A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Creating Rigidly Stabilized Fractures for Assessing Intramembranous Ossification, Distraction Osteogenesis, or Healing of Critical Sized Defects
In This Article
Summary
This article describes a method for stabilizing long bone fractures that is based on the application of modified Ilizarov external fixators 1-3. After application of the fixators and creation of the bone injury, healing can be assessed, distraction osteogenesis can be performed, or non-union or critical sized defect can be created and used to study therapeutic interventions.
Abstract
Assessing modes of skeletal repair is essential for developing therapies to be used clinically to treat fractures. Mechanical stability plays a large role in healing of bone injuries. In the worst-case scenario mechanical instability can lead to delayed or non-union in humans. However, motion can also stimulate the healing process. In fractures that have motion cartilage forms to stabilize the fracture bone ends, and this cartilage is gradually replaced by bone through recapitulation of the developmental process of endochondral ossification. In contrast, if a bone fracture is rigidly stabilized bone forms directly via intramembranous ossification. Clinically, both endochondral and intramembranous ossification occur simultaneously. To effectively replicate this process investigators insert a pin into the medullary canal of the fractured bone as described by Bonnarens4. This experimental method provides excellent lateral stability while allowing rotational instability to persist. However, our understanding of the mechanisms that regulate these two distinct processes can also be enhanced by experimentally isolating each of these processes. We have developed a stabilization protocol that provides rotational and lateral stabilization. In this model, intramembranous ossification is the only mode of healing that is observed, and healing parameters can be compared among different strains of genetically modified mice 5-7, after application of bioactive molecules 8,9, after altering physiological parameters of healing 10, after modifying the amount or time of stabilization 11, after distraction osteogenesis 12, after creation of a non-union 13, or after creation of a critical sized defect. Here, we illustrate how to apply the modified Ilizarov fixators for studying tibial fracture healing and distraction osteogenesis in mice.
Protocol
All Procedures were approved by the UCSF Institutional Animal Care and Use Committee and conform to national guidelines.
1. Preparation of Fixators Prior to Surgery
- Before creating stabilized fracture, one needs to assemble the custom-design external fixation device. The custom-designed external fixation frames consisted of two aluminum rings stabilized by three stainless-steel #0/56 threaded rods, 8 #2/56 hexagonal nuts, and 17 matching bolts (Small Part Inc., Miami Lakes, FL3).
- Two aluminum rings are needed per fracture. To one ring assemble 4 #2/56 hexagonal nuts (small Part Inc., Miami Lakes, FL) and matching bolts into the appropriate holes, these should remain loose. This will be the proximal ring. To the distal ring assemble 3 nuts and bolts, again do not tighten fully.
2. Anesthesia, Fracture Creation, and Fixator Application
- Mice (age, sex, and body weight are determined by the user) are anesthetized by intraperitoneal injection of 50mg/ml Ketamine, 0.5 mg/ml Medetomidine (0.03 ml/mouse).
- Apply eye lubricant to the eyes of the mice and place a piece of tape across their head to protect their eyes during the procedure.
- The animal is placed on a heating pad for the remainder of the procedure.
- Transfix the proximal and distal metaphyses of the left tibia using four 0.25 mm sterile insect pins (Anticorro: Fine Science Tool, Foster City, CA) by attaching the pins to a Dremel Tool and drilling them through the bone.
- Pins are oriented perpendicular to the long axis of the tibia, and 90 ° to each other. At least 10 mm between the proximal and distal pins.
- Position the first ring above the proximal pins with the nuts facing inward, toward the pins. Secure the pins to the ring keeping the tibia positioned centrally within the aluminum ring.
- Position the second ring below the distal pins and secure the pins to the ring using the hexagonal nuts as before. Add the fourth nut-bolt combination to the distal fixator.
- Create the transverse fracture by three-point bending with an appropriate device. We use the gravity system of Bonnarens and Einhorn 4. Rest the posterolateral surface of the tibia across the blocks, raise the weight to a predetermined height along the drop arm and drop the weight so that it contacts the anterolateral aspect of the tibia to produce the blunt fracture. The height the weight is dropped from needs to be determined for each strain of mouse to ensure a single fracture exclusively of the tibia.
