Фреймворк для исследования перцептивного обучения с симуляцией потери центрального зрения
302 Views
•
07:12 min
•
April 11th, 2025
DOI :
April 11th, 2025
•Транскрипт
Below, we summarize key aspects of implementing a gaze-contingent framework for studying peripheral vision abilities.
1. Identifying an ideal system for simulated central vision loss research
- A first step is to identify a system that efficiently transmits information from the eye tracker to the stimulus generation software, in a continuous loop. We employed methods described in Saunders and Woods37 to measure latency of different combinations of systems, to identify the one with the lowest latency. A comparison of combined latency of four different combinations of systems comprising two eye trackers (EyeLink 1000 Plus Tower Mount and TRACKPixx3), two display devices (CRT Monitor (refresh rate = 100Hz) and Display++ (refresh rate = 120Hz)) along with two operating systems (Windows 10 and Mac iOS) is shown in Figure 3. Each combination was measured 20 times. Results showed that the system with the lowest latency was the Vpixx TrackPixx3 eye tracker in combination with the Windows 10 operating system.

Figure 3. Latency comparison across different combinations of monitors, eye-tracking devices, and operating systems. (E1000: Eyelink 1000; CRT: Cathode-Ray Tube Display ++; Mac: Mac iOS; CRS: ViewSonicPF817; Win: Windows 10; TP: VPixx TrackPixx3). Bars represent the +/-1 standard deviation across the 20 repetitions per combination. Measures were taken with an Apple iPhone 12 in slow motion mode, reaching a refresh rate of 240Hz. TP/CRS/Win is statistically different from E1000/CRT/Mac (t(38)=9.53, p<0.001), E1000/CRS/Mac (t(38)=16.24, p<0.001) and E1000/CRS/Win (t(38)=3.94, p<0.001). Please click here to view a larger version of this figure.
2. Participant familiarization with simulated central vision loss via gaze-contingent display
NOTE: A fundamental component in simulating central vision loss is to familiarize participants with the gaze-contingent display. Without proper familiarization, measures of abilities can be conflated by the participants' effort to navigate the gaze-contingent display. Several key steps in our protocol ensure sufficient familiarization with the gaze-contingent display to be able to measure visual performance reliably. These steps are summarized below:
- Participants are provided with audiovisual instructions about the task that they will be performing during a particular session. Each task has dedicated video instructions with screen captures from the actual task. This is followed by the experimenter explaining the instructions verbally to ensure that the participant has a good understanding of what to expect in a given task.
- Participants are provided with practice trials before beginning each of the main tasks. This provides an opportunity to clarify any questions related to the task.
- During the initial visit, before conducting gaze-contingent tasks, participants undergo fixation training, where they learn to place their simulated scotoma within a white central box on the screen for varying durations with spatial tolerance increasing across trials, while they ignore distractors that may appear on the screen.
- Additionally, participants undergo a 'PRL induction task', which is designed to promote development of PRL-like behavior. In this task, participants view an opaque disk randomly placed on the screen that covers a target (for example a Landolt C) and must move the scotoma close to the opaque disk to reveal the target. Oculomotor analysis of this task can indicate an early PRL-like location that can later be used as a training locus. In our experimental paradigm, the circular central scotoma subtended 10 degrees visual angle.
- These steps allow participants to familiarize themselves with the gaze-contingent display and prepare them to perform a wide range of perceptual assessments and training tasks by using their peripheral vision.
3. Development of effective instructions
NOTE: Instructions play a crucial role in guiding participants on how to respond to stimuli and manage their simulated scotoma during different tasks. Appropriate instructions must be thorough and clear to avoid any confusion. Instructions should be reiterated as needed to ensure understanding. The following methods are recommended to effectively convey task instructions:
- Instructional Videos:
- Visual Demonstration: Videos visually demonstrate each step of the task. Videos should clearly illustrate how to manage the simulated scotoma appropriately during the task, and how to respond to stimuli.
- Narration: A concise script should be developed to accompany the visual demonstration that explains the process in simple terms. Ensure that language is easy to understand and avoid technical terminology.
- Scripted Verbal Instructions:
- Consistency: Use a standardized script for verbal instructions to ensure there is consistency across different sessions and participants.
- Example: "Throughout the task, there will be multiple breaks to rest your eyes. During these breaks make sure to keep your head in the chin-rest. When you are ready to continue the task, press the spacebar and the task will begin again."
- Clarity: Speak slowly and clearly – make sure to emphasize all important aspects of the task.
- Consistency: Use a standardized script for verbal instructions to ensure there is consistency across different sessions and participants.
- Visual Instructions:
- On-screen instructions: Provide written guidance on the screen that participants can read before and during the completion of tasks. Use short sentences for clarity with visual aids to demonstrate stimuli that the participant may encounter during each task.
4. Assessment Tasks' Design and Implementation
NOTE: Tasks designed within this framework are broadly divided into two main categories: (1) Free eye movement tasks and (2) Fixation-constrained tasks. In the free eye movement tasks, participants are allowed to make eye movements across the screen to identify targets appearing at random locations on the screen (or read text) whereas in fixation-constrained tasks participants are required to maintain fixation within a central white box throughout the task and use their periphery to make judgments. Figure 4 shows example tasks and descriptions for each category. More detailed information about the tasks can be found in Supplementary Material and Jayakumar (2024)38.
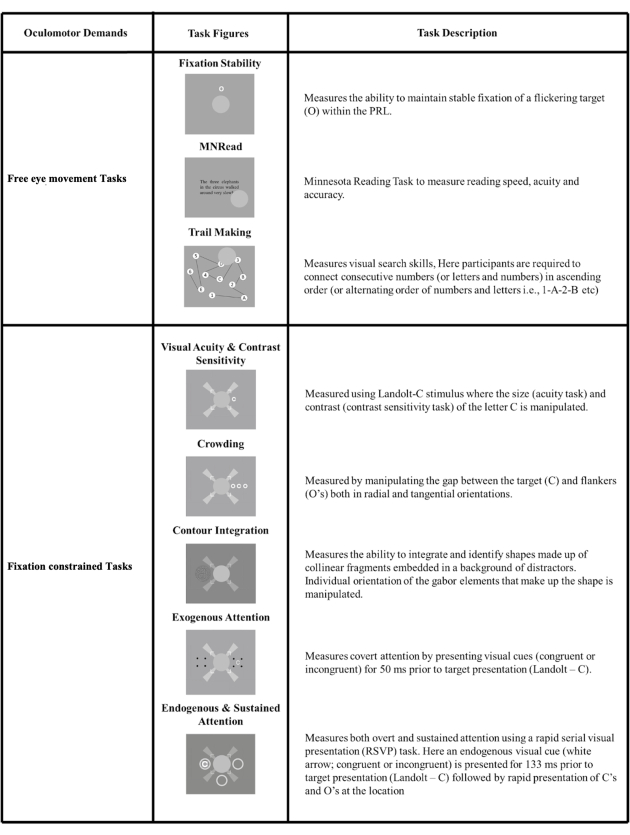
Figure 4. Perceptual Tasks: A visual representation of different assessment tasks designed using our framework. The tasks are broadly categorized into Free eye movement tasks where the scotoma follows the eye movements of the participants to view targets freely (top panel); and Fixation-constrained tasks where the scotoma needs to be placed within a central white box throughout the task (bottom panel). This task has been modified from38. Please click here to view a larger version of this figure.
- Free Eye Movement Tasks
Free eye movement tasks measure participants' eye movement behavior while they perform tasks. These promote understanding of the eye movements in the context of naturalistic tasks such as reading and visual search.
General protocol for free-viewing tasks- Instructional Video/Verbal Instructions
- An instructional video and scripted verbal instructions will be presented to the participant prior to the calibration.
- Calibration
- Validations of previous calibrations are run between tasks and additional calibrations are conducted when validations are poor, or when participants take breaks between tasks.
- Free-Viewing task specific methods
- Free-viewing tasks instruct participants to do a variety of actions using their gaze rather than fixating in one area. Some variants include:
- Bring the scotoma near a cue, causing a stimulus to appear.
- Maintain fixation on a specific screen location for a period of time.
- Perform a standard task, like reading or visual search with central vision occluded by the scotoma.
- At the beginning of tasks, participants are provided with on-screen instructions followed by a set of practice trials. Following the completion of the practice trials, they are given reminder instructions before moving on to the task. It is important the participants understand and have shown proficiency using the visual layouts, the required oculomotor actions, and the response characteristics of each task prior to measuring performance.
- Participants are provided with auditory feedback indicating the accuracy of their responses as they complete each task as visual feedback can be missed due to the use of a scotoma.
- Breaks up to one minute are built into each task to reduce the chance of testing fatigue. Breaks of 3 minutes or longer are built into days that include longer sessions of assessments to reduce the chances of testing fatigue.
- Free-viewing tasks instruct participants to do a variety of actions using their gaze rather than fixating in one area. Some variants include:
- Instructional Video/Verbal Instructions
- Fixation-Constrained Tasks
Fixation-constrained tasks are useful to test, or train, peripheral vision at specific visual field locations. These tasks are suitable for testing both early- and mid-level visual processing, including visual acuity, contrast sensitivity, crowding, etc. as well as high-level visual processing including exogenous and endogenous attention. For these tasks it is important that participants learn to maintain steady fixation, to avoid task performance being confounded by attentional resources dedicated to steady fixation. During these tasks, participants are asked to keep their central vision focused on the center of the screen with the help of fixation aids (Figure 5B) while responding to stimuli that appear in their peripheral vision.
General protocol for fixation-constrained tasks- Instructional Video/Verbal Instructions
- An instructional video and scripted verbal instructions will be presented to the participant prior to the calibration.
- Calibration
- Validations of previous calibrations are run between tasks and additional calibrations are conducted when validations are poor, or when participants take breaks between tasks.
- Fixation-constrained task specific methods
- During fixation constrained tasks, participants are asked to maintain their head position in the chinrest for the duration of the task, ensuring that the calibration remains as accurate as possible to the original position throughout the process.
- Participants are provided with on-screen instructions followed by a set of practice trials. Following the completion of the practice trials, they are given a reminder set of on-screen instructions before moving on to the task.
- During these tasks, participants are asked to keep their central vision focused on the center of the screen with the help of fixation aids (white rectangular fixation box) while responding to stimuli that appear in their peripheral vision to either side of the fixation box.
- Participants respond using their right index finger on a five button response box, located to their right during assessment. If fixation is not maintained, the stimulus will not be presented, and will time out unless fixation is resumed.
- Participants are provided with auditory feedback indicating the accuracy of their responses as they complete each task, as again visual feedback can be missed due to the use of a scotoma.
- Breaks up to one minute are built into each task to reduce the chance of testing fatigue. Breaks of 3 minutes or longer are built into days that include longer sessions of assessments to reduce the chances of testing fatigue.
- Instructional Video/Verbal Instructions
- Development of appropriate fixation displays
Tasks involving peripherally presented targets and simulated scotoma obstructing central vision present challenges when trying to estimate performance in a retinotopically defined location. Indeed, even in foveal tasks, the eyes make small, involuntary movements, in the form of drift and microsaccades). Thus, in order to optimize fixation stability, careful thoughts should go into designing fixation aids. To do so, we developed a fixation aid design that incorporates both a large fixation cross and a fixation box (Figure 5). Participants are instructed to maintain the opaque occluder within the fixation box and use the long arms of the fixation cross as a reference for the center of the screen. This design combines both bullseye- and crosshair- types of visual aids, which have been shown to lead to the best fixation stability38.
Additionally, by having both a fixation box and a fixation cross, this design can be easily used in translational contexts to test patients with central vision loss - Optimization of adaptive procedures to accurately measure performance
A critical aspect of the implementation of different assessments is the ability to quickly and successfully estimate performance thresholds in a subset of these tasks (specifically visual acuity, contrast sensitivity, crowding, and contour integration). A challenge is that traditional staircases can converge slowly and target performance that is close to the threshold might cause frustration and fatigue in participants. To circumvent this, we implemented a three-stage procedure to estimate performance of participants in these tasks. In the first stage, participants perform 12 practice trials before the actual experiment. During the second stage, we utilized a 2-down 1-up staircase that terminated after 3 downward reversals (i.e., direction of stimulus change, from down (hard) to up (easy), also refer to representative results section), followed by the third stage that consisted of a conventional 3-down 1-up staircase that ended after 60 trials. Pilot studies indicated that this procedure achieves reliable thresholds for most tasks (visual acuity, crowding, and contrast sensitivity tasks), however, some tasks can require other methods, especially when performance can differ greatly across participants. For example, in the contour integration task, after the first stage of the procedure (practice) additional procedure was implemented. Difficulty of the task was manipulated using a progressive staircase method where the orientation jitter (0°, 1°, 2°, 4°, 6°, 8°, 10°, 12°) increased every three trials for a total of 24 trials. Then the second and third stages of our procedure (adaptive staircase) continued as normal. In general, different tasks may require slightly different adaptive procedures, however, the 3-stage approach allows participants to practice, and then quickly gets within range of their threshold and provides detailed measurement within that range.
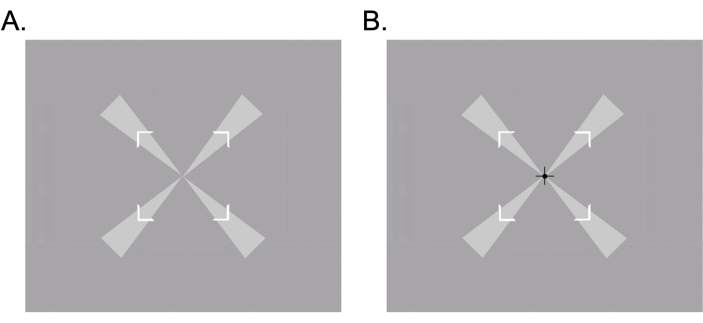
Figure 5. Fixation aids used to promote fixation stability in participants: A. Fixation cross and fixation box that were used for fixation stability tasks, B. Fixation cross, fixation box and black cross at the center that were used in low-level vision tasks. Please click here to view a larger version of this figure.
5. Adapting the framework for testing in MD patients
- While this framework is designed for simulated central vision loss in healthy individuals, it can be extended for research in MD patients, similar to previous gaze-contingent paradigms7,39,40. When adapting this framework for patients, it is important to keep in mind that their viewing strategies drastically differ from that of the sighted individuals. First, it is well known that patients with MD tend to have unstable fixations, thus despite recent attempts at calibrating eye-tracking devices used in vision research in this population41, this might prove challenging. To address this issue, we modified the nine-point calibration and validation process for MD patients by using larger calibration points combined with wedges and reducing the distance between the dots. This adjustment ensures that the targets appear closer to the center of the screen, preventing the need to view targets at extreme eccentricities. Additionally, because many tasks within our framework require stable central fixation, we included extra fixation aids, such as wedges that extend outward from the center of the fixation box to enhance detection. Secondly, it is also important to note that simulated and pathological scotomas differ in several key aspects, including the timeline of their formation, the development of compensatory strategies, and overall fixation stability, which may result in qualitatively different experiences. It is however possible to map the shape and size of the scotoma in MD patients through microperimetry testing and use this to define the shape of the scotoma in our tasks42. Finally, although the metrics we have presented may differ from those typically observed in patients, the ability to dissect eye movement behaviors and characterize the development of oculomotor strategies at various stages of simulated training offers a valuable tool. This approach enhances our understanding of how the visual system adapts to either simulated or pathological central vision loss.
Мы представляем разработку фреймворка для отображения взгляда, предназначенной для перцептивных и глазодвигательных исследований с симуляцией потери центрального зрения. Эта структура особенно пригодна для изучения компенсаторных поведенческих и глазодвигательных стратегий у лиц, испытывающих как симулированную, так и патологическую потерю центрального зрения.
Главы в этом видео
0:00
Introduction
2:03
Participant Familiarization with Gaze-Contingent Displays for Simulated Central Vision Loss
3:26
Design and Implementation of Assessment Tasks for Simulated Central Vision Loss Studies
Похожие видео

Соотнося поведенческих реакций на МРТ Сигналы от человека префронтальной коры: Изучение когнитивных процессов с помощью Task Analysis
12.7K Views

Создание объектов и объектов категории по изучению восприятия и восприятия обучения
11.8K Views

Высокое разрешение функциональной магнитно-резонансной томографии методы по правам мозга
12.8K Views

Оптическая запись запороговой нейронной активности с одноклеточных и одного всплеска резолюции
11.8K Views

В естественных условиях Optogenetic возбуждение нервной системы грызунов Центральной
59.2K Views

Простой Поведенческая Анализ для тестирования зрительной функции в
9.8K Views

Vibratome секционирования мыши Retina Подготовка фоторецептора культур
17.7K Views

Высокое разрешение Структурная магнитно-резонансная томография в подкорке человека
15.3K Views

Обогащение мембраны Бруха от глаз человека доноров
12.0K Views

Измерение Связь в первичной зрительной Путь в человека Альбинизм Использование Diffusion Tensor визуализации и трактография
12.2K Views
Авторские права © 2025 MyJoVE Corporation. Все права защищены