Esame obiettivo ginecologico II: esame con lo speculum
Fonte:
Alexandra Duncan, GTA, Praxis Clinical, New Haven, CT
Tiffany Cook, GTA, Praxis Clinical, New Haven, CT
Jaideep S. Talwalkar, MD, Medicina interna e pediatria, Yale School of Medicine, New Haven, CT
Fornire un comodo posizionamento dello speculum è un'abilità importante da sviluppare per i fornitori, poiché lo speculum è uno strumento necessario in molte procedure ginecologiche. I pazienti e i fornitori sono spesso ansiosi per l'esame speculum, ma è del tutto possibile posizionare uno speculum senza disagio del paziente. È importante che il clinico sia consapevole del ruolo che il linguaggio gioca nella creazione di un ambiente confortevole; ad esempio, un fornitore dovrebbe fare riferimento alle "fatture" dello speculum piuttosto che alle "lame" per evitare di sconvolgere il paziente.
Esistono due tipi di speculomi: metallo e plastica (Figura 1). Questa dimostrazione utilizza la plastica, poiché gli speculam di plastica sono più comunemente usati nelle cliniche per i test di routine. Quando si utilizza uno speculum metallico, si consiglia di utilizzare uno speculum Graves se il paziente ha partorito per via vaginale e uno speculum Pederson se il paziente non lo ha fatto. Gli speculomi pederson e Graves sono forme diverse ed entrambi sono disponibili in molte dimensioni diverse (il mezzo è usato più spesso). Prima di posizionare uno speculum metallico, è utile eseguire un esame cervicale digitale per valutare la dimensione dello speculum appropriata. La profondità e la direzione della cervice sono stimate posizionando un dito nella vagina. Se la cervice del paziente può essere localizzata mentre il paziente è seduto, è probabile che il paziente abbia una vagina poco profonda, e quindi dovrebbe essere più a suo agio con uno speculum metallico corto.

Figura 1. Una fotografia di speculoms disponibili in commercio in diverse dimensioni.
Gli speculam in plastica hanno tutti la forma di speculms metallici Pederson e sono disponibili in diverse dimensioni. Per valutare la dimensione appropriata per uno speculum di plastica, l'esaminatore posiziona due dita nella vagina del paziente, palmo verso il basso e cerca di separare le dita: se non c'è spazio tra le dita, deve essere usato un piccolo speculum di plastica; se c'è spazio tra le dita, dovrebbe essere usato uno medio. L'esame non dovrebbe mai essere eseguito con un grande speculum (poiché è significativamente più lungo) senza prima determinare la lunghezza del canale vaginale.
Lo speculum viene utilizzato per eseguire il test Papanicolaou come parte degli esami di screening del cancro cervicale. Il cancro cervicale era una volta la principale causa di decessi per cancro per le donne negli Stati Uniti, ma negli ultimi decenni il numero di casi e decessi è diminuito significativamente1. Questo cambiamento è attribuito alla scoperta fatta da Georgios Papanicolaou nel 1928 che il cancro cervicale poteva essere diagnosticato da strisci vaginali e cervicali. Il Pap test, come viene ora chiamato, rileva cellule anormali nella cervice, sia cancerose che precorose. Le attuali linee guida per gli intervalli di screening raccomandati sono disponibili sul sito Web della US Preventive Services Task Force (USPSTF)2.
Il test può essere eseguito utilizzando 1) un vetrino convenzionale e fissativo con spatola e pennello endocervicale (il tradizionale "Pap test") o 2) la citologia a base liquida più comunemente utilizzata con una scopa cervicale o una spatola e un pennello endocervicale (Figura 2). Indipendentemente dagli strumenti utilizzati, i campioni vengono raccolti appena all'interno del sistema operativo esterno e della giunzione squamocolona, o zona di transizione attorno al sistema operativo (Figura 3). Questo video mostra la spatola e il pennello endocervicale con citologia a base liquida, poiché la preparazione del liquido è una tecnica più efficace per il rilevamento delle lesioni cervicali e la spatola e il pennello endocervicale migliorano la raccolta dei campioni.

Figura 2. Strumenti pap test. Mostrati in sequenza sono: un contenitore di citologia liquida, una scopa cervicale, una spatola e un pennello endocervicale.
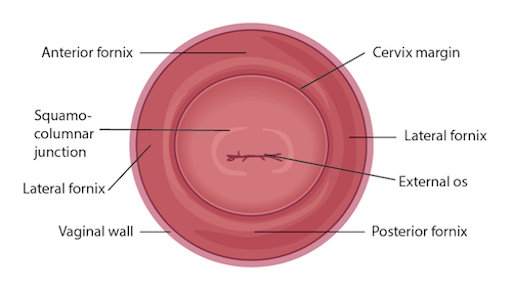
Figura 3. Diagramma della cervice construtture pertinenti etichettate.
L'esame dello speculum inizia immediatamente dopo la fine dell'esame dei genitali esterni; pertanto, il paziente ha già fornito una storia ed è nella posizione di litotomia modificata. Assicurarsi che il paziente sia seduto alla fine del tavolo, poiché lo speculum non può essere completamente inserito in nessun altro modo.
1. Preparazione
- Disadi le forniture per il Pap test.
- Etichettare il contenitore di citologia liquida con le informazioni del paziente.
- Svitare il coperchio del contenitore fino a quando non è appoggiato sulla parte superiore e può essere sollevato.
- Posiziona lo speculum nella mano non dominante e posiziona il dito indice sopra le banconote, il dito medio sotto le banconote e il pollice sul retro dello speculum (Figura 4).
- Usa la mano dominante per stendere il lubrificante a base d'acqua (o acqua calda, altrimenti) all'esterno delle bollette.
- Introdurre lo speculum e far sapere al paziente cosa aspettarsi: "Questo è uno speculum. Queste sono le bollette, che metterò nella tua vagina per vedere la cervice e prendere alcuni campioni. Questa è la maniglia, che non verrà inserita."
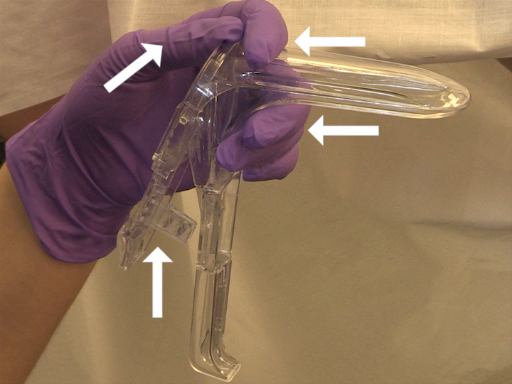
Figura 4. Come tenere uno speculum di plastica.
2. Inserimento
- Come sempre, presenta il tuo tocco al paziente prima di iniziare l'esame.
- Fai sapere al paziente che stai per posizionare il dorso della mano sulla coscia del paziente e quindi inizierai l'esame.
- Posiziona il dorso della mano all'interno della coscia del paziente, sopra il drappo, quindi inizia a esaminare: questo prepara il paziente e inizia con il contatto non invasivo, che può aiutare a mettere il paziente a proprio agio.
- Usando i cuscinetti dell'indice e del medio della tua mano dominante, separa le piccole labbra appena sopra il perineo per ottenere una visione chiara dell'introito vaginale.
- Guida il paziente attraverso una tecnica di rilassamento: "Ti insegnerò come renderlo più confortevole per te stesso. Per favore, fai un respiro profondo e, mentre espiri, sopporta come se stessi facendo un movimento intestinale. (Se il paziente non lo capisce, chiedi al paziente di spingere contro le dita.)"
- Mentre il paziente si abbatte, l'introito vaginale si apre. Fai sapere al paziente: "Sentirai che inserisco lo speculum".
- Inserire dolcemente lo speculum a circa metà strada nella vagina con un angolo obliquo (circa 45 °), angolando i becco sotto dove ci si aspetta che sia la cervice (in base all'esame digitale) mantenendo la pressione posteriore.
- Usa le prime due dita della tua mano dominante per liberare le labbra su un lato, in modo che le labbra non vengano tisse insieme allo speculum.
- Usa la tua mano dominante per liberare le labbra dall'altra parte.
- Portare la mano non dominante sul manico inferiore dello speculum, ruotare lo speculum piatto e inserirlo completamente, fino a quando l'impugnatura non è a filo contro il bacino del paziente e perpendicolare al pavimento.
- Posiziona un dito della tua mano dominante all'interno dei becco dello speculum e usa il dito per applicare una forte pressione posteriore mentre la tua mano non dominante tira verso il basso l'impugnatura dello speculum allo stesso tempo. Applicare abbastanza pressione posteriore in modo che lo spazio nella vagina possa essere visto sopra lo speculum.
- Posiziona il pollice della mano non dominante sulla leva del pollice e deprimi dolcemente.
- Non continuare a deprimere una volta soddisfatta la resistenza, oppure potresti aprire le bollette troppo lontano e causare disagio al paziente.
- Tenere lo speculum fermo e controllare se la cervice è stata localizzata.
3. Pap test
- Se c'è abbastanza scarico sulla faccia della cervice per oscurare l'os e interferire con la raccolta dei campioni, utilizzare un grande tampone con punta di cotone per eliminare delicatamente le mucose cervicali in eccesso.
- Usa la tua mano dominante per raccogliere la spatola (o fai in modo che l'accompagnatore te la consechi).
- Inserire la spatola nella vagina, facendo attenzione a non lasciarla toccare le pareti, fino a quando l'estremità lunga non riposa nel sistema operativo e la depressione e l'estremità corta vengono premute contro la giunzione squamocolondolare.
- Ruotare di 360°, mantenendo una pressione costante e il contatto con l'esocervice.
- Rimuovere la spatola, facendo attenzione a non toccare le pareti della vagina.
- Posizionare la spatola nel contenitore aperto e risciacquare accuratamente ruotando vigorosamente nel liquido (diverse marche di citologia a base liquida raccomandano di ruotare per diversi periodi di tempo; avere familiarità con la raccomandazione del produttore prima di iniziare).
- Scartare la spatola o rimetterla sul vassoio.
- Usa la tua mano dominante per raccogliere il pennello endocervicale.
- Inserire la spazzola endocervicale nella vagina, facendo attenzione a non lasciarla toccare le pareti, e inserirla delicatamente nel sistema operativo fino a quando non sono esposte solo le setole inferiori.
- Ruotare lentamente di 180° in una direzione. Non ruotare eccessivamente.
- Se si utilizza una scopa cervicale, piuttosto che una spazzola endocervicale e una spatola, inserire la scopa fino a quando le setole centrali sono nell'os e le setole più corte poggiano sulla giunzione squamocolondo, quindi ruotare cinque volte in una direzione prima di rimuovere.
- Rimuovere il pennello, facendo attenzione a non toccare le pareti della vagina.
- Posizionare la spazzola endocervicale nel contenitore aperto e risciacquare accuratamente ruotando vigorosamente e premendola ripetutamente contro i lati del contenitore per rilasciare materiale.
- Scartare il pennello endocervicale.
- Sostituire e stringere il coperchio del contenitore di citologia.
4. Rimozione dello speculum
- Posizionare il pollice non dominante sulla leva del pollice e mantenere la pressione rilasciando il meccanismo di bloccaggio.
- Continuare a tenere la leva del pollice verso il basso e rimuovere lo speculum a circa un pollice fuori per consentire alla cervice di liberare la punta delle banconote.
- Rimuovere completamente il pollice dalla leva e posizionarlo sul manico dello speculum.
- Ruotare lo speculum di 45° rimuovendolo dolcemente per il resto della via d'uscita, permettendo alle pareti vaginali di chiudere le bollette.
- Posiziona la mano dominante sotto lo speculum per catturare qualsiasi scarico.
- Scartare lo speculum di plastica, se usa e getta.
Questo video ha esaminato le tecniche per eseguire un comodo esame speculum e raccogliere i campioni per un Pap test. Prima di iniziare l'esame, l'esaminatore dovrebbe assicurarsi che tutte le forniture siano preparate e far sapere al paziente cosa aspettarsi. Essere in grado di eseguire un comodo esame speculum è un'abilità importante per qualsiasi professionista, in quanto viene utilizzato in un'ampia varietà di procedure ginecologiche e può fornire una ricchezza di informazioni. Quando lo speculum viene inserito, è possibile osservare la cervice e le pareti vaginali per una varietà di segni tra cui tono, colore, scarico, lesioni, polipi, ulcerazioni e altro ancora, tutti i quali possono essere clinicamente significativi e possono aiutare con il processo di diagnosi. Uno speculum ben inserito consente anche un facile accesso all'os cervicale, a quel punto possono essere prelevati campioni per il Pap test (così come per altri screening, come clamidia e gonorrea). È necessario utilizzare uno speculum per accedere alla cervice per molte altre procedure, tra cui l'inserimento o la rimozione di un dispositivo intrauterino (IUD), una procedura di escissione elettrochirurgica ad anello (LEEP) e altro ancora.
Molti pazienti possono provare ansia per lo speculum e sperimentarlo come la parte più invasiva dell'esame ginecologico. Il fornitore può offrire al paziente supporto generale ed empatia, insieme a strumenti specifici per rendere l'esame più confortevole per se stessi. Chiedere al paziente di fare un respiro profondo e poi sopportare come se avere un movimento intestinale prima dell'inserimento possa aprire l'introito vaginale e aiutare notevolmente il comfort. L'esaminatore può offrire a un paziente particolarmente ansioso l'opportunità di inserire lo speculum stesso posizionandolo a testa in giù con la maniglia rivolta verso il soffitto mentre il fornitore li parla attraverso l'apertura3. Spesso è più facile ottenere una visione chiara della cervice con un inserimento capovolto, ma non è una tecnica che i professionisti dovrebbero utilizzare, perché posiziona la mano dell'esaminatore direttamente contro il clitoride del paziente.
Ci sono molte cose che il praticante può fare per garantire che l'esame sia confortevole. Lo speculum deve essere inserito ad angolo obliquo per evitare di esercitare troppa pressione diretta sull'uretra. Quando lo speculum è inserito completamente, le banconote devono essere inclinate al di sotto di dove si trovava la cervice durante l'esame digitale. Il praticante può quindi applicare una pressione posteriore sufficiente allo speculum, quindi c'è spazio visibile nella vagina sopra le bollette; questo permette di aprire le banconote senza esercitare pressione sulle delicate strutture anteriori. La cosa più importante è non inserire o rimuovere mai uno speculum mentre le banconote sono aperte. Questo è molto doloroso e rischia di ferire il paziente. L'esaminatore non deve toccare la leva del pollice fino a quando lo speculum non è posizionato completamente e pronto per essere aperto. Il blocco dello speculum deve essere rilasciato completamente prima della rimozione e l'eventuale pressione deve essere mantenuta manualmente. Una volta che la cervice è libera, la leva del pollice deve essere completamente rilasciata e lo speculum rimosso senza problemi il resto del percorso, consentendo alle pareti vaginali di chiudere le banconote all'uscita.
- Cervical Cancer Statistics. U.S. Preventive Services Task Force. Centers for Disease Control and Prevention (2014).
- Cervical Cancer: Screening. Recommendation Summary. U.S. Preventive Services Task Force (2012).
- Wright, D., Fenwick, J., Stephenson, P., Monterosso, L. Speculum 'self-insertion': a pilot study. Journal of Clinical Nursing. 14(9): 1098-1111 (2005).
Vai a...
Video da questa raccolta:

Now Playing
Esame obiettivo ginecologico II: esame con lo speculum
Physical Examinations II
148.3K Visualizzazioni

Esame obiettivo dell'occhio
Physical Examinations II
75.9K Visualizzazioni

Esame oftalmoscopico
Physical Examinations II
66.7K Visualizzazioni

Esame obiettivo dell'orecchio
Physical Examinations II
53.7K Visualizzazioni

Esame di naso, seni, cavità orale e faringe
Physical Examinations II
64.6K Visualizzazioni

Esame obiettivo della tiroide
Physical Examinations II
103.5K Visualizzazioni

Esame obiettivo dei linfonodi
Physical Examinations II
381.3K Visualizzazioni

Esame obiettivo dell'addome I: ispezione e auscultazione
Physical Examinations II
200.7K Visualizzazioni

Esame obiettivo dell'addome II: percussione
Physical Examinations II
245.6K Visualizzazioni

Esame obiettivo dell'addome III: palpazione
Physical Examinations II
137.5K Visualizzazioni

Esame obiettivo dell'addome IV: valutazione del dolore addominale acuto
Physical Examinations II
66.5K Visualizzazioni

Esame rettale maschile
Physical Examinations II
112.5K Visualizzazioni

Esame completo del seno
Physical Examinations II
85.6K Visualizzazioni

Esame obiettivo ginecologico I: valutazione dei genitali esterni
Physical Examinations II
300.0K Visualizzazioni

Esame obiettivo ginecologico III: palpazione rettovaginale e bimanuale
Physical Examinations II
145.5K Visualizzazioni