Pharmacol. Physiol. 30, 580-585 (2003).
- Gottdiener, J. S., et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. JASE. 17, 1086-1119 (2004).
- Kovács, S. J. Jr, Barzilai, B., Pérez, J. E. Evaluation of diastolic function with Doppler echocardiography: the PDF formalism. Am. J. Physiol. Heart Circ. Physiol. 252, H178-H187 (1987).
- Hall, A. F., Aronovitz, J. A., Nudelman, S. P., Kovács, S. J. Automated method for characterization of diastolic transmitral Doppler velocity contours: Late atrial filling. Ultrasound Med. Biol. 20, 859-869 (1994).
- Hall, A. F., Kovács, S. J. Automated method for characterization of diastolic transmitral Doppler velocity contours: Early rapid filling. Ultrasound Med. Biol. 20, 107-116 (1994).
- Riordan, M. M., Kovács, S. J. Quantitation of Mitral Annular Oscillations and Longitudinal 'Ringing' of the Left Ventricle: A New Window into Longitudinal Diastolic Function. J. Appl. Physiol. 100, 112-119 (2006).
- Kovács, S. J., Meisner, J. S., Yellin, E. L. Modeling of diastole. Cardiol. Clin. 18, 459-487 (2000).
- Riordan, M. M., Chung, C. S., Kovács, S. J. Diabetes and Diastolic Function: Stiffness and Relaxation from Transmitral Flow. Ultrasound Med. Biol. 31, 1589-1596 (2005).
- Bauman, L., Chung, C. S., Karamanoglu, M., Kovács, S. J. The peak atrioventricular pressure gradient to transmitral flow relation: kinematic model prediction with in vivo validation. J. Am. Soc. Echocardiogr. 17 (8), 839-844 (2004).
- Kovács, S. J. Jr, Rosado, J., Manson-McGuire, A. L., Hall, A. F. Can Transmitral Doppler E-waves Differentiate Hypertensive Hearts From Normal? Hypertension. 30, 788-795 (1997).
- Riordan, M. M., et al. The Effects of Caloric Restriction- and Exercise-Induced Weight Loss on Left Ventricular Diastolic Function. Am. J. Physiol. Heart Circ. Physiol. 294, H1174-H1182 (2008).
- Meyer, T. E., Kovács, S. J., Ehsani, A. A., Klein, S., Holloszy, J. O., Fontana, L. Long-term Caloric Restriction Slows Cardiac Aging in Humans. J. Am. Coll. Cardiol. 47, 398-402 (2006).
- Riordan, M. M., Kovács, S. J. Absence of diastolic mitral annular oscillations is a marker for relaxation- related diastolic dysfunction. Am. J. Physiol. Heart Circ. Physiol. 292, H2952-H2958 (2007).
- Mossahebi, S., Kovács, S. J. Kinematic Modeling-based Left Ventricular Diastatic (Passive) Chamber Stiffness Determination with In-Vivo Validation. Annals BME. 40 (5), 987-995 (2012).
- Zhang, W., Chung, C. S., Riordan, M. M., Wu, Y., Shmuylovich, L., Kovács, S. J. The Kinematic Filling Efficiency Index of the Left Ventricle: Contrasting Normal vs. Diabetic Physiology. Ultrasound Med. Biol. 33, 842-850 (2007).
- Zhang, W., Kovács, S. J. The Age Dependence of Left Ventricular Filling Efficiency. Ultrasound Med. Biol. 35, 1076-1085 (2009).
- Courtois, M., Kovács, S. J., Ludbrook, P. A. Transmitral pressure-flow velocity relation. Importance of regional pressure gradients in the left ventricle during diastole. Circulation. 78, 661-671 (1988).
- Zhang, W., Shmuylovich, L., Kovács, S. J. The E-wave delayed relaxation pattern to LV pressure contour relation: model-based prediction with in vivo validation. Ultrasound Med. Biol. 36 (3), 497-511 (2010).
- Shmuylovich, L., Kovács, S. J. A load-independent index of diastolic filling: model-based derivation with in-vivo validation in control and diastolic dysfunction subjects. J. Appl. Physiol. 101, 92-101 (2006).
- Kreyszig, E. Advanced Engineering Mathematics. , 10th, John Wiley and Sons. Hoboken NJ. (2011).
- Press, W. H., Teukolsky, S. A., Vetterling, W. T., Flannery, B. P. Numerical recipes 3rd Edition: The Art of Scientific Computing. , Cambridge University Press. New York, NY. (2007).
- Claessens, T., et al. The Parametrized Diastolic Filling Formalism: Application in the Asklepios Population. Am. Soc. Mech. Eng. Summer Bioengineering Conference Proceedings. Farmington PA, , (2011).
- Chung, C. S., Kovács, S. J. Consequences of Increasing Heart Rate on Deceleration Time, Velocity Time Integral, and E/A. Am. J. Cardiol. 97, 130-136 (2006).
Access restricted. Please log in or start a trial to view this content.
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone