需要订阅 JoVE 才能查看此. 登录或开始免费试用。
Method Article
评价L-DOPA诱导的运动障碍在帕金森病单侧6-OHDA病变大鼠模型中
摘要
左旋多巴诱导的运动障碍的啮齿动物模型是确定治疗干预措施的宝贵工具,以减轻发展或减轻由于反复施用左旋多巴而出现的表现.该协议演示了如何在帕金森病的单侧6-OHDA病变大鼠模型中诱导和分析运动障碍样运动。
摘要
左旋多巴诱导的运动障碍 (LID) 是指帕金森病患者长期服用左旋多巴引起的运动并发症 (PD).在临床上观察到的最常见的模式是峰值剂量运动障碍,包括舞蹈样、肌张力障碍和弹道运动的临床表现。PD的6-羟基多巴胺(6-OHDA)大鼠模型模仿了LIDS的几个特征。重复左旋多巴给药后, 6-OHDA 病变的大鼠表现出运动障碍样运动 (例如, 异常不自主运动, AIMs).该协议展示了如何在黑质纹状体途径中具有90%-95%多巴胺能消耗的6-OHDA病变大鼠中诱导和分析AIM。重复给药(3周)左旋多巴(5毫克/千克,与12.5毫克/千克苄丝肼联合)可诱导AIM的发展。时程分析显示 30-90 分钟时 AIM 显着增加(峰值剂量运动障碍)。LID的啮齿动物模型是确定有效抗运动障碍干预措施的重要临床前工具。
引言
多巴胺前体L-3,4-二羟基苯丙氨酸(L-DOPA)是帕金森病(PD)运动症状最有效的治疗方法1。左旋多巴治疗可能会改善与帕金森病相关的运动症状,但随着时间的推移会失去效果.运动波动,如"磨损波动"或"剂量结束恶化"在临床上表现为单次 l-DOPA 剂量的作用持续时间缩短2.在其他情况下,临床表现包括缓慢扭转运动和异常姿势(肌张力障碍)3 ,并在多巴胺水平低时发生(非经期肌张力障碍)4。另一方面, 左旋多巴诱导的运动障碍 (LID) 当血浆和大脑中的多巴胺水平高时出现5.
LID 会产生使人衰弱的副作用,包括舞蹈样、肌张力障碍和弹道6 运动等运动并发症。一旦建立, LID 发生在每次 l-DOPA 给药后.40%-50%接受左旋多巴治疗的PD患者发生运动并发症5年,发病率随年增加7。虽然PD患者LIDs发展的病理生理机制尚未完全阐明,但多巴胺能去神经支配的程度,脉动性L-DOPA给药,纹状体蛋白和基因的下游变化以及非多巴胺递质系统的异常是导致这些不良副作用发展的因素6,8,9,10。
神经毒素6-羟基多巴胺(6-OHDA)是研究啮齿动物PD的良好表征工具11,12,13,14。由于6-OHDA不穿过血脑屏障,因此必须直接注射到黑质纹状体通路中。6-OHDA诱导的多巴胺能耗竭是浓度和位点依赖性的15。在内侧前脑束(MFB)单侧施用6-OHDA可在啮齿动物中产生严重的(>90%)黑质纹状体损伤16,17,18,19。长期给予左旋多巴对严重的单侧 6-OHDA 病变啮齿动物会导致出现运动障碍样运动,称为异常不自主运动 (AIM).啮齿动物的运动障碍样运动具有与PD患者LID相关的相似分子,功能和药理学机制5。因此,6-OHDA病变的大鼠20和小鼠21是研究LID的有价值的临床前模型。当用治疗剂量的左旋多巴(5-20mg / kg)长期治疗(7-21天)时,单侧6-OHDA病变的大鼠和小鼠显示出影响前肢,躯干和对侧病变的口面部肌肉的AIM的逐渐发展17,18,19,20,22,23,24.这些运动在类似于 PD 患者中左旋多巴诱导的峰值剂量运动障碍的时间过程呈现25,其特征是运动过度和肌张力障碍5.AIM通常根据其严重程度(例如,当存在特定AIM时)和振幅(例如,以每个运动的振幅为特征)进行评分5,23,25。
6-OHDA病变的LID啮齿动物模型呈现面部有效性(即,该模型具有几个看起来像人类状况的特征)5,11,26,27,28。啮齿动物AIM与PD患者发生的情况类似,被视为运动过度(前肢和口舌)和肌张力障碍(轴向)运动29,并类似于峰值剂量运动障碍。在分子和功能水平上,啮齿动物模型与PD患者5具有许多病理特征,例如FosB / ΔFosB19,26,30,31,32,33和血清素转运蛋白(SERT)的上调34,35.关于预测有效性,降低PD患者LID的药物(例如,N-甲基-D-天冬氨酸(NMDA)受体拮抗剂金刚烷胺)在啮齿动物模型中具有抗运动失调功效22,36,37,38,39。
啮齿动物 AIM 评定量表基于四种 AIM 亚型创建,包括影响头部、颈部和躯干的 AIM(轴向 AIM)、多动性前肢运动(肢体 AIM)和运动障碍样口语运动(口语 AIM)。尽管对侧旋转(机车AIMs)也存在于单侧病变的啮齿动物20,22,23,25,40中,但它尚未被评分为运动障碍样运动,因为它可能不代表LIDs的特定测量22,37,41。
在这里,我们将描述如何在PD的严重(>90%)单侧6-OHDA病变大鼠模型中诱导和分析运动障碍样运动(轴向,肢体和口舌AIM)。我们根据以前的文献和实验室专业知识组织了我们的方案。
研究方案
所有实验均按照里贝朗·普雷图哲学、科学和文学学院伦理委员会(CEUA/FFCLRP 18.5.35.59.5)进行。
1. 6-OHDA病变
- 在实验开始时(6周)使用体重为200-250g的Sprague-Dawley雄性大鼠。在标准实验室条件下(12:12小时光照/黑暗循环,06:00点亮灯,温控设施(22-24°C), 随意提供食物和水。
注意:有关如何产生严重的6-OHDA病变大鼠的完整描述在别处描述42。 - 在任何实验程序开始之前适当地适应动物。
- 手术前30分钟给予(腹膜内,ip)去甲肾上腺素转运蛋白抑制剂丙咪嗪(20mg / kg,溶解在0.9%盐水溶液中)。
注意:丙咪嗪给药将增加多巴胺能神经元的6-OHDA选择性。 - 腹腔内给予氯胺酮/甲苯噻嗪(70/10mg / kg)。
- 确保动物因对脚趾捏没有反应而深度麻醉,并放置在加热垫顶部立体定位装置中的俯卧位置。
- 去除头上的皮毛并对手术区域进行 3 次消毒,在碘基磨砂膏和酒精之间交替进行。
- 使用手术刀在显微注射的区域切开(约1厘米)。
- 用棉签清洁头骨区域,并确保布雷格玛和Lambda暴露在外。
- 确保 MFB 立体定位坐标取自前胸43,44,45:前部 -4.3 毫米,横向 1.6 毫米(右侧)和腹侧 8.3 毫米(来自硬脑膜)。
- 使用 50 μL 汉密尔顿玻璃注射器在右内侧前脑束 (MFB) 中以 0.4 μL/min 的速率(10 μg 在含有 0.1% 抗坏血酸的 4 μL 盐水溶液中)单侧施用 6-OHDA。
- 在手术结束时,缝合头皮切口并用温热(~37°C)无菌0.9%盐水溶液(~10mL / kg,sc.C.)对动物进行再水化。
- 将动物从立体定位框架中取出,并将其放入加热的恢复笼中。监测直到恢复意识。
- 使用步进试验评估病变后 4 周多巴胺能病变的有效性46,47。
注意:在该测试中,通过前爪对侧对病变的调整步骤数来评估病变前肢对侧的运动不能。对侧前肢出现三个或更少调整步骤的大鼠被纳入研究,作为推定的严重6-OHDA病变大鼠48。
2. 左旋多巴慢性治疗
- 周一开始慢性治疗,6-OHDA病变后4周。
注意:由于AIMs将每周连续3天(周三,周四和周五)录像3周,因此建议在周一开始治疗。 - 用新鲜制备的左旋多巴(通过皮下(皮下),1mL / kg)加盐酸苄丝肼(分别为5mg / kg和12.5mg / kg)治疗大鼠3周,周一至周五每天一次45。
注意: 一旦建立, 目标将随着左旋多巴的每次给药而显现.因此, 左旋多巴给药 2-4 在 3 周诱导期后每周一次足以维持 AIMs 的稳定表达48.
3. 目标记录和评分
- 在09:00h和17:00h之间进行实验。确保研究者完全不知道大鼠的身份和药物治疗。
- 小心地将大鼠放入透明圆柱体(直径20厘米x 40厘米高)中,使其适应至少15分钟。确保地板上用品覆盖。镜子必须放置在圆柱体后面,以便实验者可以从所有可能的角度观察动物。
注意:如果每个实验有多个大鼠,则每只大鼠使用一个圆筒。在会话之间对动物的操作会干扰行为分析。 - 以有利于查看轴向、肢体和口舌目标的方式放置高分辨率摄像机。由于在这些实验条件下存在旋转行为,因此圆柱体后面的镜子将允许以360°角跟踪AIM。使用三脚架或将相机直接固定在工作台上。
注意:Orolingual AIM 的评分可能具有挑战性,尤其是在旋转行为发生率高的情况下。使用相机放置在略低于动物15°角的平面下方拍摄视频将有助于观察这种运动亚型。 - 轻轻地将动物从圆筒中取出并施用左旋多巴(5毫克/公斤与12.5毫克/公斤苄丝肼,皮下)。
- 将动物放回圆筒中,并在注射左旋多巴后启动计时器以跟踪目标.使用摄像机记录目标 180 注射左旋多巴后分钟.虽然可以通过直接观察动物进行分析,但最好进行离线评分。
注意: 确保计时器也被录像,以便可以在 l-DOPA 给药后的精确时间对 AIM 进行评分. - 以 30 分钟的间隔对 AIM 进行评分,直到 L-DOPA 注射后 180 分钟(定义见 表 1 ),如最初描述的那样20,23.评分必须在1-2分钟期间给出,并分为轴向、肢体或口舌(图1)。
- 仔细观察每个 AIM 并针对严重程度和振幅进行属性评分。有关说明,请使用 表 1 。不要在评级中包含正常行为,例如饲养、嗅闻、梳理和啃咬。总共将有六个观察期(30、60、90、120、150 和 180 分钟)。
| 亚 |
| 轴向:头部、颈部和躯干扭转 |
| 肢体:远端和近端前肢的不自主运动 |
| 口语:口面部肌肉的不自主运动 |
| 严厉 |
| 0:缺席 |
| 1:偶尔(有中断,在不到一半的观察时间内出现) |
| 2:频繁(有中断,但超过一半的观察时间存在) |
| 3:连续但被外部感官刺激打断 |
| 4:连续且不受外界感官刺激干扰 |
| 波幅 |
| 轴的 |
| 1:头部和颈部扭转约30°角 |
| 2:头部和颈部扭转约30°<角度≤60° |
| 3:头部、颈部和上躯干扭转约60°<角度≤90° |
| 4:头部、颈部和躯干>90°角扭转,常导致大鼠失去平衡 |
| 肢体 |
| 1:远端前肢的小不自主运动 |
| 2:低振幅运动导致前肢远端和近端易位 |
| 3:整个肢体的不自主运动,包括肩部肌肉 |
| 4:强力的肢体和肩部运动,通常类似于弹道 |
| 奥罗语 |
| 1:口面部肌肉的小不自主运动 |
| 2:高振幅的口面部运动伴舌头突出 |
表1:AIMS的定义和评级标准。
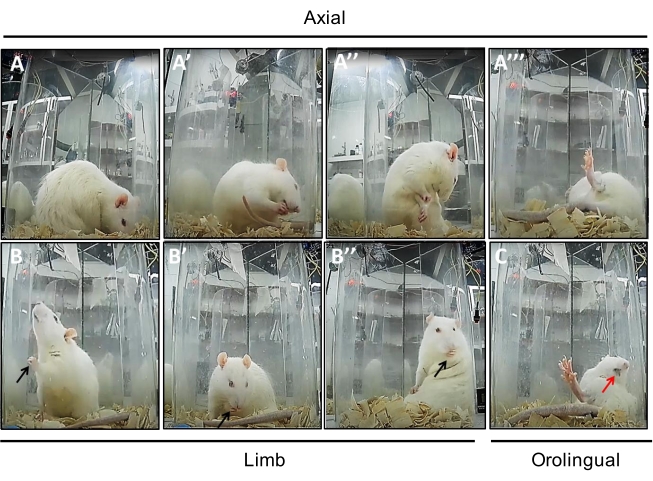
图 1:显示每个 AIM 亚型的照片序列。 (A 到 A'")轴向 AIM 显示不同角度的肌张力障碍样运动(A:30° 角,A':30° <角≤ 60°,A":60° <角≤ 90°,A'":> 90° 角)。(B 至 B")肢体AIM(黑色箭头)显示远端(B和B')和整个前肢(包括肩膀,B")的不自主运动。(C)高振幅的舌头AIM(红色箭头)伴舌头突出。 请点击此处查看此图的大图。
4. 数据分析
- 通过将左旋多巴给药后每个观察期(即六个观察期)的严重程度和幅度分数相乘来计算轴向、肢体或口舌 AIM 亚型,如前所述20.一只动物在一次测试中可以累积的理论最高分是240分(每个观察期的最高分是40分,详见 表1 )。
- 绘制周三、周四和周五记录的所有六个观察期的 AIM 评分 3 周的慢性左旋多巴给药(图 2).AIMs可以总结为表示每只动物在每个评分日(图3)或每周(图4)的最高分数 3周的慢性左旋多巴给药.
- 在选择统计分析方法之前,请验证数据是否具有接近正态分布。
注意:AIMs评级量表由有序数据组成,可以使用非参数统计量进行分析。在重复测试会话后比较实验组的AIMs分数时,广泛使用参数测试40。
结果
尽管与在人类和非人灵长类动物中观察到的AIMs模式相比,在大鼠中观察到的AIMs模式更简单且有限,但该模型再现了由慢性左旋多巴给药引起的运动过度和肌张力障碍样运动。在这里,我们展示了从一组(n = 10)单侧6-OHDA病变大鼠收集的数据,这些大鼠长期用左旋多巴(5mg / kg组合12.5mg / kg苄丝肼)长期治疗3周(周一至周五)。请注意,图 2、图 3 和
讨论
该协议演示了如何在MFB中单侧显微注射6-OHDA诱导的PD大鼠模型中诱导和分析AIM。长期每日施用低剂量的左旋多巴(5毫克/公斤,结合12.5毫克/公斤苄丝肼)在治疗的3周内产生了AIM的发展。时间分析显示AIMs显着增加,并且在左旋多巴给药后30至90分钟之间观察到峰值剂量运动障碍。AIM 是累及轴向、四肢和口舌肌的重复且无目的的运动。此处提供的协议和数据与先前的文献22,
披露声明
作者没有利益冲突。
致谢
这项工作得到了圣保罗研究基金会(FAPESP,赠款2017/00003-0)的支持。我们感谢高等教育人员改进协调会(CAPES)。我们感谢Anthony R. West博士,Heinz Steiner博士和Kuei Y. Tseng博士的支持和指导。
材料
| Name | Company | Catalog Number | Comments |
| 6-hydroxydopamine hydrobromide | Sigma-Aldrich, USA | H6507 | Neurotoxin that produces degeneration of catecholaminergic terminals |
| Benzerazide hydrochloride | Sigma | B7283 | Peripheral dopa-decarboxylase inhibitor |
| Camera Bullet IR Turbo HD (HD-TVI) 2.8mm B | HIKVISION | DS-2CE16C0T-IRP | Camera used to record all behavior |
| Imipramine hidrochloride | Alfa Aesar | J63723 | Norepinephrine transporter inhibitor (NET) used to protect noradrenergic neurons from 6-OHDA |
| Ketamine hydrochloride | Ceva Animal Health | Anesthesia for surgical intervention | |
| L-3,4-dihydroxyphenylalanine (L-DOPA) methyl ester (hydrochloride) | Cayman Chemical Company | 16149 | Dopamine precursor |
| Mirrors | Used to observe the behavior of animals during experiments in all directions | ||
| Needles 0.30 x 13 mm | PrecisionGlide | Needles used to inject drugs | |
| Sodium chloride (NaCl) | Samtec | Salt | |
| Syringes 1 ml Sterile | BD Plastipak | Syringes used to inject drugs | |
| Transparent cylinders | Used to record animal behavior during experiments | ||
| Xylazine hydrochloride | Ceva Animal Health | Sedative, analgesic and muscle relaxant for surgical intervention |
参考文献
- Jenner, P. Molecular mechanisms of L-DOPA-induced dyskinesia. Nature Reviews. Neuroscience. 9 (9), 665-677 (2008).
- Nutt, J. G. Levodopa-induced dyskinesia: review, observations, and speculations. Neurology. 40 (2), 340-345 (1990).
- Luquin, M. R., Scipioni, O., Vaamonde, J., Gershanik, O., Obeso, J. A. Levodopa-induced dyskinesias in Parkinson's disease: clinical and pharmacological classification. Movement Disorders: Official Journal of the Movement Disorder Society. 7 (2), 117-124 (1992).
- Fabbrini, G., Brotchie, J. M., Grandas, F., Nomoto, M., Goetz, C. G. Levodopa-induced dyskinesias. Movement Disorders: Official Journal of the Movement Disorder Society. 22 (10), 1379 (2007).
- Cenci, M. A., Crossman, A. R. Animal models of l-dopa-induced dyskinesia in Parkinson's disease. Movement Disorders: Official Journal of the Movement Disorder Society. 33 (6), 889-899 (2018).
- Bastide, M. F., et al. Pathophysiology of L-dopa-induced motor and non-motor complications in Parkinson's disease. Progress in Neurobiology. 132, 96-168 (2015).
- Manson, A., Stirpe, P., Schrag, A. Levodopa-induced-dyskinesias clinical features, incidence, risk factors, management and impact on quality of life. Journal of Parkinson's Disease. 2 (3), 189-198 (2012).
- Grandas, F., Galiano, M. L., Tabernero, C. Risk factors for levodopa-induced dyskinesias in Parkinson's disease. Journal of Neurology. 246 (12), 1127-1133 (1999).
- Schrag, A., Quinn, N. Dyskinesias and motor fluctuations in Parkinson's disease. A community-based study. Brain: A Journal of Neurology. 123, 2297-2305 (2000).
- Bezard, E., Brotchie, J. M., Gross, C. E. Pathophysiology of levodopa-induced dyskinesia: potential for new therapies. Nature Reviews. Neuroscience. 2 (8), 577-588 (2001).
- Tronci, E., Shin, E., Björklund, A., Carta, M. Amphetamine-induced rotation and L-DOPA-induced dyskinesia in the rat 6-OHDA model: a correlation study. Neuroscience Research. 73 (2), 168-172 (2012).
- Duty, S., Jenner, P. Animal models of Parkinson's disease: a source of novel treatments and clues to the cause of the disease. British Journal of Pharmacology. 164 (4), 1357-1391 (2011).
- Ungerstedt, U. 6-Hydroxy-dopamine induced degeneration of central monoamine neurons. European Journal of Pharmacology. 5 (1), 107-110 (1968).
- Ungerstedt, U. Postsynaptic supersensitivity after 6-hydroxy-dopamine induced degeneration of the nigro-striatal dopamine system. Acta Physiologica Scandinavica. Supplementum. 367, 69-93 (1971).
- Kirik, D., Rosenblad, C., Bjorklund, A. Characterization of behavioral and neurodegenerative changes following partial lesions of the nigrostriatal dopamine system induced by intrastriatal 6-hydroxydopamine in the rat. Experimental Neurology. 152, 259-277 (1998).
- Zahm, D. S. Compartments in rat dorsal and ventral striatum revealed following injection of 6-hydroxydopamine into the ventral mesencephalon. Brain Research. 552 (1), 164-169 (1991).
- Padovan-Neto, F. E., Echeverry, M. B., Tumas, V., Del-Bel, E. A. Nitric oxide synthase inhibition attenuates L-DOPA-induced dyskinesias in a rodent model of Parkinson's disease. Neuroscience. 159 (3), 927-935 (2009).
- Padovan-Neto, F. E., et al. Antidyskinetic effect of the neuronal nitric oxide synthase inhibitor is linked to decrease of FosB/deltaFosB expression. Neuroscience Letters. 541, 126-131 (2013).
- Padovan-Neto, F. E., Cavalcanti-Kiwiatkoviski, R., Carolino, R. O., Anselmo-Franci, J., Del Bel, E. Effects of prolonged neuronal nitric oxide synthase inhibition on the development and expression of L-DOPA-induced dyskinesia in 6-OHDA-lesioned rats. Neuropharmacology. 89, 87-99 (2015).
- Winkler, C., Kirik, D., Björklund, A., Cenci, M. A. L-DOPA-induced dyskinesia in the intrastriatal 6-hydroxydopamine model of parkinson's disease: relation to motor and cellular parameters of nigrostriatal function. Neurobiology of Disease. 10 (2), 165-186 (2002).
- Francardo, V., et al. Impact of the lesion procedure on the profiles of motor impairment and molecular responsiveness to l-DOPA in the 6-hydroxydopamine mouse model of Parkinson's disease. Neurobiology of Disease. 42, 327-340 (2011).
- Lundblad, M., et al. Pharmacological validation of behavioural measures of akinesia and dyskinesia in a rat model of Parkinson's disease. The European Journal of Neuroscience. 15 (1), 120-132 (2002).
- Cenci, M. A., Lee, C. S., Björklund, A. L-DOPA-induced dyskinesia in the rat is associated with striatal overexpression of prodynorphin- and glutamic acid decarboxylase mRNA. The European Journal of Neuroscience. 10 (8), 2694-2706 (1998).
- Henry, B., Crossman, A. R., Brotchie, J. M. Characterization of enhanced behavioral responses to L-DOPA following repeated administration in the 6-hydroxydopamine-lesioned rat model of Parkinson's disease. Experimental Neurology. 151 (2), 334-342 (1998).
- Lee, C. S., Cenci, M. A., Schulzer, M., Björklund, A. Embryonic ventral mesencephalic grafts improve levodopa-induced dyskinesia in a rat model of Parkinson's disease. Brain: A Journal of Neurology. 123, 1365-1379 (2000).
- Andersson, M., Hilbertson, A., Cenci, M. A. Striatal fosB expression is causally linked with l-DOPA-induced abnormal involuntary movements and the associated upregulation of striatal prodynorphin mRNA in a rat model of Parkinson's disease. Neurobiology of Disease. 6 (6), 461-474 (1999).
- Lindgren, H. S., Rylander, D., Ohlin, K. E., Lundblad, M., Cenci, M. A. The "motor complication syndrome" in rats with 6-OHDA lesions treated chronically with L-DOPA: relation to dose and route of administration. Behavioural Brain Research. 177 (1), 150-159 (2007).
- Lane, E. L., Dunnett, S. . Animal Models of Movement Disorders: volume I, Neuromethods. 61, (2011).
- Carlsson, T., Carta, M., Winkler, C., Björklund, A., Kirik, D. Serotonin neuron transplants exacerbate l-DOPA-induced dyskinesias in a rat model of Parkinson's disease. Journal of Neuroscience. 27 (30), 8011-8022 (2007).
- Lundblad, M., Picconi, B., Lindgren, H., Cenci, M. A. A model of L-DOPA-induced dyskinesia in 6-hydroxydopamine lesioned mice: relation to motor and cellular parameters of nigrostriatal function. Neurobiology of Disease. 16 (1), 110-123 (2004).
- Fasano, S., et al. Inhibition of Ras-guanine nucleotide-releasing factor 1 (Ras-GRF1) signaling in the striatum reverts motor symptoms associated with L-dopa-induced dyskinesia. Proceedings of the National Academy of Sciences of the United States of America. 107 (50), 21824-21829 (2010).
- Berton, O., et al. Striatal overexpression of DeltaJunD resets L-DOPA-induced dyskinesia in a primate model of Parkinson disease. Biological Psychiatry. 66 (6), 554-561 (2009).
- Lindgren, H. S., et al. Putaminal upregulation of FosB/ΔFosB-like immunoreactivity in Parkinson's disease patients with dyskinesia. Journal of Parkinson's Disease. 1 (4), 347-357 (2011).
- Rylander, D., et al. Maladaptive plasticity of serotonin axon terminals in levodopa-induced dyskinesia. Annals of Neurology. 68 (5), 619-628 (2010).
- Smith, R., et al. The role of pallidal serotonergic function in Parkinson's disease dyskinesias: a positron emission tomography study. Neurobiology of Aging. 36 (4), 1736-1742 (2015).
- Lundblad, M., et al. Pharmacological validation of a mouse model of l-DOPA-induced dyskinesia. Experimental Neurology. 194 (1), 66-75 (2005).
- Dekundy, A., Lundblad, M., Danysz, W., Cenci, M. A. Modulation of L-DOPA-induced abnormal involuntary movements by clinically tested compounds: further validation of the rat dyskinesia model. Behavioural Brain Research. 179 (1), 76-89 (2007).
- Blanchet, P. J., Konitsiotis, S., Chase, T. N. Amantadine reduces levodopa-induced dyskinesias in parkinsonian monkeys. Movement Disorders: Official Journal of the Movement Disorder Society. 13 (5), 798-802 (1998).
- Verhagen Metman, I., et al. Amantadine as treatment for dyskinesias and motor fluctuations in Parkinson's disease. Neurology. 50 (5), 1323-1326 (1998).
- Cenci, M. A., Lundblad, M. Ratings of L-DOPA-induced dyskinesia in the unilateral 6-OHDA lesion model of Parkinson's disease in rats and mice. Current Protocols in Neuroscience. , 25 (2007).
- Dupre, K. B., et al. Effects of coincident 5- HT1A receptor stimulation and NMDA receptor antagonism on L-DOPA-induced dyskinesia and rotational behaviors in the hemi-parkinsonian rat. Psychopharmacology (Berl). 199 (1), 99-108 (2008).
- Guimarães, P. R., Bariotto-dos-Santos, K., Ribeiro, D. L., Padovan-Neto, F. E. The 6-hydroxydopamine (6-OHDA) rat model of Parkinson's disease. Journal of Visualized Experiments: JoVE. , (2021).
- Paxinos, G., Watson, C. . The Rat Brain in Stereotaxic Coordinates. , (1998).
- Tseng, K. Y., et al. Inhibition of striatal soluble guanylyl cyclase-cGMP signaling reverses basal ganglia dysfunction and akinesia in experimental parkinsonism. PloS One. 6 (11), 27187 (2011).
- Padovan-Neto, F. E., et al. Selective regulation of 5-HT1B serotonin receptor expression in the striatum by dopamine depletion and repeated L-DOPA treatment: Relationship to L-DOPA-induced dyskinesias. Molecular Neurobiology. 57 (2), 736-751 (2020).
- Olsson, M., Nikkhah, G., Bentlage, C., Bjorklund, A. Forelimb akinesia in the rat Parkinson model: Differential effects of dopamine agonists and nigral transplants as assessed by a new stepping test. Journal of Neuroscience. 15, 3863-3875 (1995).
- Chang, J. W., Wachtel, S. R., Young, D., Kang, U. J. Biochemical and anatomical characterization of forepaw adjusting steps in rat models of Parkinson's disease lesions. Neuroscience. 88, 617-628 (1995).
- Jayasinghe, V. R., Flores-Barrera, E., West, A. R., Tseng, K. Y. Frequency-dependent corticostriatal disinhibition resulting from chronic dopamine depletion: Role of local striatal cGMP and GABAAR signaling. Cerebral Cortex. 27, 625-634 (2017).
- Picconi, B., et al. Loss of bidirectional striatal synaptic plasticity in L-DOPA-induced dyskinesia. Nature Neuroscience. 6 (5), 501-506 (2003).
- Carta, M., et al. Role of striatal L-DOPA in the production of dyskinesia in 6-hydroxydopamine lesioned rats. Journal of Neurochemistry. 96 (6), 1718-1727 (2006).
- Westin, J. E., Andersson, M., Lundblad, M., Cenci, M. A. Persistent changes in striatal gene expression induced by long-term L-DOPA treatment in a rat model of Parkinson's disease. The European Journal of Neuroscience. 14 (7), 1171-1176 (2001).
- Bariotto-Dos-Santos, K., et al. Repurposing an established drug: an emerging role for methylene blue in L-DOPA-induced dyskinesia. The European Journal of Neuroscience. 49 (6), 869-882 (2018).
- Lindgren, H. S., Lane, E. L., Lane, E., Dunnett, S. Rodent Models of l-DOPA-Induced Dyskinesia. Animal Models of Movement Disorders. Neuromethods. 61, (2011).
- Doucet, J., et al. Drug-drug interactions related to hospital admissions in older adults: A prospective study of 1000 patients. Journal of the American Geriatrics Society. 44, 944-948 (1996).
- Ohlin, K. E., et al. Vascular endothelial growth factor is upregulated by L-dopa in the parkinsonian brain: implications for the development of dyskinesia. Brain: A Journal of Neurology. 134, 2339-2357 (2011).
- Jourdain, V. A., et al. Increased putamen hypercapnic vasoreactivity in levodopa-induced dyskinesia. JCI insight. 2 (20), 96411 (2017).
- Thiele, S. L., et al. Generation of a model of l-DOPA-induced dyskinesia in two different mouse strains. Journal of Neuroscience Methods. 197 (2), 193-208 (2011).
- Dos-Santos-Pereira, M., et al. Contributive role of TNF-α to L-DOPA-induced dyskinesia in a unilateral 6-OHDA lesion model of Parkinson's disease. Frontiers in Pharmacology. 11, 617085 (2021).
- Cenci, M. A., Ohlin, K. E., Odin, P. Current options and future possibilities for the treatment of dyskinesia and motor fluctuations in Parkinson's disease. CNS & Neurological Disorders Drug Targets. 10 (6), 670-684 (2011).
- Cenci, M. A. Presynaptic mechanisms of l-DOPA-induced dyskinesia: The findings, the debate, and the therapeutic implications. Frontiers in Neurology. 5, 242 (2014).
- Langston, J. W., Quik, M., Petzinger, G., Jakowec, M., Di Monte, D. A. Investigating levodopa-induced dyskinesias in the parkinsonian primate. Annals of Neurology. 47 (4), 79-89 (2000).
- Chase, T. N. Levodopa therapy: consequences of the nonphysiologic replacement of dopamine. Neurology. 50 (5), 17-25 (1998).
转载和许可
请求许可使用此 JoVE 文章的文本或图形
请求许可探索更多文章
This article has been published
Video Coming Soon
版权所属 © 2025 MyJoVE 公司版权所有,本公司不涉及任何医疗业务和医疗服务。