Method Article
Transcranial Direct Current Stimulation (tDCS) for Memory Enhancement
In This Article
Summary
A protocol for memory enhancement by using transcranial direct current stimulation (tDCS) targeting dorsolateral prefrontal and posterior parietal cortices, as core cortical nodes within hippocampo-cortical network, is presented. The protocol has been well evaluated in healthy-participant studies and is applicable to aging and dementia research as well.
Abstract
Memory enhancement is one of the great challenges in cognitive neuroscience and neurorehabilitation. Among various techniques used for memory enhancement, transcranial direct current stimulation (tDCS) is emerging as an especially promising tool for improvement of memory functions in a non-invasive manner. Here, we present a tDCS protocol that can be applied for memory enhancement in healthy-participant studies as well as in aging and dementia research. The protocol uses weak constant anodal current to stimulate cortical targets within cortico-hippocampal functional network engaged in memory processes. The target electrode is placed either on the posterior parietal cortex (PPC) or the dorsolateral prefrontal cortex (DLPFC), while the return electrode is placed extracranially (i.e., on the contralateral cheek). In addition, we outline a more advanced method of oscillatory tDCS, mimicking a natural brain rhythm to promote hippocampus-dependent memory functions, which can be applied in a personalized and non-personalized manner. We present illustrative results of associative and working memory improvement following single tDCS sessions (20 minutes) in which the described electrode montages were used with current intensities between 1.5 mA and 1.8 mA. Finally, we discuss crucial steps in the protocol and methodological decisions that must be made when designing a tDCS study on memory.
Introduction
Memory plays a vital role in everyday functioning as it enables one to remember information about people and places, recall past events, learn new facts and skills, as well as to make judgments and decisions. Here we focus on two types of memory - working memory (WM) and associative memory (AM). WM provide us with the ability to temporarily maintain and store information for ongoing cognitive processing1, while AM enables us to remember multiple pieces of experience or information bound together. Therefore, these two types of memory underline almost all daily activities. Unfortunately, memory is one of the most vulnerable functions as it declines with normal ageing as well as due to various pathological states and conditions. Both WM and AM decline is prominent in mild cognitive impairment2,3 and dementia4,5 as well as in normal ageing6,7. Since memory deficits are associated with a high disease burden level8,9 and significantly affect quality of life10,11,12,13, there is a growing need for novel approaches to prevention and treatment of memory decline.
Transcranial direct current stimulation (tDCS) is a promising tool for tackling memory decline14,15,16 and gaining better understanding of brain functions in general17. tDCS is a non-invasive brain stimulation technique that uses weak electric currents (usually between 1 mA and 2 mA) to modulate brain activity by affecting neuronal membrane excitability. The effects of tDCS are polarity-dependent, such that anodal stimulation increases while cathodal decreases neuronal excitability. Namely, anodal tDCS increases the likelihood for action potentials to fire through depolarization of neuronal membranes, thus facilitating spontaneous brain activity under the anode18. Moreover, it is shown that the effect of increased activation does not remain localized but tends to spread to other functionally connected areas of the central nervous system. Anodal tDCS is thus expected to promote cognitive functions that rely on targeted brain regions and functionally interconnected brain areas, while cathodal tDCS is expected to have the opposite effect.
The tDCS has several advantages over other brain stimulation techniques: (1) tDCS is safe, i.e., does not pose health risks and does not produce any negative short or long term structural or functional changes19; (2) tDCS is characterized by highest tolerability among brain stimulation techniques as it causes minimal discomfort to participants in a form of a mild tingling and itching sensations under the stimulating electrodes20; (3) tDCS is cost-effective - the price of tDCS devices and application are ten to hundred times lower than other treatment options, which makes it attractive for patients and healthcare system; (4) tDCS is easy to use, and therefore has a high potential to be applied even in home-based settings, which can lead to higher compliance of patients and reduced cost for medical staff and facilities.
The main challenges for using tDCS for memory enhancement are finding the optimal electrode montage and stimulation protocol that will produce reliable effects on memory. Here we use the term electrode montage to refer to the configuration and the positions of the electrodes (i.e., the placement of the target and reference (return) electrode). Due to the nature of the electrical fields, the reference (return) electrode is not neutral - it has the polarity opposite to the target electrode - and thus can also exercise biological (neuromodulatory) effects on the underlying neural tissue. Therefore, careful choice of the reference electrode is essential for avoiding unwanted additional effects of the stimulation.
When using the term stimulation protocol, we refer to the tDCS parameters such as the duration and the intensity of the current being applied as well as the way current intensity changes over time (i.e., whether the intensity is constant throughout the stimulation or changes following a sinusoidal waveform with certain amplitude and frequency). Different stimulation protocols can be applied using the same electrode montage, and the same protocol can be used across different montages.
To optimize the electrode montage, we look at the function-relevant brain areas and how the electric fields induced by various positions of the electrodes would affect those brain areas and consequentially cognitive functions. Several different cortical and subcortical structures play a significant role in memory functions - including areas of the frontal, temporal, and parietal cortex. Namely, WM is supported by a widespread neural network that includes dorsolateral (DLPFC) and ventral lateral prefrontal cortex (VLPFC), premotor and supplementary motor cortices, as well as posterior parietal cortex (PPC)21. For AM and episodic memory in general, structures within medial temporal lobe are essential22. However, associative areas of the parietal, frontal, and temporal cortices, with their convergent pathways to the hippocampus also play a significant role. Due to its anatomical position, the hippocampus cannot be directly stimulated using tDCS, and thus the enhancement of hippocampus-dependent memory functions is done using the cortical targets with high functional connectivity to hippocampus such as posterior parietal cortex. For these reasons, DLPFC and PPC are most frequently used as stimulation targets to enhance memory. Positioning of the electrodes can be further refined based on current flow modeling23 and validated in studies that combine tDCS with neuroimaging techniques24.
The most usual stimulation protocol is a constant anodal current of 1-2 mA that lasts between 10-30 minutes. The assumed mechanism behind this protocol is that the electrode with a positive charge will increase the excitability of the underlying cortical tissue which will than result in enhanced subsequent memory performance. Unlike the constant anodal tDCS, where current intensity stays the same during the whole stimulation period, in the oscillatory tDCS protocol the intensity of the current fluctuates at the given frequency around a set value. Therefore, this type of protocol modulates not only excitability but also entrains neural oscillations of the relevant brain areas. It is important to note that for both constant and oscillatory tDCS the electrodes retain the same current polarity for the whole duration of the stimulation.
Here we present tDCS montages that target nodes within fronto-parieto-hippocampal network to promote memory - both WM and AM: specifically, two electrode montages with the target electrode over either left/right DLPFC or left/right PPC. In addition to constant anodal tDCS protocol we outline a theta oscillatory tDCS protocol.
Study design
Before providing a detailed guide on how to use tDCS for memory enhancement, we will outline a few essential properties of the experimental design that are important to consider when planning a tDCS study on memory.
Sham control
To assess the effects of tDCS on memory, the study needs to be sham controlled. This implies that in one of the experimental conditions the protocol resembles a real stimulation session, but no treatment is given. This fake or sham session serves as a reference point to compare performance following real tDCS and make inferences about its effectiveness. Commonly, in the sham protocol the current is applied only for a brief period - usually up to 60 seconds at the beginning and at the end of the sham stimulation as a ramp-up followed by immediate ramp-down (i.e., fade-in/fade-out, up to 30 seconds each) fashion. This way it is ensured that the duration of the stimulation is insufficient to produce any behavioral or physiological effects. Since local skin/scalp sensations are usually most pronounced at the beginning and at the end of stimulation (due to changes in the current intensity), the sensations induced in all protocols are comparable and difficult to distinguish25. This way, the participant is blinded on whether the stimulation is real or not, which is especially important in within-subject designs.
In addition to sham-control, to assess the specificity of the effects of oscillatory protocols, it is advisable to have an active control condition, too. For instance, the active control for oscillatory protocol can be constant anodal stimulation of the same intensity26,27, or oscillatory stimulation in different frequency e.g. theta vs gamma28.
Within- or between-subjects design.
In within-subjects design each participant undergoes both real and sham tDCS, while in between-subjects design one group of participants receives real, and the other group receives sham tDCS. The main advantage of within-subject design is better control of subject-specific confounds. That is, individual differences in anatomy and cognitive abilities are best controlled for when each participant is compared to their self. However, since within-subject design needs to be applied in cross-over fashion (i.e., half of the participants receive real tDCS in the first session and sham in the second session, while the other half of participants receive sham first and real tDCS second) this design may not be optimal for clinical and training studies as well as studies involving several tDCS sessions over consecutive days, because crossover design may result in unequal baselines between crossover arms. Therefore, within-subject design is suited the best when assessing either behavioral or physiological effects of a single tDCS session, and when unequal baselines are not considered an issue for the research hypothesis. In within-subject design assessing the effects of single tDCS session, it is a good practice to keep 7 days between real and sham tDCS session to avoid carryover effects (however some studies suggest even shorter wash-out periods do not significantly affect the outcomes29,30) and to use parallel forms of memory tasks in counterbalanced order to minimize training and between-session learning effects.
When between-subjects design is used, the control group should be carefully matched for baseline performance, as well as other relevant characteristics known to be of relevance for tDCS effectiveness. Random group assignment may not be the best approach in small sample sizes (e.g., <100) as it may lead to suboptimal matching. In either case, baseline performance should be accounted for in statistical analysis.
Sample size.
One of frequently asked questions is "how many participants does one need to detect tDCS effects". The answer to this question depends on several aspects of the study including experimental design, expected effects sizes, type of statistical analysis, etc. The sample sizes in the brain stimulation experiments are often too small, and it is estimated that studies in this field miss around 50% of true positive results because they are underpowered31. Power analysis enables determining adequate sample size for each specific experiment based on the study design and expected effect size for planned statistical analysis. The power analysis can be performed in R environment or using free specialized software such as G*Power32, and it should always be performed a priori (i.e., before the experiment). The power should be set at >.80 (ideally .95) and expected effect size on memory tasks following a single tDCS session is usually between .15-.20 (η2) i.e., Cohen f 0.42-0.50. Therefore, one typically needs to enroll 20-30 participants in total for within-subject experiment and 30-40 participants per group for between-subject study, to achieve satisfactory power and thus diminish type II error. However, the sample size depends on the number of other factors including the planned analysis, and sensitivity of the behavior measures that are used. Therefore ideally, one would run an initial experiment to understand the effect sizes for the specific design and use those data as an input for power analysis. However, it is important to note that running a pilot experiment on just a few participants will lead to faulty and unreliable estimates of the effect sizes. Therefore, if resources are limited it is better to rely on the previous studies with comparable outcomes, and take slightly more conservative approach i.e., by estimating for somewhat smaller effect sizes than reported in the literature.
Outcome measures
To assess the effectiveness of tDCS on memory one needs to select adequate behavioral tasks. In fact, the choice of the memory task is one of the crucial aspects of the study design, because the ability to detect the tDCS effect directly depends on the sensitivity of the task. The challenge here is that most standardized memory assessment tools or classical neuropsychological tasks may not be sensitive enough to detect tDCS effects in specific populations. Furthermore, most of the standardized tasks are not available in two or more parallel forms and therefore cannot be used in within-subjects designs. For that reason, most of the tDCS memory studies use custom-build tasks. When designing or selecting outcome measure one should ensure that the task is: (1) focal/selective measure of the memory function of interest; (2) sensitive (i.e., that the scale is fine enough to detect even small changes); (3) challenging for the participants (i.e., that the task difficulty is sufficient and thus to avoid celling effects); (4) reliable (i.e., that the measurement error is minimized as much as possible). Therefore, one should use empirically validated strictly parallel forms of memory tasks, which have a sufficient number of trials - both to ensure sensitivity of the measure as well as to maximize its reliability. Ideally, the tasks should be pre-tested on a group sampled from the same population as the experiment participants to ensure that maximum performance is not achievable, and that the task-forms have equal indices of difficulty. Finally, it is best to use computerized tasks whenever possible as they allow for controlled duration and precise timing. This way researchers can ensure that all participants undergo memory assessment at the same time in respect to the timing of stimulation (either during or following tDCS). The duration of each task or task block should not be longer than 10 minutes, to avoid fatigue and fluctuation in attention levels; the cognitive assessment should not be longer than 90 minutes in total (including tasks both during and after tDCS).
Protocol
This procedure has been approved by the Institutional Ethics Committee and is in line with the Declaration of Helsinki and guidelines for human research.
1. Materials
NOTE: For each tDCS session prepare the following materials (Figure 1).
- Obtain a tDCS device - use only a battery driven tDCS device or a mains-connected optically isolated tDCS device. The device should function as a constant current stimulator with a maximum output limited preferably to a few milliampere range. The device must have regulatory approval for human use.
- Obtain rubber electrodes - use either 5 cm x 5 cm square-shaped or 25 cm2 round-shaped electrodes. These electrodes will have the current densities between 0.06 mA/cm2 and 0.08 mA/cm2 for currents of 1.5 mA-2 mA, respectively.
- Prepare sponge pockets that fit the rubber electrodes. If the sponge pocket is too large it will increase the contact surface to the skin.
- Prepare saline solution (standard 0.9% NaCl).
- Prepare alcohol (70%).
- Obtain an adjustable silicone cap - head straps can be used as well, however EEG silicone caps can be better adjusted to the size and the shape of participants' head and are therefore more comfortable for electrode placement.
- Obtain measuring tape (flexible; plastic or ribbon).
- Obtain a skin marker - skin marker pencils or various makeup products (e.g., eye pencil or eyeshadow crayon), the later can be even more convenient as they are dermatologically tested and easily removable.
- Obtain cotton pads.
- Obtain comb and single-use mini silicon hair bands.
- Obtain a syringe or plastic pipette.
- Prepare a protocol sheet - fill-in form for basic information about the session i.e., participants ID, study ID, date, times, notes, etc (see Appendix for an example).
- Prepare a table with pre-calculated head measures to help with electrodes' placement.
NOTE: To speed-up the process and to reduce the possibility for errors, it is advisable to have this table ready in advance. The measurement is based on 10-20 EEG electrode placement system; the values used for calculations are nasion-inion/left-right-preauricular distances (see below). The table gives 20% values for a range of distance values. We have found it as the most convenient to have the table embedded into the protocol sheet (Appendix). - Prepare questionnaires. For each session, collect data on sensations and side effects before and after tDCS; sensations and the level of (un)pleasantness during tDCS; mood and general subjective state i.e., freshness/tiredness.
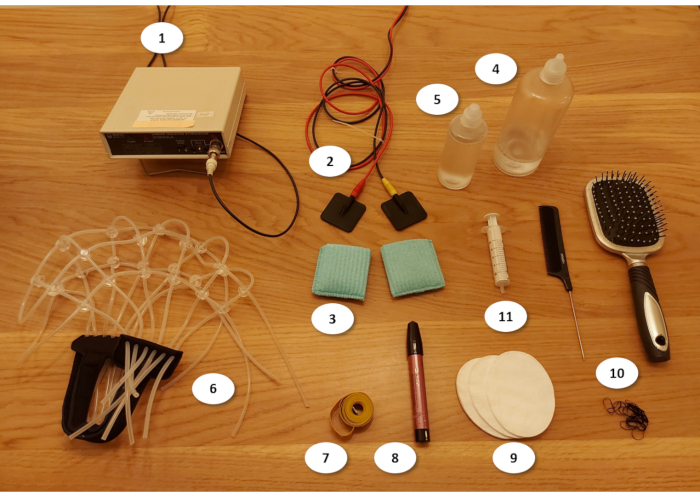
Figure 1: Materials for tDCS experiment (see text for details). 1) tDCS device; 2) electrodes; 3) sponges; 4) saline solution; 5) alcohol; 6) silicone cap; 7) measuring tape; 8) skin pencil; 9) cotton pads; 10) combs and silicon hairbands; 11) syringe Please click here to view a larger version of this figure.
2. Programing stimulation protocols
NOTE: Exact steps in programming tDCS protocol differ across tDCS systems/devices. However, all tDCS devices provide basic features - the ability to produce constant current with desired stimulation intensity, the ability to gradually ramp up and down, and a method to set the duration of stimulation. The more advanced protocols such as theta-oscillatory tDCS require devices/systems that allow for custom-built stimulation protocols.
- Constant anodal tDCS
- Define the standard constant anodal tDCS protocol (Figure 2A) as: (1) fade-in period of 30 seconds, when current intensity is gradually ramped up from 0 mA to the target intensity (we typically use 1.5 mA, but other intensities can be used as well, providing they stay within safety limits); (2) stimulation period during which the constant current of the target intensity (e.g., 1.5 mA) is delivered; and (3) fade-out period of 30 seconds when current intensity is gradually decreased to 0 mA.
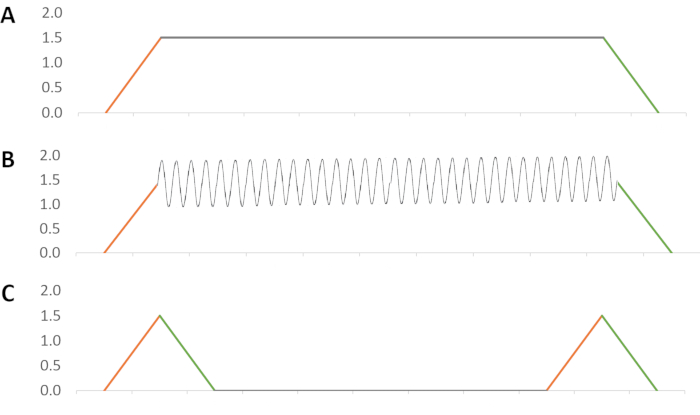
Figure 2: tDCS protocols: (A) Constant anodal tDCS; (B) Theta oscillatory tDCS; (3) Sham tDCS. Fade in period is marked orange; fade out period is marked green. Please click here to view a larger version of this figure.
- Theta oscillatory tDCS
- Theta-oscillatory tDCS delivers current of varying intensity but does not switch polarities (Figure 2B). Therefore, define the waveform in which the current is delivered as following: (1) fade-in period of 30 seconds, when current intensity is gradually ramped up from 0 mA to the target intensity (e.g., 1.5 mA); (2) the stimulation period of 19 minutes in which the current oscillates around the target intensity within a pre-defined amplitude range (we use oscillations of ± 0.5 mA of the target intensity) in a selected frequency (we typically use 5 Hz frequency as representative for theta rhythm); and (3) fade-out period of 30 seconds to bring the current intensity to 0 mA.
NOTE: This protocol can be generated by any experimental control software (e.g., CED Signal) and delivered through an intelligent interface (e.g., CED 1401 range of devices) that is compatible with tDCS device which is to be used. Some more advanced dedicated transcranial electric stimulation (tES) systems besides tDCS can deliver alternating current (tACS) and random noise stimulation (tRNS) too. They can also be used to generate the oscillatory tDCS protocol. For example, in StarStim the theta-oscillatory tDCS protocol are defined as a linear combination of tDCS (1.5 mA) and tACS (±0.5 mA, 5 Hz). This type of protocol can be personalized in a sense that not all participants receive oscillatory stimulation in the same frequency (i.e., 5 Hz), but that the frequency is adjusted to the dominant frequency within theta band for each person (e.g., Person 1: 5 Hz, Person 2: 6 Hz, Person 3: 4.5 Hz, etc.).
- Theta-oscillatory tDCS delivers current of varying intensity but does not switch polarities (Figure 2B). Therefore, define the waveform in which the current is delivered as following: (1) fade-in period of 30 seconds, when current intensity is gradually ramped up from 0 mA to the target intensity (e.g., 1.5 mA); (2) the stimulation period of 19 minutes in which the current oscillates around the target intensity within a pre-defined amplitude range (we use oscillations of ± 0.5 mA of the target intensity) in a selected frequency (we typically use 5 Hz frequency as representative for theta rhythm); and (3) fade-out period of 30 seconds to bring the current intensity to 0 mA.
- Sham tDCS
- Use a sham protocol with the same duration as constant/oscillatory tDCS (Figure 2C). Namely, define it as: (1) first fade in/out period in which the current is gradually ramped up to target intensity (e.g., 1.5 mA) and gradually ramped down to 0 mA during the first 60 seconds (2) 18 minutes of 0 mA, and (3) the second fade in/out period which again lasts 60 seconds.
NOTE: An alternative approach would be to use very low current intensity over the entire stimulation period (20 min). This type of sham protocol is programmed the same as the anodal stimulation (only the current intensity is set to (0.1 mA) and is designed to produce cutaneous sensations but the intensity is too week to produce any physiological effects33.
- Use a sham protocol with the same duration as constant/oscillatory tDCS (Figure 2C). Namely, define it as: (1) first fade in/out period in which the current is gradually ramped up to target intensity (e.g., 1.5 mA) and gradually ramped down to 0 mA during the first 60 seconds (2) 18 minutes of 0 mA, and (3) the second fade in/out period which again lasts 60 seconds.
3. Electrode placement (Figure 3)
- DLPFC electrode montage: For stimulation of the DLPFC, place the target (anodal) electrode on either F3 (left) or F4 (right) of the international 10-20 EEG system. Place the return electrode (cathodal) on the contralateral cheek - i.e., right cheek for F3 anode and left cheek for F4 anode.
- PPC electrode montage: For stimulation over PPC, place the target (anodal) electrode on either P3 (left) or P4 (right) of the international 10-20 EEG system. Place the return electrode (cathodal) on the contralateral cheek same as in DLPFC montage.
- The target electrode placement
- To locate F3 on participants' head
- Use the measuring tape to measure the distance between nasion (the deepest point of the nasal bridge) and inion (the most pronounced point of the external occipital protuberance) going over the top of the head. Mark the halfway distance with the skin marker with a thin line.
- Measure the distance between the ears (use preauricular points as references) going over the top of the head and mark the halfway distance with a thin line.
- Find the vertex or midline central position, referred as Cz, at the intersections of the two midlines. Mark it clearly with the skin marker.
- Measure again the nasion-inion distance, but this time going over Cz, and note the distance as measure A. Measure again the distance between the ears, this time going over Cz, and note the distance as measure B.
- Calculate 20% of distance A, and 20% of distance B (or see Protocol sheet for pre-calculated values).
- Move 20% of distance A forward from Cz along the nasion-inion line to reach Fz (midline frontal) and mark the spot.
- Move 20% of distance B leftward from Cz along the inter-auricular line to reach C3 (left central) and mark the spot.
- Move 20% forward form C3 (in parallel with the nasion-inion line), and 20% leftward form Fz (in parallel with the inter-auricular line), to reach F3 at the intersection. Mark F3 with the skin-marker and place the center of the electrode at the spot.
- To locate F4, follow the same procedure only on the right side of the head.
- To locate P3 on participants' head
- Follow the steps 3.3.1.1-3.3.1.5 as outlined above (find Cz, note distance A and B, calculate 20%).
- Move 20% of distance A backward from Cz along the nasion-inion to reach Pz (midline parietal) and mark the spot.
- Move 20% of distance B leftward from Cz along the inter-auricular line to reach C3 and mark the spot.
- Move 20% backward from C3 (in parallel with the nasion-inion line), and 20% leftward from Pz (in parallel with the inter-auricular line), to reach P3 at their intersection. Mark P3 with the skin-marker and place the center of the electrode at the spot.
- To locate P4, follow the same procedure only on the right side of the head.
- To locate F3 on participants' head
- Return electrode placement
- After securing the target electrode with the adjustable silicon cap (see step-by step procedure), insert the return electrode below the chin band to secure the contact of the electrode with the contralateral cheek.
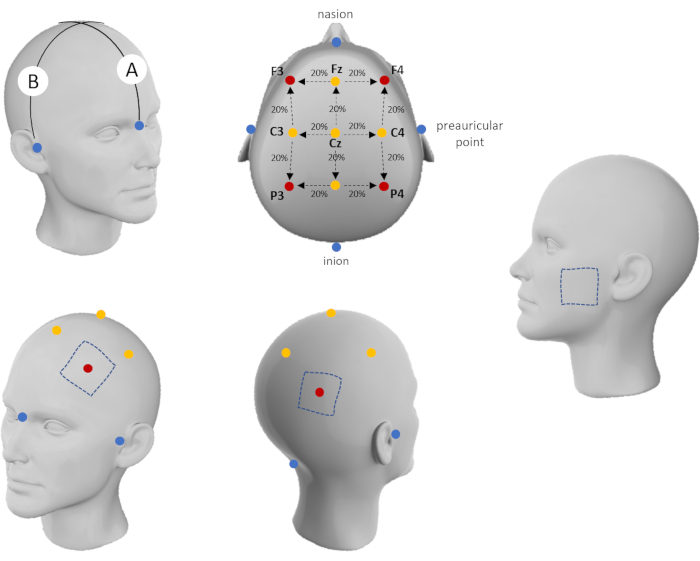
Figure 3: Electrode placement scheme. Please click here to view a larger version of this figure.
4. Step-by-step procedure
- Before the tDCS session
- Check if each participant satisfies the inclusion criteria as defined in ethical approval for the study (see Appendix for the most common inclusion/exclusion criteria).
- Ask the participant to fill in the Participant information sheet (including all the relevant information such as age, gender, nicotine/alcohol consumption, etc.34).
- Follow the institutional review board ethical guidelines, and ask participant to sign informed consent. Use this opportunity to explain the basic aspects of the procedure they will undergo and answer any questions the participants may have.
- Depending on the study design, perform baseline cognitive assessment (memory and/or other cognitive functions).
- tDCS set-up and stimulation
- Seat the participant comfortably in a chair.
- Ask participant to fill out pre-tDCS sensations checklist and to report on overall state (i.e., current mood; freshness/tiredness - these can be assessed either as a single Likert-type item or using standardized questionnaires such as Brief Mood Introspection Scale35).
- Take head measures using a measuring tape.
- For locating the DLPFC or PPC follow the procedure described above (electrode placement). Write down the measures in the Protocol sheet for each participant. These can be used to check against when taking measurements in subsequent sessions.
- To increase conductance, move away participant's hair from stimulation site (use comb and hair bands for participants with long hair).
- Inspect for any signs of skin damage at the place of stimulation. Avoid positioning electrodes over damaged skin.
- Clean the surface of the skin where electrodes will be placed using alcohol-soaked cotton pads to remove grease, dirt, etc. and let it dry (use a makeup removal product if the participant has heavy makeup on the cheek).
- Put the silicon cap on the participant's head and secure it with the chinstrap. Do not make the cap tight (this will be done later).
- Soak the sponge pockets with saline solution and put the electrodes inside them. The sponges should be moist but not dripping; usually 10-15 mL of saline solution per sponge is enough. If the sponges are too dry this will cause high resistance and result in poor conductivity, even losing the circuit connection.
NOTE: Most of the tDCS devices have the resistance indicators; however, the sponges should be occasionally inspected for moisture. On the other hand, if the sponges are excessively wet it can cause the current to shift across the head during stimulation. It is recommend having sponges medium wet and use a syringe to add more saline solution during the experiment if the sponges become too dry. - Put the sponge electrode under the silicon straps and position the center of the target electrode on the marked head-location. Set the return electrode on the contralateral cheek. Use the silicon straps to adjust the cap to the participant's head-size and shape. The cap should be tight so the electrodes cannot move, but still comfortable for the participant.
- Turn on the stimulator, select and run predefined tDCS protocol (active anodal stimulation or sham).
- Ask the participant to relax and let them report how they feel during the first few minutes of stimulation (1-3 minutes). Explain that the sensations will slowly fade away as they get used to it or when they start focusing their attention on some other activity.
- To avoid unstructured activities that can interfere with the stimulation effects, use light cognitive engagement during tDCS. For example, participants can perform practice trials of cognitive tasks or engage in easy memory games during stimulation (starting after 3-5 minutes of stimulation). This type of cognitive engagement during stimulation has the potential to promote tDCS effects and will help participants to keep the mind off the tDCS-induced skin sensations.
- Ask the participant to report how they feel multiple times during stimulation (e.g., to report the level of unpleasantness on a 10-point scale every 5 minutes of stimulation, 1 - completely absent, 10 - very intensive). Higher levels of unpleasantness (>6) could be expected during fade-in fade-out periods in some participants. If the level of unpleasantness remains high after 5 minutes abort the stimulation.
- After the pre-defined protocol run has elapsed, turn off the stimulator.
- Remove the sponge electrodes first, and then remove the silicon cap.
- Ask the participant to fill out post-tDCS sensations checklist and to report for any side effects not already listed.
- Clean the skin on the places where it was marked and inspect the skin for any changes. If there is a skin reaction (e.g., local vasodilation i.e., skin redness on the cheek), monitor as it fades away as it is usually a transient reaction in participants with sensitive skin, and should disappear within 10-15 minutes.
- Memory assessment
- To standardize the assessment across participants, use computerized assessment tools i.e., memory tasks with automatic scoring. Several WM tasks (e.g., verbal and spatial 3-back task) and AM tasks (verbal paired learning; face-word cued recall, object location, etc.) can be found here: https://osf.io/f28ak/?view_only=f8d5e8dd71d24127b3668ac3d8769408
- To evaluate the specificity of tDCS effects on memory it is advisable to include control task(s) i.e., tasks tapping other cognitive or motor function.
- Ending the experimental session/study
- After the (last) experimental session in the study ask participant to try to guess the sessions in which they have received real and sham stimulation. Note all responses and see whether obtained proportions are higher than chance probability. If not, the blinding was successful. If participants were able to differentiate real from sham stimulation analyze the data for those that guessed correctly and those that did not to check if the unsuccessful blinding affected the tDCS effects.
- In line with ethical guidelines, debrief the participants in detail after their involvement is completed.
- After the experimental session
- Wash the sponges with running water and soap so that the saline solution is fully washed away. Let the sponges to dry completely before putting them away.
- Use warm water and alcohol to clean all reusable materials including comb, silicone cap and measuring tape.
- Make notes on all unusual, unexpected, or unplanned events that might have happened during the session - including any equipment malfunctions, relevant comments made by the participant, interruptions, etc.
Results
The described protocol has been successfully used to enhance memory performance in several studies in our laboratory. However, similar protocols have been used in other research laboratories as well (e.g., see36,37).
When it comes to working memory, our results have shown that 20-minutes of right frontal tDCS (F4 location; constant current of 1.8 mA) enhanced verbal WM, while the same stimulation protocol applied over left parietal cortex (P3 location) resulted in better spatial WM performance. In contrast, no significant effects were found when the same stimulation protocol was applied over the left frontal (F3) and right parietal (P4) cortices. Figure 4 shows the representative results of modeling of the electric field generated by tDCS as well as the performance measures following active and sham tDCS based on the data reported in Živanović et al., 202138.
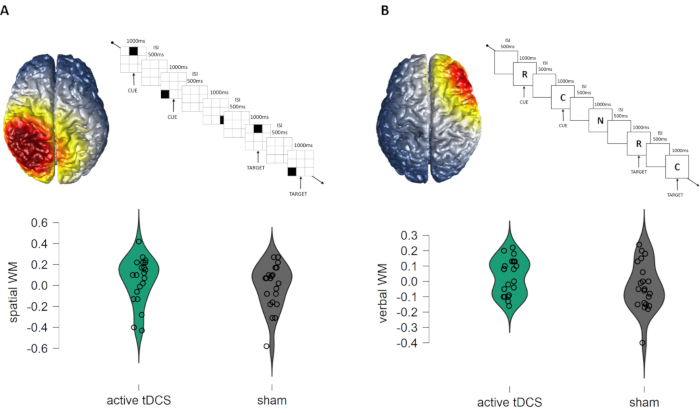
Figure 4: (A) Effects of constant anodal tDCS of left PPC (P3-contralateral cheek montage) on spatial working memory performance (spatial 3-back task); (B) Effects of constant anodal tDCS of right DLPFC (F4-contralateral cheek montage) on verbal WM performance (verbal 3-back task). The figure shows simulation of electric fields induced by tDCS, outline of the task trials, and the within-subjects performance across active and sham condition (the values are centered to the order of the session to account for counterbalancing i.e., positive values indicate above-average performance, while negative values indicate below average performance at session). The simulation of local electric fields generated by the electrode set up is performed using COMETS2 MATLAB toolbox 41. Please click here to view a larger version of this figure.
The effects of parietal tDCS on associative memory have been consistent and robust. That is, in the series of within-subject experiments we have shown that 20 minutes of tDCS over left PPC (P3 location; constant current of 1.5 mA) improves memory for face-word associations27,39,40. Figure 5 shows representative task and results. In addition, comparable effects were observed on AM task assessing the object-location associations when right PPC (P4 location) is stimulated using the same constant tDCS protocol40.
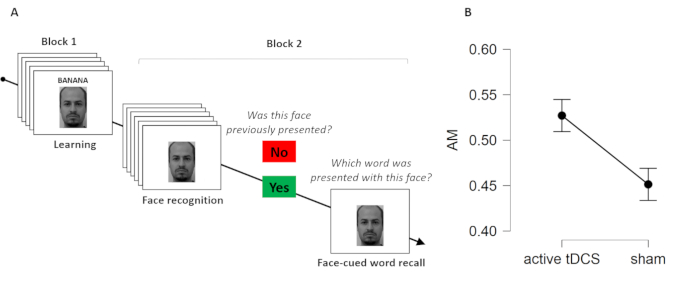
Figure 5: Effects of constant anodal tDCS of left PPC (P3-contralateral cheek montage) on associative memory performance (A) Face-word pairs task; (B) Effects of constant anodal tDCS of left PPC (P3-contralateral cheek montage) on associative memory performance (proportion of correctly recalled words on cue). Please click here to view a larger version of this figure.
The more advanced protocols such as theta-oscillatory tDCS have been less extensively studied, however the study by Lang and colleagues26 as well as recent study conducted in our laboratory27 showed improvement in face-word AM following theta-oscillatory tDCS protocol in comparison to sham. The animated figure shows simulation of the electric field induced by theta oscillatory tDCS over left PPC.
Discussion
The outcome of the tDCS study on memory depends on number of factors, and some of which e.g., homogeneity/heterogeneity of the sample, sufficient statistical power, the difficulty of the memory tasks and motivation of the participants have been previously discussed (see Berryhill, 2014). Several excellent papers on tDCS method, as well as more general tutorials on the application of tDCS to study cognitive functions are available and can be well applied to the memory research too (see17,43,44,45,46,47). Here we will focus on the aspects of the protocol which, based on our experience, are relevant but often overlooked or not discussed in sufficient detail elsewhere.
Placement of the return electrode. It is important to keep in mind that the return electrode is not passive but negative-polarity terminal (i.e., cathode). Therefore, it can induce physiological effects that are opposite to the target electrode. Furthermore, the current flow, depends on the positioning of the return as much as it depends on the target electrode. Moreover, since the current flows along the path of the least resistance, if the anode and cathode are located too close to each other, the current may flow only over the skin surface and/or through the cerebrospinal fluid between the electrodes, thus leaving the cortical tissue unaffected. For these reasons, the careful choice of the return electrode is as relevant as the position of the target electrode. There is meta-analytic evidence to suggest that extracranial cathodes are more likely to produce significant effects48. Positioning of the return electrode on contralateral cheek for memory enhancement was based on current flow modeling and selected to avoid potential confounding effects of generating negative polarity over function-irrelevant brain areas. The positioning of return electrode on the contralateral cheek has successfully been used in previous WM studies (see36,37,38,49, as well as in AM studies27,39,40), and has been highlighted as a good choice for tDCS montages aiming to modulate other cognitive functions as well45.
Blinding. In single blind experiments, to ensure blinding of the participant, the position of the stimulator and/or monitoring display should be out of participant's sight. This is especially important when using stimulators that have lights indicating when the unit is on and/or delivering current. For double-blind designs (when both participant and experimenter are unaware of the protocol which is administered), one should use the double-blind option, or similar option that is available for a given device. If such option is not available, the good practice is to have two-experimenter procedure. That is, one experimenter comes in only to run the stimulation protocol, while the other experimenter who runs the participant through the experiment, including the subsequent memory task and analyzes the data, leaves the room just before and during the stimulation. By methodological standards, double-blind experiments are preferred to the single-blind designs because they reduce the bias or the "experimenter" effects. This is highly relevant when conducting clinical trials and/or using the interview-based assessments of cognitive functions. However, blinding of the experimenter is less of an issue when participants are highly motivated to maximize their performance (which is mostly the case in memory assessment or cognitive enhancement in general), and when the task is administrated as well as scored automatically (i.e., when experimenter has little to no intervention in the assessment phase).
Activity during tDCS. Authors of tDCS papers rarely report on what were the participants doing during stimulation. When the activity is not reported it is usually implied that the participants were instructed to sit comfortably and relax. However, the absence of structured activity represents source of the uncontrollable "noise" in the experiments. Namely, 20 minutes is rather long time, so some participants may use the time to relax (with possibility to even fall asleep) while others may focus on tDCS sensations or start ruminating or excessively thinking about some tDCS unrelated topics. There is evidence to suggest that function-relevant but not tiring activity performed during tDCS has the potential to promote tDCS effects50. For these reasons, in our experiments, participants perform either practice trials of the memory tasks to be used as outcome measures or similar memory tasks. Practice trials are good choice because they engage the same neural networks as the target function but are easier and therefore not frustrating or tiring for the participants. Besides that, performing practice trials during stimulation is economical in a sense that it cuts down the testing time following tDCS, which comes as a benefit especially when the study design includes multiple tasks to be completed post-tDCS. However, the practice trials are usually much shorter than 20 minutes, thus alternative activity needs to be presented too. For this purpose, we have used common memory games40, that keep the participants focused, help them pass the time and keep the mind off the tDCS induced sensations and make them overall more comfortable in the testing setting. A few things to keep in mind when choosing the memory task to be performed during tDCS are that the task should not be difficult but also not boring (adaptive tasks set at 80% success rate are good in this context); the task should not have the material that might interfere with subsequent memory assessment (e.g., when assessing memory for faces and words, one can use abstract images/shapes pairs). Another important issue is the duration of the "habituation period" i.e., how long after the beginning of stimulation should participants start to perform the "distraction activity". There are individual differences in the intensity of the sensation and habituation times, but majority of participants will be ready to start the activity after 3-5 minutes of stimulation.
Cutaneous sensations. Some participants may be more sensitive to cutaneous tDCS effects, thus reporting elevated levels of discomfort, although this does not happen very often. It is important to inform participants about potential sensations they might experience prior the experiment. If someone is afraid of the procedure, we often let participants "feel" the current on their hand before putting the sponges on their head. The participants should be continuously monitored and asked to provide feedback on their level of comfort and sensations at regular intervals. If the participant reports increased level of discomfort, always offer to abort the experiment. It is essential that the participants are aware that the stimulation can be stopped at any time if they ask. If participant decides to stop the stimulation, the current should be slowly turned down (abrupt cancelation of the stimulation protocol may induce even stronger sensations). It is often recommended that in the case of unpleasant sensations the current intensity is temporarily lowered to the highest comfortable level, until participant adjusts, and then gradually returned to the target intensity. This seems like an appropriate alternative to stopping the stimulation protocol, especially if tDCS is used in clinical setting. However, when tDCS is used for the research purposes, and especially in relatively small samples, it is essential that all participants undergo the same procedure. Therefore, stopping the experiment is preferred to lowering the intensity of the stimulation for some participants for some time.
Reporting tDCS methodology and monitoring for potential confounds. The tDCS research field is highly heterogeneous regarding methods and measures, thus it is important to clearly report all aspects of the tDCS procedure, including blinding procedure and assessment; the head-positioning of the target as well as the position of the return electrode; the size and shape of the electrodes; type of conducting substance used (saline or gel); the current intensity (mA) and density (mA/cm2) as well as the duration of fade-in/out period; the impedance levels if measured; the duration of the stimulation (including the fade-in/out period); the detailed account of the activities participants were engaged in during the stimulation; the timing and the duration of the cognitive tasks following the stimulation (including break-times, if any). This type of information facilitates standardization and systematic analysis of the published studies (see recent review for example51). The aspects that are rarely reported on are the effect of potentially moderating/confounding variables such as time of the day of tDCS session, level of tiredness/mood reported by the participants, successfulness of blinding (i.e., beliefs about the type of stimulation they are receiving), the order of experimental sessions in within-subject designs, etc. Most of these variables have been reported to modulate the effects of tDCS, but their effect remains understudied and inconsistently reported. Therefore, tDCS studies should ensure to collect and report on any potentially confounding variables; for details on good practices see Tables 10A, 10B, 11 by Antal and colleagues34.
Application of the described protocol for anodal tDCS either in its standard or, even more, in its advanced form (i.e., oscillatory-modulated tDCS) provides a mean not only for enhancement of memory functions (and prospective use in clinical populations), but also allows for investigation of the neurobiology of the functional neural networks behind these functions.
Disclosures
Authors have no conflicting interests to disclose
Acknowledgements
This research was supported by the Science Fund of the Republic of Serbia, PROMIS, grant no. #6058808, MEMORYST
Materials
| Name | Company | Catalog Number | Comments |
| Adjustable silicone cap | |||
| Alcohol | |||
| Comb | |||
| Cotton pads | |||
| Measuring tape | |||
| Rubber electrodes | |||
| Saline solution | |||
| Single-use mini silicon hair bands | |||
| Skin marker | |||
| Sponge pockets | |||
| Syringe | |||
| tDCS device |
References
- Baddeley, A. Working memory: Looking back and looking forward. Nature Reviews Neuroscience. 4, 829-839 (2003).
- Aurtenetxe, S., et al. Interference Impacts Working Memory in Mild Cognitive Impairment. Frontiers in Neuroscience. 10, 443 (2016).
- Chen, P. C., Chang, Y. L. Associative memory and underlying brain correlates in older adults with mild cognitive impairment. Neuropsychologia. 85, 216-225 (2016).
- Bastin, C., et al. Associative memory and its cerebral correlates in Alzheimer's disease: Evidence for distinct deficits of relational and conjunctive memory. Neuropsychologia. 63, 99-106 (2014).
- McKhann, G. M., et al. The diagnosis of dementia due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's & Dementia. 7, 263-269 (2011).
- Bopp, K. L., Verhaeghen, P. Aging and Verbal Memory Span: A Meta-Analysis. Journals of Gerontology: Social Sciences section of The Journal of Gerontology Series B. 60, 223-233 (2005).
- Chalfonte, B. L., Johnson, M. K. Feature memory and binding in young and older adults. Memory & Cognition. 24, 403-416 (1996).
- Livingston, G., et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 396, 413-446 (2020).
- Dharmarajan, T. S., Gunturu, S. G. Alzheimer's disease: A healthcare burden of epidemic proportion. American Health & Drug Benefits. 2, 39-47 (2009).
- Stites, S. D., Harkins, K., Rubright, J. D., Karlawish, J. Relationships between cognitive complaints and quality of life in older adults with mild cognitive impairment, mild Alzheimer disease dementia, and normal cognition. Alzheimer Disease and Associated Disorders. 32, 276-283 (2018).
- Montejo, P., Montenegro, M., Fernández, M. A., Maestú, F. Memory complaints in the elderly: Quality of life and daily living activities. A population based study. Archives of Gerontology and Geriatrics. 54, 298-304 (2012).
- Hussenoeder, F. S., et al. Mild cognitive impairment and quality of life in the oldest old: a closer look. Quality of Life Research. 29, 1675-1683 (2020).
- Mol, M., et al. The effect of percieved forgetfulness on quality of life in older adults; a qualitative review. International Journal of Geriatric Psychiatry. 22, 393-400 (2007).
- Malkani, R. G., Zee, P. C. Brain Stimulation for Improving Sleep and Memory. Sleep Medicine Clinics. 15, 101-115 (2020).
- Sandrini, M., Manenti, R., Sahin, H., Cotelli, M. Effects of transcranial electrical stimulation on episodic memory in physiological and pathological ageing. Ageing Research Reviews. 61, (2020).
- Manenti, R., Cotelli, M., Robertson, I. H., Miniussi, C. Transcranial brain stimulation studies of episodic memory in young adults, elderly adults and individuals with memory dysfunction: A review. Brain Stimulation. 5, 103-109 (2012).
- Filmer, H. L., Dux, P. E., Mattingley, J. B. Applications of transcranial direct current stimulation for understanding brain function. Trends in Neuroscience. 37, 742-753 (2014).
- Stagg, C. J., Antal, A., Nitsche, M. A. Physiology of Transcranial Direct Current Stimulation. Journal of ECT. 34, 144-152 (2018).
- Bikson, M., et al. Safety of Transcranial Direct Current Stimulation: Evidence Based Update 2016. Brain Stimulation. 9, 641-661 (2016).
- Brunoni, A. R., et al. A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. International Journal of Neuropsychopharmacology. 14, 1133-1145 (2011).
- Owen, A. M., McMillan, K. M., Laird, A. R., Bullmore, E. N-back working memory paradigm: A meta-analysis of normative functional neuroimaging studies. Human Brain Mapping. , 46-59 (2005).
- Staresina, B. P., Henson, R. N. A., Kriegeskorte, N., Alink, A. Episodic Reinstatement in the Medial Temporal Lobe. Journal of Neuroscience. 32, 18150-18156 (2012).
- Bai, S., Loo, C., Dokos, S. A review of computational models of transcranial electrical stimulation. Critical Reviews in Biomedical Engineering. 41, 21-35 (2013).
- Esmaeilpour, Z., et al. Methodology for tDCS integration with fMRI. Human Brain Mapping. 41, 1950-1967 (2020).
- Gandiga, P. C., Hummel, F. C., Cohen, L. G. Transcranial DC stimulation (tDCS): A tool for double-blind sham-controlled clinical studies in brain stimulation. Clinical Neurophysiology. 117, 845-850 (2006).
- Lang, S., Gan, L. S., Alrazi, T., Monchi, O. Theta band high definition transcranial alternating current stimulation, but not transcranial direct current stimulation, improves associative memory performance. Scientific Reports. 9, (2019).
- Vulić, K., Bjekić, J., Paunović, D., Jovanović, M., Milanović, S., Filipović, S. R. Theta-modulated oscillatory transcranial direct current stimulation over posterior parietal cortex improves associative memory. Scientific Reports. 11, 3013 (2021).
- Pahor, A., Jaušovec, N. The effects of theta and gamma tacs on working memory and electrophysiology. Frontiers in Human Neuroscience. 11, 651 (2018).
- Dedoncker, J., Brunoni, A. R., Baeken, C., Vanderhasselt, M. A. The effect of the interval-between-sessions on prefrontal transcranial direct current stimulation (tDCS) on cognitive outcomes: a systematic review and meta-analysis. Journal of Neural Transmission. 123, 1159-1172 (2016).
- Sarkis, R. A., Kaur, N., Camprodon, J. A. Transcranial Direct Current Stimulation (tDCS): Modulation of Executive Function in Health and Disease. Current Behavioral Neuroscience Reports. 1, 74-85 (2014).
- Mitra, S., Mehta, U. M., Binukumar, B., Venkatasubramanian, G., Thirthalli, J. Statistical power estimation in non-invasive brain stimulation studies and its clinical implications: An exploratory study of the meta-analyses. Asian Journal of Psychiatry. 44, 29-34 (2019).
- Faul, F., Erdfelder, E., Lang, A. G., Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods (Psychonomic Society Inc.). , 175-191 (2007).
- Coffman, B. A., Clark, V. P., Parasuraman, R. Battery powered thought: Enhancement of attention, learning, and memory in healthy adults using transcranial direct current stimulation. Neuroimage. 85, 895-908 (2014).
- Antal, A., et al. Low intensity transcranial electric stimulation: Safety, ethical, legal regulatory and application guidelines. Clinical Neurophysiology. 128, 1774-1809 (2017).
- Mayer, J. D., Gaschke, Y. N. The experience and meta-experience of mood. Journal of Personality and Social Psychology. 55, 102-111 (1988).
- Berryhill, M. E., Wencil, E. B., Branch Coslett, H., Olson, I. R. A. A selective working memory impairment after transcranial direct current stimulation to the right parietal lobe. Neuroscience Letters. 479, 312-316 (2010).
- Berryhill, M. E., Jones, K. T. tDCS selectively improves working memory in older adults with more education. Neuroscience Letters. 521, 148-151 (2012).
- Živanović, M., et al. The Effects of Offline and Online Prefrontal vs Parietal Transcranial Direct Current Stimulation (tDCS) on Verbal and Spatial Working Memory. Neurobiology of Learning and Memory. 179, 107398 (2021).
- Bjekić, J., et al. The immediate and delayed effects of single tDCS session over posterior parietal cortex on face-word associative memory. Behavioural Brain Research. 366, 88-95 (2019).
- Bjekić, J., Čolić, V. M., Živanović, M., Milanović, D. S., Filipović, R. S. Transcranial direct current stimulation (tDCS) over parietal cortex improves associative memory. Neurobiology of Learning and Memory. 157, 114-120 (2019).
- Lee, C., Jung, Y. J., Lee, S. J., Im, C. H. COMETS2: An advanced MATLAB toolbox for the numerical analysis of electric fields generated by transcranial direct current stimulation. Journal of Neuroscience Methods. 277, 56-62 (2017).
- Berryhill, M. E. Hits and misses: leveraging tDCS to advance cognitive research. Frontiers in Psychology. 5, (2014).
- Kuo, M. F., Nitsche, M. A. Effects of transcranial electrical stimulation on cognition. Clinical EEG and Neuroscience. 43, 192-199 (2012).
- DaSilva, A. F., Volz, M. S., Bikson, M., Fregni, F. Electrode positioning and montage in transcranial direct current stimulation. Journal of Visualized Experiments. , 2744 (2011).
- Reinhart, R. M. G., Cosman, J. D., Fukuda, K., Woodman, G. F. Using transcranial direct-current stimulation (tDCS) to understand cognitive processing. Attention, Perception, & Psychophysics. 79, 3-23 (2017).
- Santarnecchi, E., et al. Enhancing cognition using transcranial electrical stimulation. Current Opinion in Behavioral Sciences. 4, 171-178 (2015).
- Woods, A. J., et al. A technical guide to tDCS, and related non-invasive brain stimulation tools. Clinical Neurophysiology. 127, 1031-1048 (2016).
- Imburgio, M. J., Orr, J. M. Effects of prefrontal tDCS on executive function: Methodological considerations revealed by meta-analysis. Neuropsychologia. 117, 156-166 (2018).
- Lally, N., Nord, C. L., Walsh, V., Roiser, J. P. Does excitatory fronto-extracerebral tDCS lead to improved working memory performance. F1000Research. 2, (2013).
- Nozari, N., Woodard, K., Thompson-Schill, S. L. Consequences of cathodal stimulation for behavior: When does it help and when does it hurt performance. PLoS One. 9, (2014).
- Hoebeke, Y., Desmedt, O., Özçimen, B., Heeren, A. The impact of transcranial Direct Current stimulation on rumination: A systematic review of the sham-controlled studies in healthy and clinical samples. Comprehensive Psychiatry. 106, 152226 (2021).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved