Comprehensive Breast Exam
Source:
Alexandra Duncan, GTA, Praxis Clinical, New Haven, CT
Tiffany Cook, GTA, Praxis Clinical, New Haven, CT
Jaideep S. Talwalkar, MD, Internal Medicine and Pediatrics, Yale School of Medicine, New Haven, CT
Breast exams are a key part of an annual gynecological exam and are important for all patients, no matter their sex or gender expression. One out of every 8 women will be diagnosed with breast cancer; male breast cancer, though less common, has a lifetime incidence of 1 in 1000.
Breast exams can feel invasive to patients, so it is important to do everything possible to make the patients feel comfortable and empowered, rather than vulnerable. Examiners should be aware of what they are communicating, both verbally and non-verbally, and give their patients control wherever possible (for instance, always allowing them to remove their own gowns). Examiners may choose to utilize chaperones for the patients' (as well as their own) comfort. Some institutions require the use of chaperones.
While it is always important to avoid overly clinical language, certain colloquial words can cross the line from caring to overly intimate in this exam. It is helpful to avoid the words "touch" and "feel" in this exam, as this language can feel sexualized. Instead, use words like "assess," "check," or "examine."
Additionally, the best practice dictates avoiding assumptions about patients' gender, as patients with female anatomy may identify as another gender (e.g., transgender, genderqueer, etc.). This video depicts the approach to patients whose history has revealed no specific complaints or risk factors related to breast health.
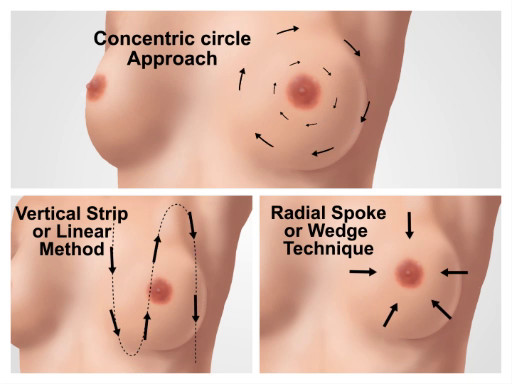
In order to avoid missing potential findings, the breast exam should be performed in a systematic approach and consist of three main components: visual inspection of the breast tissue, palpation of the lymph nodes, and palpation of breast tissue.
The breast tissue extends from directly under the clavicle to around the fifth rib (or bra line). Laterally, it extends from the midaxillary line to the sternal border. The breast is viewed in four quadrants; the upper outer quadrant has the most tissue and is the location of many lymph nodes, and the tail of Spence (or axillary tail) extends to the edge of the axilla, where it attaches to the chest wall (Figure 1).
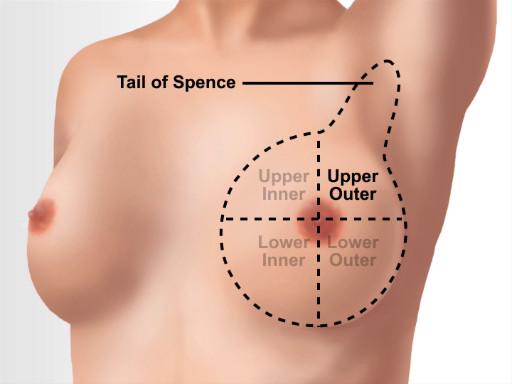
Figure 1. Breast anatomical landmarks.
1. Preparation
- Before beginning the breast exams, establish an expectation of comfort, and ask the patient to communicate questions and concerns during the visit. For example, say something like, "Have you had an exam like this before? How was that experience for you? I expect this to be a comfortable exam. If there is anything I can do to make this more comfortable for you, please let me know and I will make any adjustments I can. You may ask me questions at any time."
- Clean your hands. Som
This video covers how to perform the clinical breast exam and how to visually inspect and examine breast tissue and associated lymph nodes. Before the breast exam is started, the examiner should establish the expectation that the patient can communicate questions and concerns during the visit. The patient should be asked to remove the gown only when necessary and reminded when to raise the gown during the exam. This minimizes feelings of vulnerability.
The clinician should begin with an overvi
Skip to...
Videos from this collection:

Now Playing
Comprehensive Breast Exam
Physical Examinations II
85.6K Views

Eye Exam
Physical Examinations II
75.9K Views

Ophthalmoscopic Examination
Physical Examinations II
66.7K Views

Ear Exam
Physical Examinations II
53.7K Views

Nose, Sinuses, Oral Cavity and Pharynx Exam
Physical Examinations II
64.6K Views

Thyroid Exam
Physical Examinations II
103.5K Views

Lymph Node Exam
Physical Examinations II
381.3K Views

Abdominal Exam I: Inspection and Auscultation
Physical Examinations II
200.7K Views

Abdominal Exam II: Percussion
Physical Examinations II
245.6K Views

Abdominal Exam III: Palpation
Physical Examinations II
137.5K Views

Abdominal Exam IV: Acute Abdominal Pain Assessment
Physical Examinations II
66.5K Views

Male Rectal Exam
Physical Examinations II
112.5K Views

Pelvic Exam I: Assessment of the External Genitalia
Physical Examinations II
300.0K Views

Pelvic Exam II: Speculum Exam
Physical Examinations II
148.3K Views

Pelvic Exam III: Bimanual and Rectovaginal Exam
Physical Examinations II
145.5K Views
Copyright © 2025 MyJoVE Corporation. All rights reserved