- Fracture is confirmed by X-ray.
- After confirming the fracture, three stainless steel #0/56 threaded rods are attached to the rings. Starting from the distal end insert the rod and thread a nut onto the distal ring to secure the rod. Then put another nut onto the rod, the proximal ring will sit on top of this nut. Ensure that the two rings will be held at equal distances and are not straining the pins. Secure the proximal ring to the rods with a third nut.
- Subcutaneous injections of buprenorphine (1.0 mg/kg) for analgesia are given immediately after surgery and animals are monitored for pain and given buprenorphine as needed.
- Anesthesia is reversed by administering Atipamezole, and animals are monitored until they are responsive and ambulating.
3. Distraction Osteogenesis (see also: 12,13)
To modify this procedure to accommodate distraction osteogenesis is straightforward. The rings are held in position by threaded rods, and by turning the nuts holding the rods in place the rings can be moved apart.
- Latency: For standard distraction osteogenesis using this model the fixators are placed onto the tibia and left alone for a latency period of 5 days.
- Distraction: Distraction osteogenesis can be performed by turning the nuts on the stabilizing rods ¼ turn (0.25 mm) every day 7 days.
- Maturation: Bony bridging is observed by 10 days and complete consolidation is observed by 27 days after the completion of distraction.
4. Creation of a Critical Sized Defect
To create a critical sized defect the external fixators are applied as previously described with the following modifications.
- Before beginning the procedure the skin is cleaned with 70 % ethanol.
- The fixators are applied completely prior to creating the defect.
- The mouse is then place under the dissecting microscope to visualize the medial tibia, and an incision (5-7 mm) is made with a #10 blade on a scalpel.
- The muscle is gently transected and separated to expose the mid-diaphysis of the tibia.
- A 3 mm segment of the bone is then removed from the mid-diaphysis using scissors. Using the point of the scissors, the bone is slowly snipped away and bone fragments are removed with forceps if necessary. Care should be taken with the tips of the scissors to avoid displacing the tibia with a large mechanical force.
- Examine the surgical site to ensure that there are no bone fragments, as these could promote healing.
- Replace the muscle around the blunted ends of the tibia.
- Close the incision on the skin with 2-3 sutures of 6-0 Polyamine Monofilament.
- Anesthesia is reversed and the animals are monitored for pain and given analgesics as previously described.
5. Representative Results
When properly applied, the external fixators provide more rigid stability of the closed tibial fracture with excellent reduction (Figs. 1, 2). However, in some cases inadequate reduction (an obvious and large gap between bone ends or multiple fractures occur (Fig. 3), and these mice are excluded from analyses. Fractures stabilized using this method heal primarily via intramembranous ossification (Fig. 4). In contrast, if the fracture is not stabilized a large cartilage callus is formed in the fracture gap (Fig. 5), and this is replaced by bone through the process of intramembranous ossification.
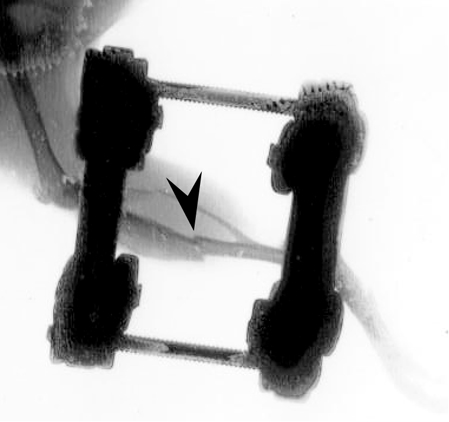
Figure 1. Radiographs illustrating an external fixation device used to stabilize tibial fracture. Radiograph taken after fracture showing a well-aligned bone segments (arrowhead).

Figure 2. Image of a mouse after the fixator has been applied.

Figure 3. Radiograph taken after fracture shows misaligned and fragmented bone segments (arrowhead).

Figure 4. Stabilized fracture heals via intramembranous ossification. Trichrome staining of stabilized fracture shows some new bone (b) at fracture site. Scale bar = 500 μm.

Figure 5. Non-stabilized fracture heals via endochondral ossification. Trichrome staining of non-stabilized fracture shows cartilage (c) and bone (b) at fracture site. Scale bar = 500 μm.
Discussion
Bones heal by two different modalities depending on mechanical stability (reviewed in: 14). When left unstable a large cartilage template forms in the fracture gap that is replaced by bone to bridge the two ends of broken bone. Proximally and distally to the break, bone forms directly by intramembranous ossification within the periosteum and endosteum. In contrast, in stable fractures healing occurs exclusively via intramembranous ossification 3. However, the specific mechanisms that regulate the sw...
Disclosures
We have nothing to disclose.
Acknowledgements
This work was funded by R01-AR053645 from NIAMS.
Materials
| Name | Company | Catalog Number | Comments |
| 0.25mm insect pin | Fine Science Tools | 26000-25 | Blacked Anodized Steel, 0.25mm rod diameter, 4cm length |
| Stainless Steel Hex Nut | Small Parts, Inc. | #2-56 | 1/8" length, 56 threads per inch |
| Stainless Steel Hex Nut | Small Parts, Inc. | #0-80 | 1/8" length, 80 threads per inch |
| Stainless Steel Machine Screw | Small Parts, Inc. | #0-80 | 1/8" length, 80 threads per inch |
| Stainless Steel Machine Cut Threaded Rod | Small Parts, Inc. | #0-80 | 6" length, 80 threads per inch |
| 18-8 Stainless Steel Head Machine Screw | McMaster-Carr | 2-56 Threads, 3/6" length | |
| External Fixation Device | Machine shop | Custom-designed |
References
- Ilizarov, G. A., Lediaev, V. I., Shitin, V. P. The course of compact bone reparative regeneration in distraction osteosynthesis under different conditions of bone fragment fixation (experimental study). Eksperimentalnaia Khirurgiia i Anesteziologiia. 14, 3-12 (1969).
- Ilizarov, G. A., Deviatov, A. A. Surgical elongation of the leg. Ortopediia Travmatologiia i Protezirovanie. 32, (1971).
- Thompson, Z., Miclau, T., Hu, D., Helms, J. A. A model for intramembranous ossification during fracture healing. J. Orthop. Res. 20, 1091-1098 (2002).
- Bonnarens, F., Einhorn, T. A. Production of a standard closed fracture in laboratory animal. J. Orthop. Res. 2, 97-101 (1984).
- Colnot, C., Thompson, Z., Miclau, T., Werb, Z., Helms, J. A. Altered fracture repair in the absence of MMP9. Development. 130, 4123-4133 (2003).
- Lange, J. Action of IL-1beta during fracture healing. J. Orthop. Res. 28, 778-784 (2010).
- Xing, Z. Multiple roles for CCR2 during fracture healing. Dis. Model Mech. 3, 451-458 (2010).
- Lu, C. Recombinant human bone morphogenetic protein-7 enhances fracture healing in an ischemic environment. J. Orthop. Res. , (2009).
- Yu, Y. Y., Lieu, S., Lu, C., Colnot, C. Bone morphogenetic protein 2 stimulates endochondral ossification by regulating periosteal cell fate during bone repair. Bone. 47, 65-73 (2010).
- Lu, C., Miclau, T., Hu, D., Marcucio, R. S. Ischemia leads to delayed union during fracture healing: a mouse model. J. Orthop. Res. 25, 51-61 (2007).
- Miclau, T. Effects of delayed stabilization on fracture healing. J. Orthop. Res. 25, 1552-1558 (2007).
- Tay, B. K., Le, A. X., Gould, S. E., Helms, J. A. Histochemical and molecular analyses of distraction osteogenesis in a mouse model. Journal of Orthopaedic Research. 16, 636-642 (1998).
- Choi, P., Ogilvie, C., Thompson, Z., Miclau, T., Helms, J. A. Cellular and molecular characterization of a murine non-union model. J. Orthop. Res. 22, 1100-1107 (2004).
- Buckwalter, J. A., Marsh, E. T., J, L., Heckman, J. D., Bucholz, R. W. . Rockwood and Green's fractures in adults. , 245-271 (2001).
- Garcia, P. The LockingMouseNail-A New Implant for Standardized Stable Osteosynthesis in Mice. J. Surg. Res. , (2009).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved