Method Article
Testing of all Six Semicircular Canals with Video Head Impulse Test Systems
In This Article
Erratum Notice
Summary
This protocol describes how to correctly perform the video head impulse test with two separate test systems commonly used worldwide. Both the 2D and 3D video head impulse test methods are described.
Abstract
Throughout the last decade, there has been a rapid development of existing test procedures and methods evaluating the human vestibular system. In 2009 and 2013, commercially available video Head Impulse Testing (vHIT) has enabled clinicians to examine the function of all three paired semicircular canals within the vestibular system. The vHIT test has revolutionized vestibular testing and, at many clinics and hospitals around the world, this test is now considered the most important initial test of vertiginous patients. There are several manufacturers of vHIT systems around the world. A test protocol for two of the most widespread vHIT systems, EyeSeeCam and ICS Impulse, will be presented. Included in this protocol is a description of the two different test methods termed 2D vHIT testing and 3D vHIT testing. The vHIT system includes a lightweight goggle with accompanying software. The test is fast (5-10 min) and can be done with minimal discomfort to the person being examined. However, there are many steps of the test, and each of these steps may alter the final test results, if the individual steps of the test are not performed correctly. It is therefore of paramount importance that the examiner is familiar with the potential noise and/or artifact triggers. Systematic training of future examiners before performing vHIT in a clinical setting and compliance with this protocol may minimize these challenges of the test. The vHIT test is not just a “plug and play” test. However, if carried out correctly, this test offers excellent objective assessment of the function of the high frequency domain of the vestibular system. It has a very high positive predictive value and offers a specificity very close to one hundred percent.
Introduction
Vertigo is the third most common complaint among patients seeking general medical advice and has a lifetime prevalence of 7.8 percent1,2. It is often difficult to determine whether the cause of vertigo is due to disease within the vestibular organs or disease in other parts of the body, because vertigo may be the presenting symptom of numerous diseases3. Traditionally, vestibular testing has been difficult and time-consuming for the clinician and often not very pleasant for the participant. Many of these tests have been done as bedside examinations that rely upon a very skilled examiner and cooperative, dizzy patient. A well-recognized method for bedside testing of vestibular function was introduced in 1988 and termed the "head impulse test"4. Throughout the last decade, there has been rapid development of existing test procedures and methods as well as a rise in new methods of testing. Various laboratory tests, which evaluate the function of the vestibular system, are now commercially available. In 2009, a new test method, video head impulse testing (vHIT), became commercially available. With this test, clinicians around the world are now able to test functioning of the six semicircular canals (SCCs) of the vestibular system objectively and quickly (5-10 min), with only minor discomfort to the patient5. The vHIT test has revolutionized vestibular testing, and in many clinics and hospitals around the world, it is now considered the most important initial test for both acute and chronic vertiginous patients6.
There are several manufacturers of vHIT systems around the world. Some of the most widespread vHIT systems include the EyeSeeCam (Denmark), ICS Impulse (Denmark), and VHIT Ulmer (France) (see Table of Materials). The first two mentioned vHIT systems are quite similar in design and further described in this article (and referred to as vHIT systems A and B, respectively). Both these vHIT systems provide a lightweight goggle that contains a high-speed camera for the recording of eye movements and a sensor that measures head velocity7. Accompanying software needs to be installed on a laptop computer, and the goggle is connected via a USB cable connection to the same computer. During vHIT testing, the goggles are mounted on the patient’s head and attached firmly. Participants keep their eyes fixed on a target on the wall while the examiner applies fast, abrupt, and unpredictable head impulses in the plane of the semicircular canal being tested. The vHIT provides the examiner with a report that includes 1) a graph depicting head and eye velocity as a function of time and 2) a calculated numeric value termed the "mean gain value".
After completion of the vHIT test, the software calculates the mean gain value, which is defined as the eye velocity in °/s divided by the head velocity in °/s for each of the SCCs being tested. Individual vHIT systems assess the function of the SCCs by means of testing the vestibular-ocular reflex (VOR), but they often calculate the mean gain value by various methods. The vHIT system A uses the regression gain method, which allows for graphical data analysis over the entire velocity range of head impulses. Following vHIT test completion, it provides the average regression plot slope (a best-fit line through data points at different head velocities with accompanying gain values). The vHIT system B uses the area-under-the-curve (AUC) method for calculation of gain values. The area under the eye velocity record is divided by the area under the head velocity record. This area VOR gain is less affected by minor deviations in eye velocity, which may affect VOR gain calculated from only eye velocity records7. When using the AUC method, the gain value is calculated as the ratio of cumulative slow-phase eye velocity over cumulative head velocity from the onset of the head impulse to the moment at which head velocity returns to zero.
Additionally, unlike the bedside head impulse test, vHIT enables the examiner to detect compensatory eye movements and saccades [both occurring after head movement has stopped (overt saccades) and saccades occurring during the head movement (covert saccades)] by analyzing the graphs provided in the accompanying report8,9. Conclusions on whether or not pathological saccades are present require subjective assessment of the test report, as no consensus exists on the definition of pathological saccades. However, if the software with ICS impulse identifies saccades as pathological, these curves are marked as red. Eye recordings are analyzed differently by the two vHIT systems. In system B, the center of mass of the pupil is determined and used, along with the timestamps from the images, to determine the eye velocities. These are used along with the head velocities for the gain calculations. In system A, lateral and vertical eye movement velocities are analyzed. If only the pupil is analyzed, only the horizontal and vertical components of eye-in-head position enter a vector analysis algorithm that calculates the VOR gain.
The vHIT test is considered an objective test. This test, however, is technically demanding for the examiner to perform. Head impulses, applied to the participant, need to be unpredictable in both timing and direction, and they need to be delivered at peak head velocities between 150° and 250° per second with an amplitude of 5° to 20°, ideally8,9,10,11. Another prerequisite for successful testing is that the participant is able to understand and comply with the given instructions8. The test is also susceptible to several sources of error, with the most common being goggle slippage8,11,12 and noise/artifacts due to poor pupil detecting and tracking8. The company software discards impulses with too much noise/artifacts during testing. Upon completion of the test, it is often necessary to manually remove additional noise and/or artifacts that the software did not detect and remove automatically.
Both vHIT systems use the same test method for horizontal vHIT testing. Vertical SCC testing is, however, more difficult to perform than horizontal SCC testing. With testing of the vertical SCCs, head impulses are more technical demanding to deliver, the eye movements include a torsional component, the test is more susceptible to goggle slippage, and the test is more uncomfortable for the participant11. The traditional method used for vHIT testing is termed "3D vHIT testing" and is used when performing vertical SCC testing with the vHIT system A. In response to these challenges, a 2D modified vHIT test method has been developed13. This method, which provides near total removal of the rotational part of the eye movements during testing, is used when performing vertical SCC testing with the vHIT system B. Illustrations and a more detailed description of these two vHIT test methods are provided in the results section. A recent study included both of the abovementioned vHIT systems14. Because these vHIT systems use separate test methods for vertical SCC testing, both the 2D and 3D vHIT test methods were used in the evaluation of vestibular function. The name of the 3D test method may be misleading, as most commercially available vHIT test systems currently measure eye movements in only two dimensions. However, the original test is referred to as the 3D test method throughout this article. The abovementioned two vHIT test methods are described in detail. It should also be noted that 2D vHIT testing is possible with the vHIT system A, but to the best of our knowledge, this test method has not yet been validated for this vHIT system.
Protocol
This protocol follows the guidelines of the scientific Ethics Committee of the North Denmark Region.
1. Participant Screening
- Recruit participants that are capable of completing the test. Participants must have vision capabilities that allow for fixation on a dot at a distance of 1.0 to 1.5 m away.
- Disqualify participants with a history of neck surgery or cervical herniation, because the head impulses applied might worsen such conditions. Remove any makeup, as this might cause poor tracking of the pupil.
- Assess the eye movements of the participant by performing a gross eye movement examination to rule out any eye muscle palsies that might affect the examination. Also note if there is any spontaneous or gaze-induced nystagmus that may affect the final results.
- Perform a gross eye movement examination by requiring participants to move their eyes in the vertical and horizontal planes to the outer edge of the eye sockets to ensure no eye muscle palsies are present.
- Evaluate sizes of the pupils in a well-lit room and note the configuration of the pupils. This ensures that the tracking of the pupils is not compromised during testing.
- Determine if both eyes are equally suited for the recording of eye movements.
NOTE: Not all vHIT systems have the option of recording either left or right eye movements.- Decide which eye is optimal for recording eye movements (if they are not equally good) following examination of the participants eye movements and visual acuity.
- Take special notice of the area surrounding the eyes and use proper precautions if the participant has one or two droopy eyelids. Evaluate and note if eyelashes are very long and could compromise tracking of the pupils during the test.
- Use either vHIT system A or B for the test, if the right eye is suitable for testing. If only the left eye is suitable for testing, then use system A for the vHIT test.
2. Preparation for the Experiment
- Include recommended hardware and software to enable video head impulse testing. Make sure to read the manual before installment.
- The hardware requirements consist of a laptop PC and pair of accompanying lightweight goggles containing a high-speed camera and motion sensor. Use an inertial motion sensor with vHIT system A and head velocity sensor chip (MEMs gyroscope) with system B. The motion sensors provide information about the head velocity. Check that the individual hardware components are intact.
- Install the appertaining software for each system.
- Seat the participant in a non-rotating solid chair at least 1.5 m away for vHIT system A or at least 1.0 m away (vHIT system B) from a fixation dot placed on a wall. Adjust the height of the chair so that the eyes of the participant are leveled with the fixation dot; alternatively, place dots at different heights to achieve the same effect.
- Make sure the room is well-lit to minimize the size of the pupils. Instruct the patient thoroughly regarding the different steps of the test.
- Ask participants not to move their heads during the test by relaxing their neck muscles. To optimize the test, all head movements must be applied by the examiner.
- Ask the participant to avoid blinking with the eyes during the head impulse. If needed, offer a pause between individual head impulses to overcome this problem. During the test, participants should maintain fixation on a dot on the wall.
3. Conditions and Experimental Design
- Fit and adjust the goggles on the patient’s head. It must be tightly fixed (this is crucial).
- Tighten the strap firmly to ensure that goggles will not shift during application of head impulses. Place the cable from the goggles at the midline of the neck and attach it to the cable strap holder (vHIT system A) or with the accompanying cable clip to the patient’s clothing (vHIT system B).
- Ensure that the eyes are wide open, with eyelids in a position where they do not interfere with pupil detection. If required, adjust the skin around the eyelid accordingly.
- Tilt either the bottom or top of the goggles out and away from the face, pull the skin up or down, and reposition the goggles to hold the skin in place. Visually inspect to see if the goggle fit is satisfactory.
NOTE: The goggle fit is an extremely important procedure. Improper goggle fit may result in inaccurate data collection with addition of noise to the test.
- Tilt either the bottom or top of the goggles out and away from the face, pull the skin up or down, and reposition the goggles to hold the skin in place. Visually inspect to see if the goggle fit is satisfactory.
- Align the camera to center the pupil in the image by rotating the camera in the yaw, pitch, or roll direction. Place the boundary of the lower eyelid along the bottom edge of the image (vHIT system A).
- With vHIT system B, position the ROI (region of interest) around the pupil and select auto threshold on the laptop.
- Assess the tracking of the pupil by making short horizontal and vertical head movements prior to initiation of the test. Make sure that the entire pupil is visible in all positions. Adjust manually if necessary.
- Check if the reflections from the LED (two white dots) appear to be close to the edge of the pupil. If this is the case, move the patients head forward in the pitch plane to increase the distance between the two reflections and pupil (system A and B).
- Ask the participant to look straight ahead at the leveled fixation dot. If the center laser projection does not match the fixation dot on the wall, readjust the laser that is mounted on the part of the goggle that sits above the rim of the nose (system A).
4. Calibration
- For vHIT system A, initiate standard calibration (steps 4.1.1-4.1.2) prior to testing of the lateral SCCs with the appertaining software. Immediately following this procedure, initiate head calibration (step 4.1.3) if vertical SCC testing is intended.
- Double-click the software icon on the desktop, which will open the program. Select the instrument by double-clicking on the EyeSeeCam icon in the Select Instrument Box.
- Select Standard in the Calibration menu and click on Prepare.
- Tell the participant to look at the middle laser dot. Inform the participant not to blink and instruct the participant to look at each of the designated laser dots for approximately 2-3 s (one at a time) without moving the head.
- Follow the instructions on the screen or decide the order in which the patient must look at the dots. It is important that participants direct their eyes to each of the five dots once, preferably twice.
- Make sure the standard calibration meets the required criteria. A good calibration is visualized in the calibration report as a cross in which each arm is equally long (see Figure 1).
- Make sure there are five highlighted circles illustrating one center point and the four outer markings (Eye in Image). Also make sure the arms of the cross are located in zero degrees both vertically and horizontally (Eye in Space).
- Perform the head calibration to include vertical SCC testing. Select Head in the Calibration menu, then click on Prepare.
- Ensure that the amplitude of the head movements (peak head velocity) is around 50°/s. Amplitude must not exceed 100°/s (the edge of the circle markings).
- Rotate the patients head back and forth (along pitch axis) at least 5x followed by side-to-side rotations (along the yaw axis) at least 5x. The motion is depicted on the screen.
- Make sure the amplitude of the head movements is around 50°/s. Be careful that it does not exceed 100°/s (the edge of the circle markings).
- Evaluate the quality of the calibration. Learn the characteristics of a good head calibration.
- Make sure the markings do not exceed the edge of the circle. Also ensure that markings are in close proximity to the vertical and horizontal lines.
- Make sure a third image is shaped like a cross where the legs do not deviate more than one triangle vertically and horizontally (see Figure 2).
- Use the default settings if the patient cannot fully cooperate during the calibration. Try recalibrating at least 2x before choosing this option.
- Double-click the software icon on the desktop, which will open the program. Select the instrument by double-clicking on the EyeSeeCam icon in the Select Instrument Box.
- For vHIT system B, follow these steps of calibration to enable testing of all six SCCS. Make sure the ROI embeds the entire pupil area.
- Turn the lasers on. Ask the participant to move the head to position the left and right laser dots on each side of the fixation dot equidistantly (see Figure 3).
- Tell the participant to keep their head in that position. Ask the participant to follow the visible laser beam dot by moving their eyes only (during calibration, only one laser dot is visible alternating between the left and right side).
- Check the calibration by having participants stare at the fixation dot. Move their heads side-to-side about 10°.
- Check that eye and head velocities match. Keep in mind that catch-up saccades seen during low frequency head rotations can indicate either vestibular loss, cerebellar dysfunction, or both.
5. Procedure
- General test principles:
- Deliver head impulses unpredictably. This is required both in regard to direction and timing.
- Deliver abrupt head impulses. Apply head impulses with a small amplitude (5°-20°).
- Perform high acceleration head impulses (1,000°/s2-4,000°/s2). Make sure that the head impulses are fast.
- Deliver head impulses with peak head velocities between 150°/s-250°/s for horizontal SCC testing and deliver head impulses with peak head velocities between 100°/s-250°/s for vertical SCC testing.
- Deliver head impulses with an amplitude of 5°-20°. After completion of each head impulse, the software will provide feedback on quality of the head impulses.
NOTE: With vHIT system A, head impulses are accepted if peak head velocity is reached within the first 70 ms after onset of the head impulse and if the peak head velocity exceeds 150°/s (lower limit may be changed according to personal preferences). Note that this is shown visually by a green check mark or alternatively with a red cross indicating that the given head impulse did not meet the predefined criteria. With vHIT system B, data is collected in real-time during the actual testing. Head impulses will be accepted if the predefined data algorithm criteria are met. These include a head movement with a peak head velocity of minimum of 120°/s to 250°/s for testing of the lateral SCCs and a head movement with peak head velocity of minimum of 100°/s to 250°/s for testing of the vertical SCCs. Head impulses will also be rejected if the frame rate drops below 219 frames/s. Following each head impulse, operator feedback is also displayed for the current impulse. A green circle indicates that the head impulse was accepted (performed adequately), and an orange dot indicates that the head impulse was rejected (not performed adequately).
- To perform horizontal SCC testing, place hands on the jaw or on top of the head. Be careful not to touch the goggle strap or cable to avoid any unintentional movement of the goggles.
- Ask participants to clench their teeth during testing to reduce jaw movement and facilitate a more direct force transfer to the head if testing is done with hands placed on the jaws.
- Turn the patients head 30° forward in the pitch plane to position the horizontal SCCs completely horizontal. Deliver between 10 to 20 head impulses to each side. Note that the software keeps track of the total number of impulses applied to each SCC.
- To perform vertical SCC testing, place the dominant hand on top of the patient’s head and direct the fingers in the direction of the anterior SCC to be tested. Place the non-dominant hand on the chin.
- Ask participants to clench their teeth (the patient may bite on a wooden tongue depressor). Be careful not to touch the goggle strap or cable to avoid unintentional movement of the goggles (thumbs can be positioned on the mastoid and other fingers on the mandible).
- Two different methods for testing of the VOR function of the vertical SCCs exist. Evaluate the vertical SCC function using either the 2D (step 5.3.3) or 3D vHIT (step 5.3.4) test method (see Figure 4).
- Use the 2D vHIT test method for examination with vHIT system B. Rotate the chair 45° to either side, and before vertical SCC testing, place the table legs on fixed markings on the floor to ensure exact alignment of the starting position with every consecutive test. This will also assure a minimum distance of 1 m between the participant’s test eye and fixation point on the wall.
- Right anterior (RA) and left posterior (LP) SCC: turn the solid chair 45° to the left. Ask the patient to look at the fixation dot. The eye that is being measured is now lateralized.
- Right anterior (RA): rotate the participants head forwards in the pitch plane perpendicular to the wall. Be careful not to touch the cable or the goggle strap.
- Left posterior (LP): rotate the participants head backwards in the pitch plane perpendicular to the wall. Be careful not to touch the cable or the goggle strap.
- Left anterior (LA) and right posterior (RP) SCC: turn the solid chair 45° to the right. Ask the patient to look at the fixation dot. The eye that is being measured is now medialized.
- Left anterior (LA): rotate the participants head forwards in the pitch plane perpendicular to the wall. Be careful not to touch the cable or the goggle strap.
- Right posterior (RP): rotate the participant’s head backwards in the pitch plane perpendicular to the wall. Be careful not to touch the cable or the goggle strap.
- Right anterior (RA) and left posterior (LP) SCC: turn the solid chair 45° to the left. Ask the patient to look at the fixation dot. The eye that is being measured is now lateralized.
- Use the 3D vHIT test method for examination with vHIT system A.
- Position the participant in front of the wall at the desired distance. Ask the patient to remain in this position throughout the entire test.
- Use the direction/plane guide in the upper right corner for visualization of the plane of the head rotations during vertical SCC testing. If the test is done correctly, the direction must be depicted within the colored areas where the direction is shown in grey and the latest vertical head impulse in black.
- Right anterior (RA) SCC: rotate the head forwards and 45° to the right of the sagittal plane. Left posterior (LP) SCC: rotate the head backwards and 45° to the left of the sagittal plane.
- Left anterior (LA) SCC: rotate the head forwards and 45° to the left of the sagittal plane. Right posterior (RP) SCC: rotate the head backwards and 45° to the right of the sagittal plane.
- Be careful not to touch the cable or goggle strap, as it may add noise to the test.
6. Interpretation of Results
- During testing, both vHIT systems disregard datasets that do not meet certain predefined criteria. Adjust the preset head velocity criteria of both vertical and horizontal SCCs with system A manually (optional).
- Note that a final algorithm, incorporated in the company software, automatically removes head impulses than contain artifacts and noise following completion of the vHIT test. If the final test results still contain noise or artifacts, remove artifacts/noise by manual data selection.
- Both vHIT systems allow video recording of the eye movements during testing as an additional means of troubleshooting. Enable this is as needed (optional).
- Manually remove additional noise/artifacts following vHIT system A testing with the appertaining software. Enter the Edit menu.
- Choose Velocity Trace Selection. Select Multiple in the dropdown menu.
- Manually select the curves to be deleted and choose Delete Selected. A new report without the selected curves will then be generated. In case too many curves have been removed by a mistake, selection of Show All will regenerate the original report containing all data initially obtained.
- Manually remove additional noise/artifacts following vHIT system B testing with the appertaining software. Enter the 2D analysis menu.
- Place the cursor at the desired head impulse to highlight the entire graph related to that specific head impulse. Press delete to manually remove this head impulse if graph contains noise and/or artifacts.
- Mean gain values and graphs containing saccades will adjust concomitantly following manual removal of head impulses. Restore the dataset in case of unintended deletion of head impulses.
- Manually remove additional noise/artifacts following vHIT system A testing with the appertaining software. Enter the Edit menu.
- Evaluate and interpret the test report upon completion of the vHIT test. The test report includes a 2D graphic depiction of the head impulse by means of time and head and eye velocities as well as calculation of a mean gain value.
- The mean gain value is calculated by dividing the peek eye velocity (°/s) by peak head velocity (°/s). The normal range for the horizontal SCC gain values are 0.80 to 1.207. Determine if the gain value is either within the normal range, too high, or too low.
- If the mean gain value is between 0.80 and 1.20, conclude that the gain value is normal.
- Perform all steps of the vHIT test again, including a recalibration (perform all steps and substeps included in step 4, and perform all steps and substeps included in step 5 for the relevant vHIT system), if higher than expected mean gain values are obtained (>1.20).
NOTE: High numbers do not truly represent any vestibular pathology but indicate that the test was not carried out correctly or that the participant did not fully cooperate during the test. - If the mean gain value is below 0.80, conclude that the gain value is too low and may represent pathology within the vestibular organ by means of compromised VOR function.
- The normal range for the vertical SCC gain values are 0.70 to 1.207. Determine if the gain value is within the normal range, too high, or too low. If the mean gain value is between 0.70 and 1.20, conclude that the gain value is normal.
- Perform all steps of the vHIT test again, including a recalibration (perform all steps and substeps included in step 4, and perform all steps and substeps included in step 5 for the relevant vHIT system), if higher than expected mean gain values are obtained (>1.20).
NOTE: High numbers do not truly represent any vestibular pathology but indicate that the test was not carried out correctly or that the participant did not fully cooperate during the test.
- Perform all steps of the vHIT test again, including a recalibration (perform all steps and substeps included in step 4, and perform all steps and substeps included in step 5 for the relevant vHIT system), if higher than expected mean gain values are obtained (>1.20).
- If the mean gain value is below 0.70, conclude that the gain value is too low and may represent pathology within the vestibular organ by means of compromised VOR function.
- Evaluate the test report graphs and determine if any saccades are present. Saccades are corrective eye movements and, if pathological, are due to a compromised VOR function.
- Interpret all graphic material and conclude whether or not pathological saccades are present as defined by Abrahamsen et al.13.
- Evaluate the frequency of potential saccades. The saccades must occur in more than 50% of the total number of head impulses.
- Evaluate the latency of potential saccades. The saccades must occur within the interval between 100 ms after the head movement is initiated and within 100 ms after head movement has stopped.
- Evaluate the velocity of potential saccades. The saccades must have a peak head velocity of minimum 50% of the peak head velocity.
- Evaluate the direction of potential saccades. The saccades must be in the same direction as the VOR. If the saccades are depicted in the opposite direction, consider if the findings may be depictions of spontaneous nystagmus instead.
- The mean gain value is calculated by dividing the peek eye velocity (°/s) by peak head velocity (°/s). The normal range for the horizontal SCC gain values are 0.80 to 1.207. Determine if the gain value is either within the normal range, too high, or too low.
7. Conclusion
- Classify the vHIT examination of each separate SCC to be normal, atypical, or pathological based on the mean gain value and the presence/absence of pathological saccades.
- Conclude the individual SCC function to be normal if the mean gain value is within the normal range and no pathological saccades are present.
- Conclude the individual SCC function to be pathological if the mean gain value is below the normal range and pathological saccades are present.
- Conclude the individual SCC function to be potentially compromised/atypical if the mean gain value is below the normal range and no concomitant pathological saccades are present.
- Conclude the individual SCC function to be potentially compromised/atypical if the mean gain value is within the normal range and concomitant pathological saccades are present.
Results
Prerequisites for a valid and precise test result include correct, meticulous, and thorough pretest calibrations. For reports following a correct calibration with the vHIT system A, refer to Figure 1 and Figure 2. Calibration with the system B is done in one step for all six SCCs by asking participants to switch their gazes between the two dots that appear when the lasers are on (see Figure 3). Be careful to check that the eye and head velocities match after this calibration is done. A correct calibration includes a ∆ value below 21. For a detailed description of the calibration procedures, please refer to the manual provided by the manufacturer15,16.
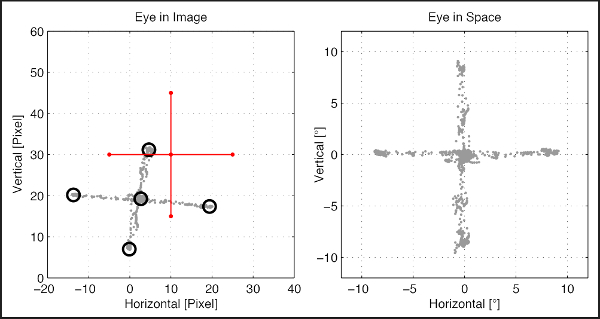
Figure 1: Standard calibration prior to testing of horizontal SCCs with vHIT system A. It should be ensured that "Eye in Image" (image on the left) contains markings equivalent to the four outer limits as well as one in the center and that "Eye in Space" is depicted as a cross with vertical and horizontal lines in zero degrees. Please click here to view a larger version of this figure.
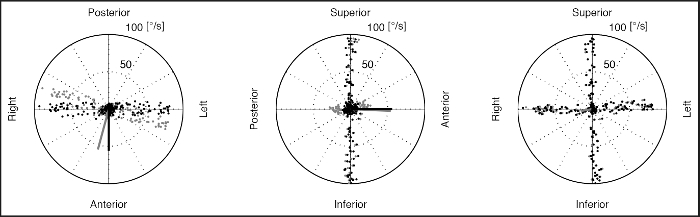
Figure 2: Head calibration for testing prior to testing of vertical SCCs with vHIT system A. Shown is a 3D representation of head movements with respect to the earth. Horizontal and vertical directions are shown together with head movements with respect to the possibly oblique axes of the inertial sensor. The three polar diagrams show the head movements from three different perspectives. Grey dots: raw head movement, black dots: calibrated head movement, solid grey line: camera orientation, solid black line: head orientation. Far left: grey and black dots must follow a line in the right-left direction (horizontal), middle: black and grey dots must follow a line in the superior-inferior direction (vertical), far right: black and grey dots must follow two perpendicular lines looking like a cross. Please click here to view a larger version of this figure.
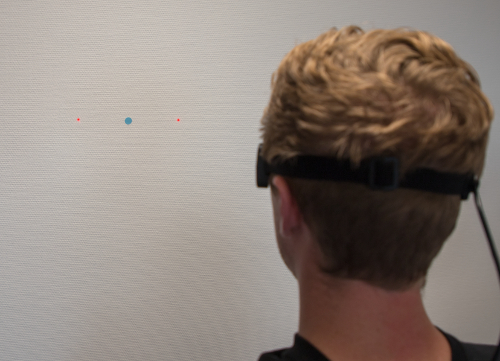
Figure 3: Calibration procedure setup with vHIT system B. Ask the patient to position the left and right dots equidistant on each side of the fixation dot. As the procedure continues, only one dot at a time will be illuminated and the participant is asked to keep their gaze on the visible dot. As the participant’s gaze switches, the system tracks the movement of the pupil. Please click here to view a larger version of this figure.
Testing of the horizontal SCCs are done in a similar fashion with both types of equipment. For testing of the vertical SCCs, either the 2D or 3D test method may be used. Please refer to Figure 4 for a detailed description of the two test methods when testing all six SCCs.
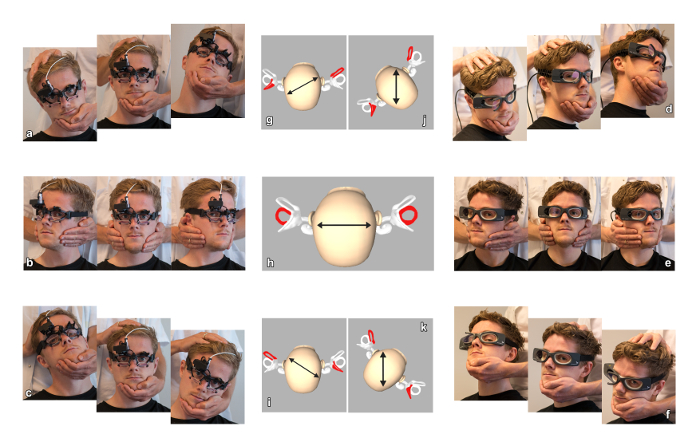
Figure 4: Visualization of the vHIT test procedures. The left side illustrates the 3D vHIT procedure with vHIT system A. The right side illustrates the 2D modified vHIT procedure with vHIT system B. The middle section illustrates orientation of the semicircular canals (SCCs) being tested. The middle section illustrations are modifications of images taken from a smartphone application (see Table of Materials) and are used with permission from the copyright owner. For horizontal SCC testing, the examiner placed his hands on the patient’s jaw, delivering head impulses to each side. For vertical SCC testing, the examiner placed his dominant hand (in this study, both examiners were right-handed) on the top of the head and other hand beneath the chin. (a-c) Illustrations of the performance of the 3D vHIT using vHIT system A. In all three setups, the patient is facing the camera and the head is rotated in the direction of the SCCs being tested. (a) Right anterior left posterior (RALP) SCC testing. (b) Horizontal SCC testing. (c) Left anterior right posterior (LARP) SCC testing. (g–i) Starting position of the head; arrows illustrate the direction in which the head is rotated; the set of SCCs being tested is marked with red. (d–f) Illustrations of the performance of the 2D modified vHIT using vHIT system B. (d) RALP SCC testing with the subject turned 45° to the left and the impulses being delivered by either rotating the head forward or backward. (e) Horizontal SCC testing. (f) LARP SCC testing with the subject turned 45° to the right and the impulses being delivered by either rotating the head forward or backward. By rotating the patient’s head 45° prior to RALP and LARP testing, the eyes align with the axis of the vertical SCCs being tested; therefore, primarily vertical eye movements are produced when applying head impulses. (h), (j), and (k) show the starting positions of the head; the arrows illustrate the direction in which the head is rotated; the set of SCCs being tested is marked with gray. LARP indicates left-anterior-right-posterior plane; RALP indicates right-anterior-left-posterior plane. Reproduction of this figure has been granted with permission. Please click here to view a larger version of this figure.
Every time the vHIT test is performed, all individual steps of the test are important, as they may affect or alter test results. Following completion of every vHIT test, the examiner must go through the report meticulously to determine if results are valid. Special attention must be made to make sure that no noise or artifacts are included in the report. Eight different types of artifacts that may alter results have been described (see Figure 5). Even though the accompanying software removes a lot of noise and/or artifacts from the report, manual deletion of noise and/or artifacts may be needed as an additional step of the evaluation. If the test was carried out properly and participant cooperated fully during the testing, a conclusion of either a normal vestibular function or true compromised function may be drawn following evaluation and interpretation of the report. Please refer to Figure 6, Figure 7, and Figure 8 for test reports following examinations of participants with normal SCC function. Prerequisites for a normal complete vHIT test include mean gain values within the normal range as well as absence of pathological saccades. When mean gain values lie within the normal range, head and eye velocities are almost similar, and the corresponding curves are almost identical in the mirrored view. When no pathological saccades are present, the depiction of both head and eye velocities closely match both during and after application of the head impulses.
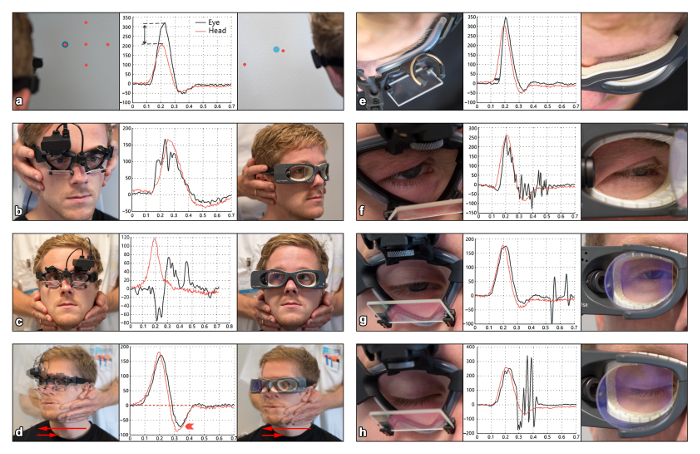
Figure 5: Visualization of eight different artifacts. Each type of artifact is illustrated by a graph as well as accompanying images depicting the test situation triggering the individual artifact (x-axis: time (seconds), y-axis: head and eye velocity (°/s)). Black and red lines indicate eye velocities and head velocities, respectively. The image on the left within a panel shows a subject being tested with vHIT system A, whereas the image on the right shows a subject being tested with vHIT system B. The appurtenant graph shows traces for eye and head movements related to the artifact. (a) Wrong calibration (high gain), (b) touching goggles (two peaks), (c) patient inattention (eye trace goes wrong direction), (d) bounce (head overshoot), (e) loose strap (delay/phase shift), (f) pupil tracking loss (trace oscillations), (g) mini-blink (pseudo-saccade), (h) blink (pseudo-saccade)17. This figure has been modified with permission17. Please click here to view a larger version of this figure.
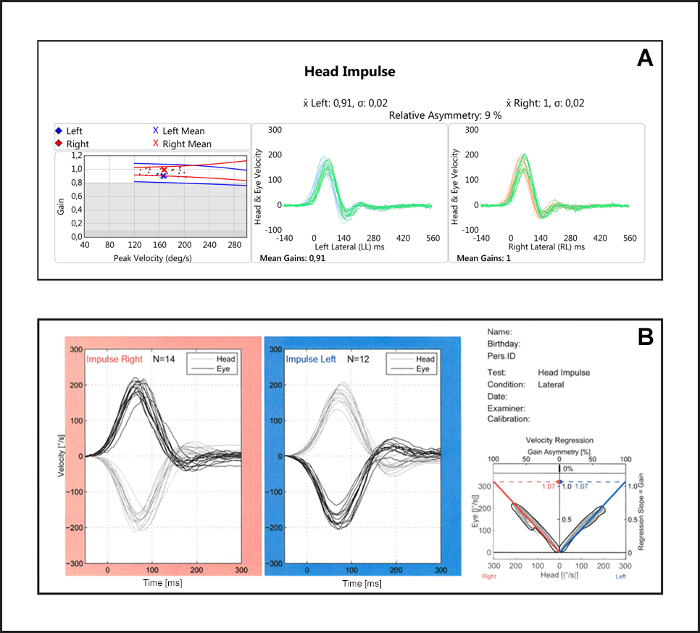
Figure 6: Report with normal findings for lateral SCCs. It should be noted that the curves for both head and eye velocities match, all mean gain values are within the normal range (0.80-1.20), and there are no pathological saccades present. (A) vHIT system B report. Left: gain values are depicted as individual dots representing coherent pars of peak head velocities and gain values; red = right side, blue = left side. Mean gain values are also shown as a numerical value (0.91 and 1). Right: x-axis = time (milliseconds), y-axis = head and eye velocities. Head and eye velocities are shown in the same direction (mirrored view) to ease the interpretation. (B) vHIT system A report. Left: x-axis = time (milliseconds), y-axis = head and eye velocities (°/s). Head and eye velocities are shown in opposite directions. Right: gain values are depicted as a best fitted line through individual dots representing coherent pars of peak head velocities and peek eye velocities (first y-axis) as well as gain values (second y-axis); red = right side, blue = left side. Mean gain values are also shown as a numerical value (1.07 and 1.07). Please click here to view a larger version of this figure.
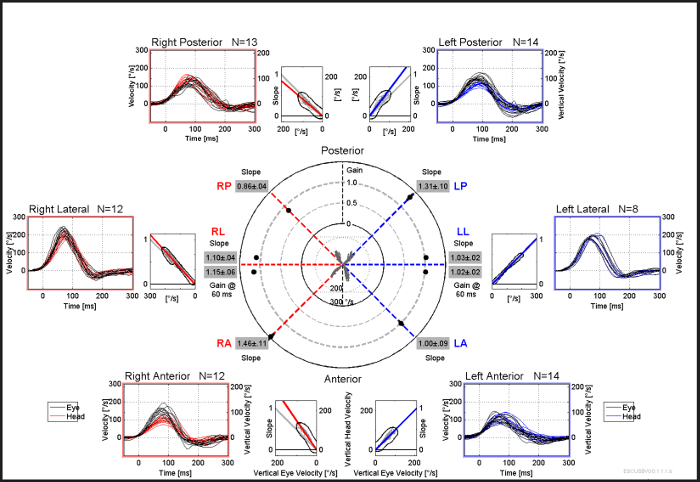
Figure 7: Report with normal findings for all six SCCs following vHIT system A testing. It should be noted that the curves for both head and eye velocities match, all mean gain values are within the normal range (0.80-1.20) or higher, and there are no pathological saccades present. Please click here to view a larger version of this figure.
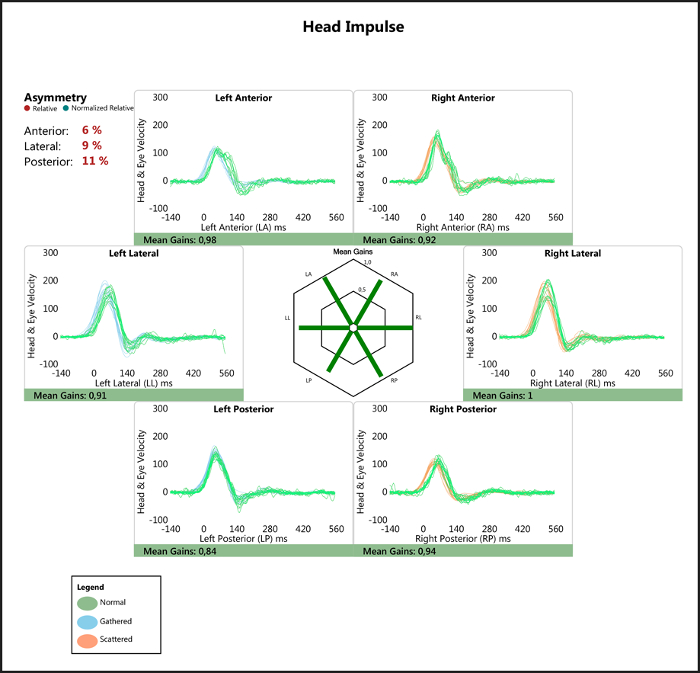
Figure 8: Report with normal findings for all six SCCs following vHIT system B testing. It should be noted that the curves for both head and eye velocities match, all mean gain values are within the normal range (0.80-1.20), and there are no pathological saccades present. Please click here to view a larger version of this figure.
In order to conclude that the vestibular function is reduced a low mean gain value AND pathological saccades must be present. When low mean gain values are present, the amplitude of eye velocity is significantly lower than the corresponding amplitude of head velocity. Pathological saccades must also be present if the examination is truly pathological. These saccades might occur during or after the head movement. In order to conclude if saccades are truly pathological, the examiner must evaluate the saccades in terms of frequency, latency, direction, and amplitude. Please refer to Figure 9 and Figure 10 for examples.
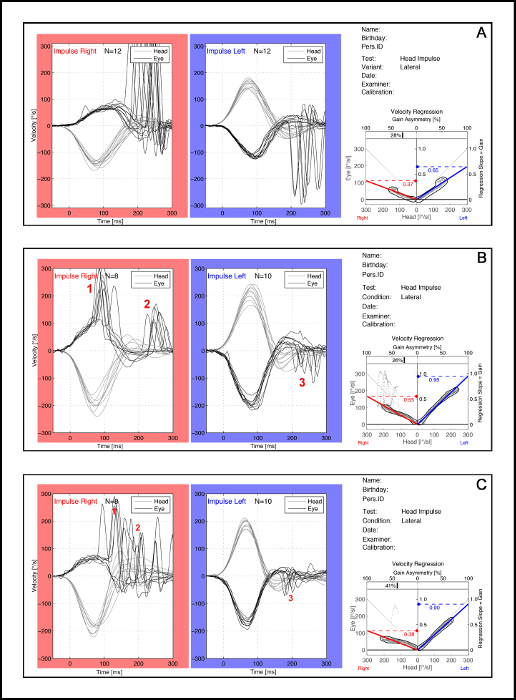
Figure 9: Pathological test results after testing with the vHIT system A. Overt saccades are seen after head movement has stopped (A), covert saccades are seen during the head movement (B), and sometimes a mixture of both are seen (C). It should also be noted that mean gain values are below the normal range on the ipsilateral side of the pathological saccades. In (B) and (C), number 1 in red indicates covert saccades, number 2 in red indicates overt saccades, and number 3 in red indicate small correctional saccades that are classified as non-pathological saccades. Please click here to view a larger version of this figure.
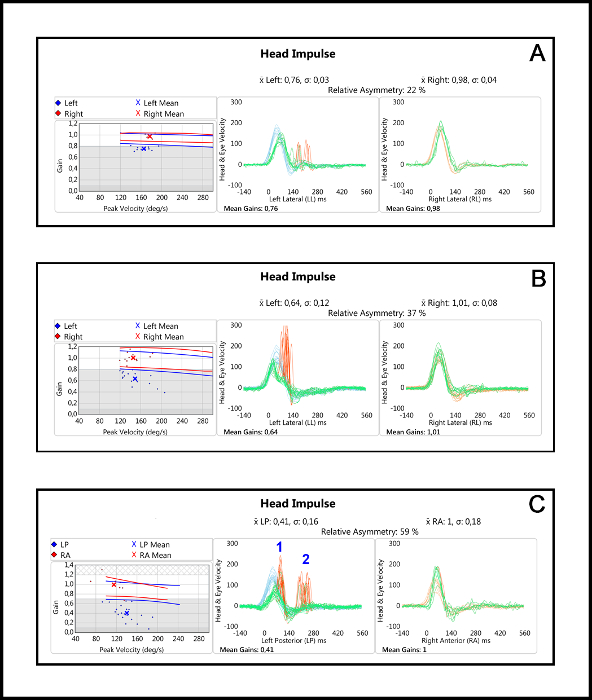
Figure 10: Pathological test results after testing with the vHIT system B. Overt saccades are seen after head movement has stopped (A), covert saccades are seen during the head movement (B), and sometimes a mixture of both are seen (C). It should also be noted that mean gain values are below the normal range on the ipsilateral side of the pathological saccades. In (C), number 1 in blue indicates covert saccades and number 2 in blue indicates overt saccades. Please click here to view a larger version of this figure.
Discussion
The experimental design provided should enable examiners to complete vHIT testing of all six SCCs of the best possible quality. There are several critical steps within the protocol that need to be followed meticulously in order to obtain reliable test results. The pretest evaluation is important because several conditions/diseases may either compromise or alter results. For instance, eye muscle palsies, strabismus, or pupillary malformations may seriously affect the test results even if vestibular function is normal. Calibration of the equipment preceding each test is also very critical, because an imprecise or wrong calibration may greatly influence the results. Special attention should also be given when performing the actual test. The participant needs to be cooperative during the test and, when applying the head impulse, special emphasis should given to directing the impulse towards the correct and desired plane.
Both methods described for vHIT testing possess strengths and weaknesses. Especially when performing vertical vHIT tests, the examiner must consider the positions of the head, eyes, and visual target. The position of the head during head impulses can be with the patient facing the wall or with the head rotated 45° to either side. Practitioners can either turn the head or entire body to obtain this position. It should also be taken into consideration which positions are optimal to individual patients, as cooperation during testing is crucial. Eye movement during testing of the vertical SCCs in the 3D vHIT is both vertical and torsional. In the 2D modified vHIT test method, the torsional component is eliminated by lateralization of the eyeball during testing. The torsional component may add noise to the test, and lateralization of the eyeball may induce artifacts especially from the eyelids or eyelashes. The examiner must also consider the fact that numerous head impulses applied in the vertical planes with continuous lateralization of the eye is fatiguing to a patient. The visual target also needs to be adjusted to each patient’s eye level. If this is not the case, artifacts and noise may alter the test, and it may be difficult for the patient to keep their eyes on the target if the target is not placed optimally during testing. After completion of the test, the examiner most conclude if test results are of sufficient quality and, if necessary, whether or not to perform all steps of the test again. A final evaluation of the test is mandatory and should include manual removal of any noise and/or artifacts before a final conclusion is drawn15,16.
It is of utmost importance that the examiner is aware of potential artifact triggers during the entire vHIT test procedure. There are many different steps during the test that may individually influence final test results5,12,17,18,19. It is important to be aware that the two important parameters provided by the vHIT test, saccades and mean gain values, may not be correct due to artifacts and/or noise and not because of a compromised VOR function. No standard mean gain calculation method exists, and individual manufacturers use different calculation methods. The examiner must thus use caution when comparing mean gain values obtained by different gain calculation methods.
One particular study found no significant mean gain value differences between several vHIT systems if the same gain calculation method was applied19. However, another recent study found differences in mean gain values depending on both the device and gain calculation method used20. Obtaining normative data for each individual vHIT device is therefore advisable21,22,23,24. Several other factors may alter the mean gain values, among these being goggle slippage (either due to a loose strap or examiner touching the googles), too short of a distance to the wall, and any covert saccades (in case the AUC gain calculation method is used)8,12,17,19,25. Furthermore, no clear definition of pathological saccades exists. Therefore, interpretation of the head and eye velocity graphs following the examination is needed to determine whether or not saccades are present. The conclusions drawn after final analysis upon test completion are subject to inter-rater variation and require previous experience with vHIT testing. It is recommended to use precise and uniform criteria defining pathological saccades. Until a consensus is reached on this matter, application of the four standard criteria, defined in a recent study14, is recommended.
During the last decade, vestibular testing has undergone a revolution. Many clinical bedside tests have been replaced by equipment that enables objective testing of all five paired vestibular end organs. vHIT is superior to the subjective bedside head impulse test and is now offered at many clinics and hospitals worldwide as the initial test of vestibular function in vertiginous patients. The test is fast and can be performed with only minor discomfort to the participant. The test is susceptible to several sources of error, which are more likely to occur if the test is not performed following certain predefined standards. Definition of clinical skills, previous experience, and specific requirements/qualifications need to be clearly defined for both clinical use and research purposes before optimal use of the vHIT test is possible. A recent study indicated that some level of prior experience is beneficial when performing the vHIT; therefore, it is recommended that future examiners undergo systematic training before performing vHIT in a clinical setting14. The vHIT test is not just a “plug and play” test; however, if performed correctly, it offers excellent objective diagnostics of vestibular system functioning. This test has a high positive predictive value and offers a specificity very close to one hundred percent14.
Disclosures
Dan Dupont Hougaard has received funding for theoretical courses on vHIT from Otometrics.
Acknowledgements
The authors have no acknowledgements.
Materials
| Name | Company | Catalog Number | Comments |
| EyeSeeCam | Interacoustics, Denmark | Video Head Impulse Test Equipment | |
| ICS Impulse | Otometrics, Denmark | Video Head Impulse Test Equipment | |
| VHIT Ulmer | Synapsys, France | Video Head Impulse Test Equipment | |
| OtoAccess | Interacoustics, Denmark | Software for Video Head Impulse Test | |
| OTOsuite | Otometrics, Denmark | Software for Video Head Impulse Test | |
| aVOR App | Iphone App | Mid section images in figure 4 have been modified from this app |
References
- Kroenke, K., Mangelsdorff, A. D. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. The American Journal of Medicine. 86 (3), 262-266 (1989).
- Neuhauser, H. K., et al. Epidemiology of vestibular vertigo: A neurotologic survey of the general population. Neurology. 65 (6), 898-904 (2005).
- Kroenke, K., Hoffman, R. M., Einstadter, D. How common are various causes of dizziness? A critical review. Southern Medical Journal. 93 (2), 160-167 (2000).
- Halmagyi, G. M., Curthoys, I. S. A clinical sign of canal paresis. Archives of Neurology. 45 (7), 737-739 (1988).
- Halmagyi, G. M., et al. The Video Head Impulse Test. Frontiers in Neurology. (8), (2017).
- Van Esch, B. F., Nobel-Hoff, G. E., van Benthem, P. P., vander Zaag-Loonen, H. J., Bruintjes, T. D. Determining vestibular hypofunction: start with the video-head impulse test. European Archives of Oto-Rhino-Laryngology. 273 (11), 3733-3739 (2016).
- Cleworth, T. W., Carpenter, M. G., Honegger, F., Allum, J. H. J. Differences in head impulse results due to analysis techniques. Journal of Vestibular Research. 27 (2-3), 163-172 (2017).
- Curthoys, I. S., et al. The Video Head Impulse Test (vHIT). Balance Function Assessment and Management 2nd ed. , 391-430 (2014).
- MacDougall, H. G., Weber, K. P., McCarvie, L. A., Halmagyi, G. M., Curthoys, I. S. The video head impulse test: diagnostic accuracy in peripheral vestibulopathy. Neurology. 73 (14), 1134-1141 (2009).
- Agrawal, Y., et al. Evaluation of quantitative head impulse testing using search coils versus video-oculography in older individuals. Otology and Neurotology. 35 (2), 283-288 (2014).
- MacDougall, H. G., McGarvie, L. A., Halmagyi, G. M., Curthoys, I. S., Weber, K. P. The video Head Impulse Test (vHIT) detects vertical semicircular canal dysfunction. PLoS One. 8 (4), 61488 (2013).
- Suh, M. W., et al. Effect of Goggle Slippage on the Video Head Impulse Test Outcome and Its Mechanisms. Otology and Neurotology. 38 (1), 102-109 (2017).
- Migliaccio, A. A., Cremer, P. D. The 2D modified head impulse test: a 2D technique for measuring function in all six semi-circular canals. Journal of Vestibular Research. 21 (4), 227-234 (2011).
- Abrahamsen, E. R., Christensen, A. E., Hougaard, D. D. Intra- and Interexaminer Variability of Two Separate Video Head Impulse Test Systems Assessing All Six Semicircular Canals. Otology and Neurotology. 39 (2), 113-122 (2018).
- . ICS Impulse USB, user guide, Doc. No. 7-50-2060-EN/03 Part No. 7-50-20600-EN Available from: https://partners.natus.com/asset/resource/file/otometrics/asset/7-50-2060-EN_03.PDF (2017)
- Mantokoudis, G., et al. Quantifying the vestibulo-ocular reflex with video-oculography: nature and frequency of artifacts. Audiology and Neurotology. 20 (1), 39-50 (2015).
- Pattersson, J. N., Bassett, A. M., Mollak, C. M., Honaker, J. A. Effects of Hand Placement Tecnique on the Video Head Impulse Test (vHIT) in Younger and Older Adults. Otology and Neurotology. 36 (6), 1061-1068 (2015).
- Kim, T. H., Kim, M. B. Effect of aging and direction of impulse in video head impulse test. Laryngoscope. 128 (6), 228-233 (2018).
- Lee, S. H., et al. Comparison of the Video Head Impulse Test (vHIT) Gains Between Two Commercially Available Devices and by Different Analytical Methods. Otology and Neurotology. 39 (5), 297-300 (2018).
- McGarvie, L. A., et al. The Video Head Impulse Test (vHIT) of Semicircular Canal Function - Age-Dependent Normative Values of VOR Gain in Healthy Subjects. Frontiers in Neurology. (6), (2015).
- Bansal, S., Sinha, S. K. Assessment of VOR gain function and its test-retest reliability in normal hearing individuals. European Archives of Oto-Rhino-Laryngology. 273 (10), 3167-3173 (2016).
- Matino-Soler, E., Esteller-More, E., Martin-Sanchez, J. C., Martinez-Sanchez, J. M., Perez-Fernandez, N. Normative data on angular vestibulo-ocular responses in the yaw axis measured using the video head impulse test. Otology and Neurotology. 36 (3), 466-471 (2015).
- Mossman, B., Mossman, S., Purdie, G., Schneider, E. Age dependent normal horizontal VOR gain of head impulse test as measured with video-oculography. Journal of Otolaryngology Head and Neck. , (2015).
- Yilmaz, O., et al. Influence of Time and Direction Information on Video Head Impulse Gains. Journal of International Advanced Otology. 13 (3), 363-367 (2017).
Erratum
Formal Correction: Erratum: Testing of all Six Semicircular Canals with Video Head Impulse Test Systems
Posted by JoVE Editors on 1/14/2019. Citeable Link.
An erratum was issued for: Testing of all Six Semicircular Canals with Video Head Impulse Test Systems. The article title was updated.
The article title was updated from:
Functional Testing of all Six Semicircular Canals with Video Head Impulse Test Systems
to:
Testing of all Six Semicircular Canals with Video Head Impulse Test Systems
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved