Aby wyświetlić tę treść, wymagana jest subskrypcja JoVE. Zaloguj się lub rozpocznij bezpłatny okres próbny.
Method Article
Functional Transcranial Doppler Ultrasound for Monitoring Cerebral Blood Flow
W tym Artykule
Podsumowanie
Functional transcranial Doppler ultrasound complements other functional imaging modalities, with its high temporal resolution measurement of stimulus-induced changes in cerebral blood flow within the basal cerebral arteries. This Methods paper gives step-by-step instructions for using functional transcranial Doppler ultrasound to perform a functional imaging experiment.
Streszczenie
Functional transcranial Doppler ultrasound (fTCD) is the use of transcranial Doppler ultrasound (TCD) to study neural activation occurring during stimuli such as physical movement, activation of tactile sensors in the skin, and viewing images. Neural activation is inferred from an increase in the cerebral blood flow velocity (CBFV) supplying the region of the brain involved in processing sensory input. For example, viewing bright light causes increased neural activity in the occipital lobe of the cerebral cortex, leading to increased blood flow in the posterior cerebral artery, which supplies the occipital lobe. In fTCD, changes in CBFV are used to estimate changes in cerebral blood flow (CBF).
With its high temporal resolution measurement of blood flow velocities in the major cerebral arteries, fTCD complements other established functional imaging techniques. The goal of this Methods paper is to give step-by-step instructions for using fTCD to perform a functional imaging experiment. First, the basic steps for identifying the middle cerebral artery (MCA) and optimizing the signal will be described. Next, placement of a fixation device for holding the TCD probe in place during the experiment will be described. Finally, the breath-holding experiment, which is a specific example of a functional imaging experiment using fTCD, will be demonstrated.
Wprowadzenie
In neuroscience research, it is often desirable to monitor real-time brain activity noninvasively in a variety of environments. However, conventional functional neuroimaging modalities have limitations that impede the ability to capture localized and/or rapid activity changes. The true (non-jittered, non-retrospective) temporal resolution of functional magnetic resonance imaging (fMRI) is currently of the order of a few seconds1, which may not capture transient hemodynamic changes linked to transient neural activation. In another example, although functional near-infrared spectroscopy (fNIRS) has high temporal resolution (milliseconds) and reasonable spatial resolution, it can only probe hemodynamic changes within the cerebral cortex and cannot provide information about changes taking place in the larger arteries supplying the brain.
In contrast, fTCD—classified as a neuroimaging modality—“imaging” refers to the dimensions of time and space, rather than two orthogonal spatial directions that are more familiar in an “image”. fTCD provides complementary information to other neuroimaging modalities by measuring high temporal resolution (typically 10 ms) hemodynamic changes at precise locations within vessels of the basal cerebral circulation. As with other neuroimaging modalities, fTCD may be used for a variety of experiments such as studying lateralization of cerebral activation during language-related tasks2,3,4, studying neural activation in response to various somatosensory stimuli5, and exploring neural activation in various cognitive stimuli such as visual tasks6, mental tasks7, and even tool production8.
Although fTCD offers several advantages for use in functional imaging, including low cost of equipment, portability, and enhanced safety (compared to Wada test3 or positron emission tomography [PET] scans), operation of a TCD machine requires skills obtained by practice. Some of these skills, which must be learned by a TCD operator, include the ability to identify various cerebral arteries and the motor skills necessary to precisely manipulate the ultrasound probe during the search for the relevant artery. The goal of this Methods paper is to present a technique for using fTCD to perform a functional imaging experiment. First, the basic steps for identifying and optimizing the signal from the MCA, which perfuses 80% of the cerebral hemisphere9, will be listed. Next, placement of a fixation device for holding the TCD probe in place during the experiment will be described. Finally, the breath-holding experiment, which is one example of a functional imaging experiment using fTCD, will be described, and representative results will be shown.
Protokół
All human subject research was performed in accordance with the Institutional Review Board of the University of Nebraska-Lincoln, and informed consent was obtained from all subjects.
1. Locating the MCA signal by freehand TCD
NOTE: “Freehand” TCD refers to operation of TCD with a handheld transducer to find a CBFV signal before beginning an fTCD experiment.
- Setting TCD parameters
- Keep the power at a reasonably high value (e.g., 400 mW) during the initial search for the MCA. Once the MCA signal is located, reduce the power as much as possible while still maintaining a “good” signal (see step 2.2.7).
NOTE: Using a reasonably high power during the initial search does not violate the “As Low As Reasonably Achievable” (ALARA) principle of exposure to acoustic radiation because higher power will allow the MCA signal to be discovered more quickly10. - Set the sample volume to 8–12 mm during the initial search for the MCA signal. If the signal is difficult to find, increase the gate size to increase the intensity of the signal, but note that this may incorporate the signal from one or more nearby arteries into the signal from the MCA.
- Set the gain at a medium level, with the goal of “keeping background noise at a minimum, but present”10.
- Set the high-pass filter cutoff (normally termed “threshold”) to 50–150 Hz.
- If the subject is an adult, set the depth to 50 mm, which is the average mid-point depth of the M1 segment of the MCA10 (Figure 1).
NOTE: This setting will be discussed in more detail in subsequent steps. Depth settings for children are given in Table 1.
- Keep the power at a reasonably high value (e.g., 400 mW) during the initial search for the MCA. Once the MCA signal is located, reduce the power as much as possible while still maintaining a “good” signal (see step 2.2.7).
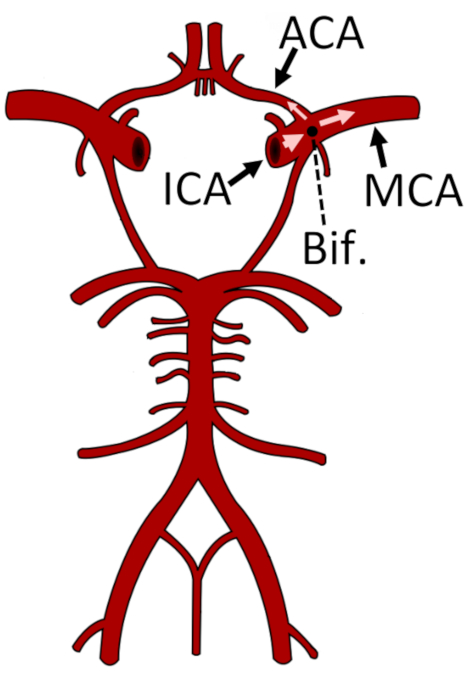
Figure 1: Representation of the circle of Willis and the major arteries of the cerebral circulatory system. The bifurcation of the ICA into the ACA and MCA is marked with a black circle. The M1 segment of the MCA is shown. This figure has been modified from24. Abbreviations: ACA = anterior cerebral artery; Bif. = bifurcation; ICA = internal carotid artery; MCA = middle cerebral artery. Please click here to view a larger version of this figure.
- Locating the temporal window
NOTE: The temporal window, also called the transtemporal acoustic window, is a part of the skull where the bone is thinnest11, thus allowing transmission of low-frequency ultrasound energy through the cranium (Figure 2).- For infants and small children, locate the temporal window just in front of the ear (the “intertragal space”) and above the rostral edge of the zygomatic arch, which can be easily felt under the skin.
- For teenagers and young adults, locate the temporal window via any of the subwindows.
NOTE: The posterior subwindow usually provides the best signal (Figure 2). - For adults aged 30 years or older, locate the temporal window just in front of the ear.
NOTE: The acoustic window decreases in size as people age due to increasing porosity of the bone of the cranium, causing some older people to have a very limited temporal window12. In such individuals, bilateral insonation of the MCA is sometimes impossible.
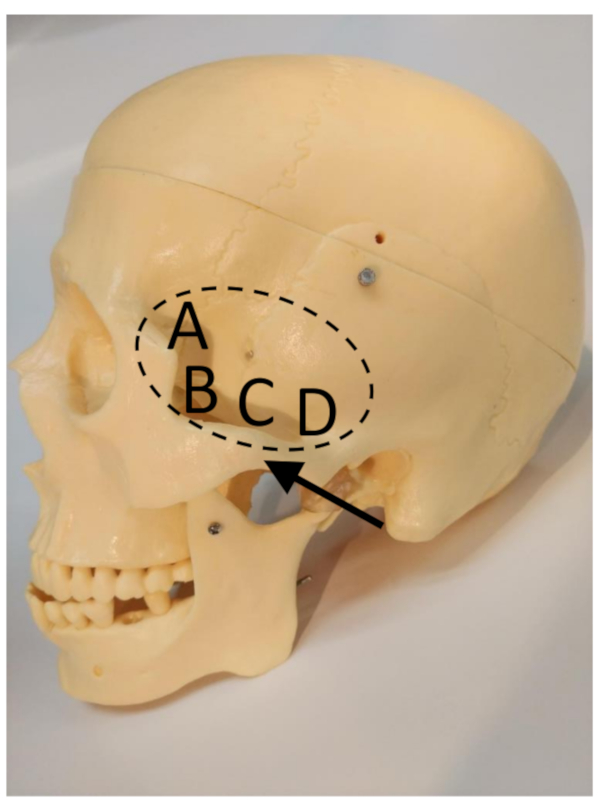
Figure 2: The transtemporal window (marked by the dashed ellipse), zygomatic arch (arrow), and subwindows11. (A) Frontal subwindow. (B) Anterior subwindow. (C) Middle subwindow. (D) Posterior subwindow. Please click here to view a larger version of this figure.
- Applying the transducer
- Apply enough ultrasound gel to cover the surface of the transducer.
NOTE: When placed on the head, the gel should cover sufficient space to maintain a seal between the scalp and the Doppler probe’s surface, thus preventing signal interruption from air coupling underneath the probe’s surface. - Alert the subject that the gel may feel cold (if at room temperature).
- Place the transducer on the temporal window, which was located in section 1.2.
- Apply enough ultrasound gel to cover the surface of the transducer.
- Searching for the MCA
- After placing the transducer on the scalp, search for the MCA signal, which will generally be located slightly anterior (forwards) and rostral (towards the head) from the location of the initial transducer scalp placement10.
- If the TCD spectral signal is not immediately obvious, adjust the angle of the transducer while keeping it in the same location relative to the scalp. Slowly angle the probe from rostral to caudal (towards feet) and posterior to anterior.
NOTE: Figure 3 shows two spectra taken from the same position, but at different angles. - If a signal is still absent after performing step 1.4.2, check the color M-mode display for flow in the MCA at different depths (indicated by red coloring). Increment or decrement the signal depth in 5 mm steps and search as described in step 1.4.2. If flow is visible in M-mode but not in the Doppler spectrum, increase or decrease the depth until the flow signal is visible in the Doppler spectrum.
- If a satisfactory signal is still not obtained, move the transducer to a nearby position on the scalp, which is slightly more anterior, and repeat steps 1.4.1–1.4.3.
- When an optimal MCA signal is obtained, note the depth and maximum velocity.
- Using a washable makeup pen, place a mark on the scalp (trace part of the transducer edge) where the optimal signal was found.
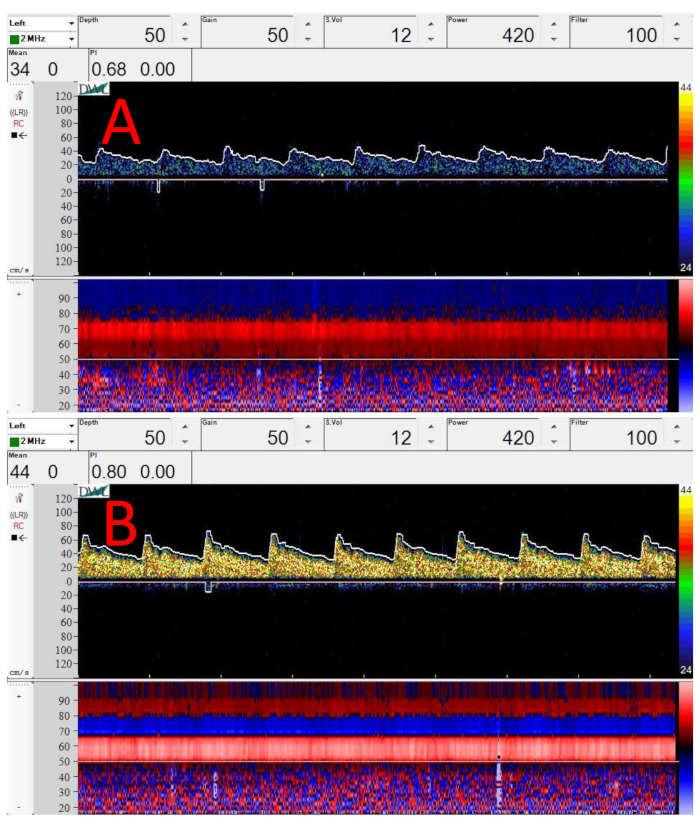
Figure 3: Sample Doppler spectra and M-mode images from midpoint of M1 segment of the MCA. (A) Spectrum taken right after applying transducer to the temporal window, just in front of the ear. (B) Sample Doppler spectrum at same location and depth as (A). The only change is that the transducer has been angled upwards (superiorly) slightly. In both (A) and (B), depth = 50 mm, gain = 50, sample volume = 12 mm, power = 420 mW/cm2, and filter = 100 Hz. Please click here to view a larger version of this figure.
- Searching for the bifurcation
NOTE: Finding the bifurcation of the internal carotid artery (ICA) is important to help confirm that the MCA is the artery being monitored. This step should be performed on both sides if bilateral monitoring will be performed, as the bifurcation may not be at the same depth on both sides.- Increase the depth until the signal from the bifurcation of the ICA into the MCA and ACA is noted (Figure 4), typically at a depth of 51–65 mm10.
- Search for the optimum bifurcation spectral signal using the procedure described in step 1.4.2. Always strive for the highest-velocity spectral signal possible10.
- When an optimal bifurcation signal is obtained, note the depth of the bifurcation.
- For bilateral monitoring, repeat sections 1.1–1.4 and steps 1.5.1–1.5.3 on the other side of the head.
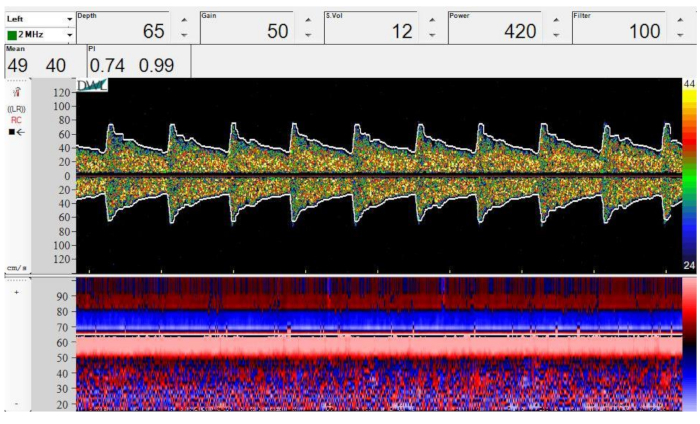
Figure 4: Spectral Doppler (top) and M-mode (bottom) image of bifurcation of the ICA into the MCA and ACA. Depth = 65 mm, gain = 50, sample volume = 12 mm, power = 420 mW/cm2, and filter = 100 Hz. Please click here to view a larger version of this figure.
2. Relocating the MCA after placing a fixation device
NOTE: For fTCD experiments, it is necessary to monitor CBFV for 10–90 min or longer. Therefore, a fixation device (Figure 5) is crucial to provide stability.
- Placing the fixation device
- By visual inspection, adjust the fixation device (Figure 5) to the subject’s approximate head size.
- Alert the subject before placing the headset on his or her head. Place the headset on the subject’s head.
NOTE: If the subject has long or thick hair, it may be necessary to tie the subject’s hair back, depending on the fixation device being used. - Adjust the fixation device’s fit, and ask the subject if the device is too tight.
NOTE: The device should be tight enough that it does not move when bumped slightly, but loose enough that the subject is not uncomfortable.

Figure 5: Subject wearing custom fixation device. Please click here to view a larger version of this figure.
- Locating the MCA signal
- Loosen the mechanism of the fixation device holding the transducer in place (e.g., loosen the mechanism, shown in in Figure 5, by turning a knob counterclockwise) so that the transducer can move freely.
- Alert the subject before applying gel to the transducers (which should already be in place from section 2.1), and that the gel may be cold (if it has been stored at room temperature).
- Apply enough ultrasound gel to the transducer to cover the face of the transducer.
- Adjust the fixation device so that the transducer is located over the top of the mark made in step 1.4.6.
- Search for the optimal MCA spectral signal using the procedure described in steps 1.4.1–1.4.3. Always strive for the highest-velocity spectral signal possible10.
NOTE: When compared to freehand TCD, the optimal depth at which the MCA is located using the fixation device may differ slightly (at most 1–2 mm) from the depth for the freehand device. This is because the fixation device may hold the transducer slightly further away from the scalp while still maintaining a coupling gel seal. - When the optimal MCA spectral signal is found, tighten the mechanism of the fixation device to lock the transducer in place. Note the depth and all other settings.
- Decrease the power (see step 1.1.1) as much as possible while still maintaining a spectral envelope that traces the maximal velocity accurately.
- For bilateral monitoring, repeat steps 2.2.1–2.2.7 on the other side.
3. Performing a breath-hold maneuver
NOTE: This section is given as an example of a functional experiment that may be performed using the experimental setup described in section 1 and section 2.
- Perform all steps described in section 1 and section 2.
- Begin recording on the TCD software.
- Breathe normally for 3 min to achieve a good baseline recording, and allow CBFV to stabilize from any previous experiments or stimuli.
- Count down slowly from three. On the count of one, ask the subject to begin breath-holding following a normal inspiration13.
NOTE: The subject should not inhale deeply, as this would decrease carbon dioxide in the lungs and decrease the likelihood of observing the increase in CBFV due to cerebrovascular reactivity. The subject should also avoid performing a Valsalva maneuver, in which intrathoracic pressure is substantially increased against a held inspiration14. - Place a marker in the TCD recording to signify the start of breath-holding.
- Have the subject hold their breath for 30 s, or until they are no longer comfortable holding their breath.
- When the subject inhales, place a marker in the TCD recording to signify the end of breath-holding.
- Continue monitoring CBFV using TCD and recording for at least 30 s following the end of breath-holding to ensure that CBFV returns to baseline values.
Wyniki
Figure 3 shows sample Doppler spectra and color M-modes from the midpoint of the M1 segment of the MCA. Figure 3A,B were taken at the same position on the scalp, but at different angles. Note how a very small change in angle, without changing the contact position on the scalp, can greatly improve Doppler signal strength, as shown by the higher-intensity yellow coloring of the spectrogram in Figure 3B. Note ...
Dyskusje
Critical steps in the protocol include 1) finding the MCA, 2) placing the headband, and 3) performing the breath-holding maneuver.
Modifications may be necessary depending on the subjects in the study. For example, subjects with Alzheimer’s disease may have difficulty following instructions, necessitating the use of a capnograph to ensure compliance with breath-holding instructions15. Young children may have difficulty following i...
Ujawnienia
The authors declare no conflicts of interest.
Podziękowania
This project is based on research that was partially supported by the Nebraska Agricultural Experiment Station with funding from the Hatch Act (Accession Number 0223605) through the USDA National Institute of Food and Agriculture.
Materiały
| Name | Company | Catalog Number | Comments |
| Aquasonic | Parker Laboratories, Inc., Fairfield, NJ, USA | 01-50 | Ultrasound Gel |
| Doppler Box X | DWL Compumedics Gmbh, Singen, Germany | Model "BoxX" | Transcranial Doppler with 2-MHz monitoring probes |
| Kimwipes | Kimberly-Clark Professional | 34256 | Delicate Task Wipers |
| Transeptic | Parker Laboratories, Inc., Fairfield, NJ, USA | 09-25 | Cleaning Spray |
Odniesienia
- Buxton, R. B. The physics of functional magnetic resonance imaging (fMRI). Reports on Progress in Physics. 76 (9), 096601 (2013).
- Lohmann, H., Dräger, B., Müller-Ehrenberg, S., Deppe, M., Knecht, S. Language lateralization in young children assessed by functional transcranial Doppler sonography. NeuroImage. 24 (3), 780-790 (2005).
- Knecht, S., et al. Noninvasive determination of language lateralization by functional transcranial Doppler sonography: a comparison with the Wada test. Stroke. 29 (1), 82-86 (1998).
- Knecht, S., et al. Successive activation of both cerebral hemispheres during cued word generation. Neuroreport. 7 (3), 820-824 (1996).
- Hage, B., Way, E., Barlow, S. M., Bashford, G. R. Real-time cerebral hemodynamic response to tactile somatosensory stimulation. Journal of Neuroimaging. 28 (6), 615-620 (2018).
- Hage, B., et al. Functional transcranial Doppler ultrasound for measurement of hemispheric lateralization during visual memory and visual search cognitive tasks. IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control. 63 (12), 2001-2007 (2016).
- Meyer, G. F., Spray, A., Fairlie, J. E., Uomini, N. T. Inferring common cognitive mechanisms from brain blood-flow lateralization data: a new methodology for fTCD analysis. Frontiers in Psychology. 5, 552 (2014).
- Uomini, N. T., Meyer, G. F. Shared brain lateralization patterns in language and Acheulean stone tool production: a functional transcranial Doppler ultrasound study. PLoS ONE. 8 (8), 72693 (2013).
- Edvinsson, L., MacKenzie, E. T., McCulloch, J. . Cerebral Blood Flow and Metabolism. , (1993).
- Alexandrov, A. V., et al. Practice standards for transcranial Doppler ultrasound: part I--test performance. Journal of Neuroimaging. 17 (1), 11-18 (2007).
- Fujioka, K. A., Douville, C. M., Newell, D. W., Aaslid, R. Anatomy and freehand examination techniques. Transcranial Doppler. , (1992).
- Alexandrov, A. V. Transcranial Doppler physics and techniques, lecture notes. American Society of Neuroimaging Conference. , (2020).
- Alwatban, M., Truemper, E. J., Al-rethaia, A., Murman, D. L., Bashford, G. R. The breath-hold acceleration index: a new method to evaluate cerebrovascular reactivity using transcranial Doppler. Journal of Neuroimaging. 28 (4), 429-435 (2018).
- Tiecks, F. P., et al. Effects of the Valsalva maneuver on cerebral circulation in healthy adults: a transcranial Doppler study. Stroke. 26 (8), 1386-1392 (1995).
- Alwatban, M., Murman, D. L., Bashford, G. Cerebrovascular reactivity impairment in preclinical Alzheimer's disease. Journal of Neuroimaging. 29 (4), 493-498 (2019).
- Twedt, M. H., et al. Most high-intensity transient signals are not associated with specific surgical maneuvers. World Journal for Pediatric and Congenital Heart Surgery. 11 (4), 401-408 (2020).
- Moehring, M. A., Spencer, M. P. Power M-mode Doppler (PMD) for observing cerebral blood flow and tracking emboli. Ultrasound in Medicine & Biology. 28 (1), 49-57 (2002).
- Poldrack, R. A. The future of fMRI in cognitive neuroscience. NeuroImage. 62 (2), 1216-1220 (2012).
- Oh, H., Custead, R., Wang, Y., Barlow, S. Neural encoding of saltatory pneumotactile velocity in human glabrous hand. PLoS ONE. 12 (8), 0183532 (2017).
- Rosner, A. O., Barlow, S. M. Hemodynamic changes in cortical sensorimotor systems following hand and orofacial motor tasks and pulsed pneumotactile stimulation. Somatosensory & Motor Research. 33 (3-4), 145-155 (2016).
- Alexandrov, A. V., et al. High rate of complete recanalization and dramatic clinical recovery during tPA infusion when continuously monitored with 2-MHz transcranial doppler monitoring. Stroke. 31 (3), 610-614 (2000).
- Watt, B. P., Burnfield, J. M., Truemper, E. J., Buster, T. W., Bashford, G. R. Monitoring cerebral hemodynamics with transcranial Doppler ultrasound during cognitive and exercise testing in adults following unilateral stroke. 2012 IEEE Engineering in Medicine and Biology Society Annual Conference Proceedings. , 2310-2313 (2012).
- Markus, H. S., Harrison, M. J. Estimation of cerebrovascular reactivity using transcranial Doppler, including the use of breath-holding as the vasodilatory stimulus. Stroke. 23 (5), 668-673 (1992).
- File:Circle of Willis en.svg. . Wikimedia Commons, the free media repository Available from: https://commons.wikimedia.org/w/index.php?title=File:Circle_of_Willis_en.svg (2020)
- Bode, H. . Pediatric Applications of Transcranial Doppler Sonography. , (1988).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone