Method Article
Endoscopic Cholesteatoma Surgery
In This Article
Summary
The present protocol describes a step-by-step guide for the complete endoscopic removal of epitympanic cholesteatoma with different techniques for cholesteatoma dissection and bone removal for epitympanectomy.
Abstract
Implementation of endoscopes in cholesteatoma surgery resulted in considerable changes in the management of cholesteatoma in the last two decades. Compared to the microscopic approach with an excellent but straight-line view and limited illumination, the introduction of endoscopes provides a wide-angled panoramic view. Moreover, angled lenses allow the surgeon to visualize the middle ear and its hidden recesses through a transcanal, minimally-invasive approach. The endoscope enables the surgeon to remove limited cholesteatoma of the middle ear and its recesses using an exclusive endoscopic technique by taking advantage of these benefits. This reduces the rate of residual disease and sparing external incisions and excessive temporal bone drilling as in a transmastoid approach. Since transcanal endoscopic access is mainly a one-handed technique, it implies the need for specific procedures and technical refinements. This article describes a step-by-step guide as a surgical manual for endoscopic removal of epitympanic cholesteatoma. Different techniques for cholesteatoma dissection and bone removal for epitympanectomy, including curettage and powered instruments such as drills and ultrasonic devices with their outcomes, are discussed. This may offer ear surgeons insight into technical refinements and the latest technological developments and open the horizon for different techniques.
Introduction
The introduction and successive spread of endoscopic ear surgery led to considerable changes in the treatment of cholesteatoma in the past two decades. The first intraoperative use of endoscopes to prevent residual cholesteatoma was already described in 1993 by Thomassin et al.1, followed by the first description of exclusive endoscopic cholesteatoma surgery in 1997 for cases of limited cholesteatoma2. Compared to the excellent but straight-line view with limited illumination in the microscopic approach, the endoscopic approach provides a panoramic view combined with high resolution, high magnification, and the ability to use angled lenses. The technique experiences increasing interest, despite the loss of binocular vision and two-handed working possibility3. As a consequence of the one-handed technique, safe and sufficient hemostasis is required to reap the benefits of superior visualization of the endoscopic technique4,5.
Traditional microscopic approaches might require a canal wall down (CWD) technique with excessive temporal bone drilling for improved visualization and complete removal of the cholesteatoma6. A less invasive alternative for limited cholesteatoma is the canal wall up (CWU) technique, although the limited visualization is often associated with a higher rate of residual cholesteatoma7. Endoscopes were therefore incorporated as an adjunct in canal wall up surgery to reduce the residual rate of cholesteatoma after CWU surgery1,8. Proceeding from this, the transcanal exclusive endoscopic approach has emerged as a possible alternative approach in cholesteatoma surgery as a minimally invasive approach. This resulted in excellent results in limited cholesteatoma with a comparable rate of residual cholesteatoma compared to the traditional CWD technique9,10,11. Nowadays, the exclusive use of endoscopes in cholesteatoma surgery is increasingly documented in the literature, and indications for exclusive endoscopic approaches are continuously expanding12. This work presents an insight into the different technical refinements and latest technological developments for exclusive endoscopic cholesteatoma surgery.
Protocol
The protocol followed the guidelines of the local institution's human research ethics committee and was approved by the local institutional review board (KEK-BE 2019-00555). All operations were performed in general anesthesia under controlled hypotension in anti-Trendelenburg positioning with standard otological instruments.
1. Preparation of the surgical site
- Manually adjust the endoscope screens (see Table of Materials) according to the surgeon's preferred position (sitting or standing).
- Monitor the facial nerve by checking impedances with a nerve monitoring system (see Table of Materials) and perform a tap test13.
- Disinfect the auricle and the retroauricular region with swabs soaked with commercially available povidone-iodine solution (see Table of Materials).
- Drape the periauricular region with sterile blankets.
- Clean and rinse the external auditory canal (EAC) with a blunt syringe and Ringer solution (see Table of Materials).
- Perform white balancing of the camera with white gauze and apply drops of anti-fog solution to the endoscope lens.
2. Exclusive transcanal endoscopic approach
- Introduce the 0°, 3mm diameter, and 15cm length endoscope in the EAC (see Table of Materials) and clean the EAC by removing earwax and cutting the hairs in the EAC.
- Perform local anesthesia with 0.5 mL of diluted epinephrine (1:200.000) injection (see Table of Materials), each using four injection sites in all quadrants of the EAC under endoscopic control. Additionally, inject 0.5 mL of diluted epinephrine (1:200.000) to the vascular strip in the posterior-superior quadrant of the EAC.
- Inspect the tympanic membrane and the attic region with the 0° endoscope.
- Elevate a tympanomeatal flap tailored to disease extension using an angled round knife and provide hemostasis with epinephrine (1:1000) soaked cottonoids.
NOTE: Additional hemostasis may be applied by electrocoagulation using mono- or bipolar cautery; alternatively, radio-frequency-cautery can be used (see Table of Materials). Be careful to use monopolar at the lowest intensities to minimize risks of spread of electricity to the facial nerve. - Expose the annulus and, if possible, the chorda tympani; open the middle ear cavity, and evaluate in detail the cholesteatoma extension.
- Carefully separate the cholesteatoma matrix from the eardrum and from the chorda tympani.
- Carefully dissect the cholesteatoma involving the middle ear and the incudostapedial area in case of an intact ossicular chain.
- Perform limited atticotomy using unpowered instruments, bone drilling, or ultrasonic devices (see Table of Materials) by stepwise removal of the lateral portion of the attic and evaluate the extent of cholesteatoma infiltration by following the steps below.
- For atticotomy with unpowered instruments: remove small parts of bone, especially the scutum, by a bone curette using rotatory movements or chisel and hammer.
- For attico- and antrotomy with bone drilling: remove larger parts of bone either in an underwater technique14, followed by cutting burrs at low speed (2000-8000 rpm) or cutting or coarse diamond burrs at slow speed with only a little irrigation.
NOTE: For the underwater technique, the EAC is filled with 0.9% of NaCl solution, and the endoscope lens is inserted into the EAC with the burrs. Subsequently, drilling for attico- and antrotomy is performed directly under visual inspection. Occasional suction is required due to bone dust and reduced visibility. Utmost care has to be applied to prevent damage to surrounding structures by direct or heat damage. The delicate lens and shaft of the endoscope have to be kept away from the rotatory instruments to prevent its damage. - For attico- and antrotomy with ultrasonic devices: remove the larger parts of bone with the curved tip in an underwater technique to prevent heat damage to bone and soft tissues.
CAUTION: Do not touch the ossicular chain and the cochlea due to possible inner ear hair cell damage due to transmission of micro-vibrations.
- If the cholesteatoma infiltrates deep into the anterior epitympanum or erodes the incus, remove the incus and, if required, the malleus head to entirely remove the cholesteatoma.
- Perform stepwise attico- and antrotomy with different devices (see Table of Materials) to follow and completely extirpate the cholesteatoma. Use angled dissectors if appropriate.
3. Middle ear exploration
- After completion of cholesteatoma resection, an entire middle ear exploration with an emphasis on residual cholesteatoma and functional considerations with the greatest sparing of healthy mucosa is performed. Use first 0° then a 45° angled lens.
NOTE: If appropriate, a 70° endoscope may also be used. - Check anterior epitympanic space, tegmen tympani, posterior epitympanum, antrum until the posterior limit of the lateral semicircular canal.
- Carefully inspect the retrotympanum, including posterior sinus, sinus tympani, subtympanic sinus, and hypotympanum.
- Check Eustachian tube, protympanum, supratubar recess, tensor fold, and isthmus; restore the ventilation route by tissue removal in case of obstruction.
4. Reconstruction of the ossicular chain and scutum
- Perform an incision 5 mm posterior to the tragus edge and cut through to the cartilage, then harvest a large piece of cartilage with perichondrium on both sides.
- Reconstruct the scutum with a trimmed piece of cartilage and perichondrium for defect closure after attico- and antrotomy.
- Perform underlay tympanoplasty using a trimmed piece of cartilage with overlapping perichondrium in island-graft technique or temporalis fascia for defect closure of the tympanic membrane. Add perichondrium in case of cartilage use for supporting the construction if necessary.
- If the stapes is intact, inspect the incus or head of the malleolus for possible malleolar head or incus interposition ossiculoplasty; otherwise, use double-block cartilage (Malafronte technique15) or PORP (partial ossicular replacement prosthesis).
- Use a TORP (total ossicular replacement prosthesis) if the stapes supra-structure is also affected by cholesteatoma and needs to be removed.
- Use resorbable gelatinous sponges to secure the reconstruction, reinforce the reconstruction using a pressed perichondrium layer or cartilage in case of PORP/TORP.
5. Wound closure
- Reposition the tympanomeatal flap and adapt it to the EAC curvature without sutures.
- Splint the tympanic membrane with silicone or silk strips of adequate size for defect coverage.
- Pack the EAC with a resorbable gelatinous sponge and the outer part with an antibiotic (polymyxin, neomycin) and hydrocortisone soaked gauze (see Table of Materials).
Results
A total of 43 consecutive cases of exclusive endoscopic cholesteatoma surgery were analyzed for this study. One surgeon performed all operations; cases needing conversion to a microscopic or combined approach were excluded. Preoperative computed tomography suspected an epitympanal cholesteatoma extension in every case. The mean age (±standard deviation) at the surgery date was 37.36 years (±15.64 years). Seven cases (16.3%) were revision surgeries, thirty-six cases (83.7%) were patients undergoing first cholesteatoma removal. The left side was operated in 26 cases (60.5%), the right side in 17 cases (39.5%).
Surgical Results
All operations were completed without significant complications like facial nerve palsy or postoperative sensorineural hearing loss, as illustrated in Figure 1. Cartilage was used as grafting material in 38 cases (88.4%) and fascia in 5 cases (11.6%). The graft intake rate (GIR) was 90.7% showing 3 cases of postoperative perforations (7.3%). The mean follow-up was 17.4 months (±10 months), with 40 cases (93%) having no recurrent cholesteatoma at the last follow-up.
Audiological Results
Each patient underwent standard audiological testing before and after surgery. One patient was already deaf before surgery; thus, no hearing improvement was expected. Two more patients had no postoperative audiogram. Preoperative air bone gap (ABG) of 23.8 dB ± 12.6 dB improved significantly (paired t-test with p = 0.0005) to a postoperative ABG of 18.2 dB ± 10 dB after surgery. The detailed surgical results are presented in Table 1.
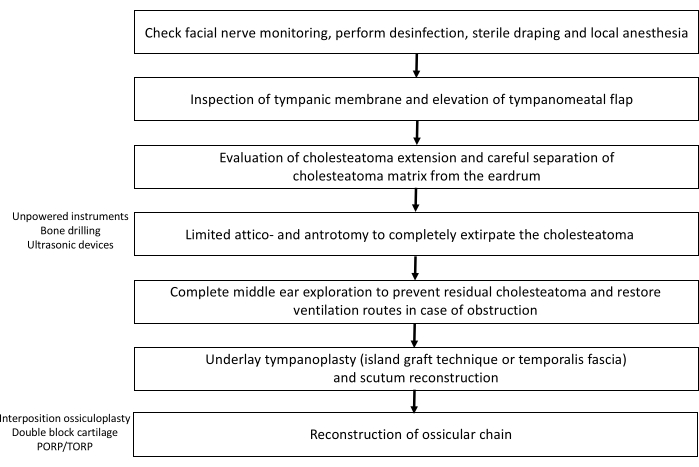
Figure 1: Overview of the essential surgical steps. Please click here to view a larger version of this figure.
| Age | 37.4 years (14-80 years) | ||
| Side | 26 left side | 17 right side | |
| Revision surgery | 36 primary surgery | 7 revision surgery | |
| Grafting sucess | 39 successful | 3 perforations | 1 missing follow up |
| Grafting material | 38 cartilage | 5 fascia | |
| Recidive | 40 without recidive | 3 with recidive | |
| Mean ABG | 23.8 ± 12.6 dB preoperative | 18.2 ± 10 dB postoperative |
Table 1: Detailed surgical results.
Discussion
This article describes a step-by-step guide as a surgical manual for endoscopic removal of limited attic cholesteatoma. Different techniques for cholesteatoma dissection and bone removal techniques for atticotomy as curettage, bone drills, and ultrasonic devices (piezoelectric devices, ultrasonic bone curettes) are presented. However, single-handed surgery requires habituation, and particular care has to be taken to avoid damage to surrounding structures directly or indirectly during attico- and antrotomy with powered instruments.
Since the first description of exclusive endoscopic cholesteatoma surgery for limited cholesteatoma by Tarabichi in 19972, several studies have been published reporting its successful application in cases of limited attic cholesteatoma. Tarabichi presented in 2004 a cohort of 73 procedures in 69 patients, who all received transcanal exclusive endoscopic cholesteatoma removal, showing 5 cases of recurrence in a mean follow-up period of 43 months9. In 2008, Barakate and Botrill presented 68 procedures of endoscopic cholesteatoma surgery in 66 cases, all of them receiving a second look procedure within a mean of 16 months16. In the second look procedure, 10 ears revealed residual disease, and 4 ears presented a recurrence. Migirov et al. demonstrated no residual disease in 18 patients after exclusive endoscopic cholesteatoma eradication after more than 1 year10. In 2013 Marchioni et al. reported on 146 patients with attic cholesteatoma and 120 patients undergoing an exclusive endoscopic approach; 26 patients underwent an endoscopic procedure combined with mastoidectomy11. Thereof, 7 patients presented with residual cholesteatoma, with no case having limited attic cholesteatoma in the beginning. Thus, the residual and recurrent cholesteatoma rate of 6.4% after endoscopic assisted or exclusive endoscopic removal seems to be comparable to the rate after most CWD procedures with 0%-13.2%, while using a minimally invasive approach7,17. In addition, direct comparison of endoscopic with microscopic techniques revealed significantly better middle ear structural visibility, reduced pain scores, and faster wound healing as further advantages of an endoscopic minimally-invasive approach8,18. Thus, the endoscopic approach seems to be particularly suitable for limited attic cholesteatoma.
Nevertheless, the inaccessibility of cholesteatoma extending deep into the mastoid remains one of the limiting factors in the success of the transcanal exclusive endoscopic approach. Despite the use of angled optics, complete endoscopic explorability is not always feasible, especially in the case of more excavated retrotympanal regions20.
Extended atticotomy was mainly performed by curettes or bone drilling until recently. To avoid the rough and time-consuming bone removal with curettes and possible facial nerve or tympanomeatal flap injury caused by drills, ultrasonic devices may provide a safe and precise alternative in cholesteatoma surgery21. With the transcanal endoscopic retrograde mastoidectomy technique, even removing cholesteatoma extensions into the antrum in a sclerotic mastoid can be achieved by an exclusive endoscopic transcanal approach22,23. However, extensive cholesteatoma formation inside the mastoid or severe hemorrhage might require switching to a microscopic retroauricular approach.
Additionally, there are also recent developments described in the literature to reduce the residual rate of cholesteatoma with chemically or physically assisted dissections. Mesna (sodium 2-mercaptoethanesulfonate) is reported as a possible chemical agent to reduce the residual rate of cholesteatoma by breaking disulfide bridges between different tissues24,25. For physically assisted dissection, different types of lasers known from stapes mobilization procedures have also been used in cholesteatoma surgery, resulting in a low recurrence rate around the ossicular chain26. In addition to white light endoscopy, other image processing technologies based on spectral separation may further improve cholesteatoma removal by recognizing residual cholesteatoma in the final overview27.
Therefore, applying endoscopic cholesteatoma surgery with improved technical devices and chemically or physically assisted dissection is promising to further evolve the minimally invasive approach and reduce the residual disease rate.
Disclosures
LA is a consultant for Stryker ENT. All other authors declare no conflict of interest.
Acknowledgements
Not applicable.
Materials
| Name | Company | Catalog Number | Comments |
| Antifog Solution | Karl Storz | N/A | |
| Epinephrine 1 mg/mL | Dr. Bichsel AG | N/A | |
| Gelatinous sponge (Gelfoam) | Pfizer | N/A | |
| HOPKINS Optic 0° | Karl Storz | 7220AA | |
| HOPKINS Optic 30° | Karl Storz | 7220BA | |
| HOPKINS Optic 45° | Karl Storz | 7220FA | |
| HOPKINS Optic 70° | Karl Storz | 7220CA | |
| Image 1S 4K | Karl Storz | TH120 | |
| ME 102 | KLS Martin | N/A | |
| Monitor 32" 4K/3D | Karl Storz | TM350 | |
| NIM-Neuro 3.0 | Medtronic | N/A | |
| OsseoDuo | Bien Air | N/A | |
| Otosporin (polymyxin, neomycin, hydrocortison) | GlaxoSmithKline | N/A | |
| Piezosurgery device | Mectron | N/A | |
| PM2 Line Drill | Bien Air | N/A | |
| Povidone-iodine (Betadine) | Mundi-Pharma | N/A | |
| Ringer Solution | B. Braun | N/A | |
| Standard otological instruments | Karl Storz | N/A | |
| Steel and diamand burrs | Bien Air | N/A | |
| Syringe Injekt Solo 10 mL | B. Braun | N/A |
References
- Thomassin, J. M., Korchia, D., Duchon Doris, J. M. Endoscopic-guided otosurgery in the prevention of residual cholesteatomas. The Laryngoscope. 103 (8), 939-943 (1993).
- Tarabichi, M. Endoscopic management of acquired cholesteatoma. The American Journal of Otology. 18 (5), 544-549 (1997).
- Emre, I. E., Cingi, C., Bayar Muluk, N., Nogueira, J. F. Endoscopic ear surgery. Journal of Otology. 15 (1), 27-32 (2020).
- Anschuetz, L., et al. Management of bleeding in exclusive endoscopic ear surgery: Pilot Clinical Experience. Otolaryngology-Head and Neck Surgery. 157 (4), 700-706 (2017).
- Alicandri-Ciufelli, M., Molinari, G., Beckmann, S., Caversaccio, M., Presutti, L., Anschuetz, L. Epinephrine use in endoscopic ear surgery: Quantitative safety assessment. Journal for Oto-Rhino-Laryngology. 82 (1), 1-7 (2020).
- Hulka, G. F., McElveen, J. T. A randomized, blinded study of canal wall up versus canal wall down mastoidectomy determining the differences in viewing middle ear anatomy and pathology. The American Journal of Otology. 19 (5), 574-578 (1998).
- Kerckhoffs, K. G. P., et al. The disease recurrence rate after the canal wall up or canal wall down technique in adults. The Laryngoscope. 126 (4), 980-987 (2016).
- Ayache, S., Tramier, B., Strunski, V. Otoendoscopy in cholesteatoma surgery of the middle ear: What benefits can be expected. Otology and Neurotology. 29 (8), 1085-1090 (2008).
- Tarabichi, M. Endoscopic management of limited attic cholesteatoma. The Laryngoscope. 114 (7), 1157-1162 (2004).
- Migirov, L., Shapira, Y., Horowitz, Z., Wolf, M. Exclusive endoscopic ear surgery for acquired cholesteatoma: Preliminary results. Otology and Neurotology. 32 (3), 433-436 (2011).
- Marchioni, D., Villari, D., Mattioli, F., Alicandri-Ciufelli, M., Piccinini, A., Presutti, L. Endoscopic management of attic cholesteatoma. A single-institution experience. Otolaryngologic Clinics of North America. 46 (2), 201-209 (2013).
- Kozin, E. D., et al. Systematic review of outcomes following observational and operative endoscopic middle ear surgery. The Laryngoscope. 125 (5), 1205-1214 (2015).
- Kartush, J. M., Rice, K. S., Minahan, R. E., Balzer, G. K., Yingling, C. D., Seubert, C. N. Best practices in facial nerve monitoring. The Laryngoscope. 131 (4), 1-42 (2021).
- Chen, Y., et al. The treatment of cholesteatomas involving the antrum and mastoid using transcanal underwater endoscopic ear surgery. Otology and Neurotology. 41 (10), 1379-1386 (2020).
- Malafronte, G., Filosa, B., Mercone, F. A new double-cartilage block ossiculoplasty: Long-term results. Otology and Neurotology. 29 (4), 531-533 (2008).
- Barakate, M., Bottrill, I. Combined approach tympanoplasty for cholesteatoma: Impact of middle-ear endoscopy. Journal of Laryngology and Otology. 122 (2), 120-124 (2008).
- Verma, B., Dabholkar, Y. G. Role of endoscopy in surgical management of cholesteatoma: A systematic review. Journal of Otology. 15 (4), 166-170 (2020).
- Magliulo, G., Iannella, G. Endoscopic versus microscopic approach in attic cholesteatoma surgery. American Journal of Otolaryngology - Head and Neck Medicine and Surgery. 39 (1), 25-30 (2018).
- Das, A., Mitra, S., Ghosh, D., Sengupta, A. Endoscopic versus microscopic management of attic cholesteatoma: A randomized controlled trial. The Laryngoscope. 130 (10), 2461-2466 (2020).
- Anschuetz, L., Alicandri-Ciufelli, M., Bonali, M., et al. Novel surgical and radiologic classification of the subtympanic sinus: Implications for endoscopic ear surgery. Otolaryngology - Head and Neck Surgery. 159 (6), 1037-1042 (2018).
- Salami, A., Mora, R., Dellepiane, M., Crippa, B., Santomauro, V., Guastini, L. Piezosurgery® versus microdrill in intact canal wall mastoidectomy. European Archives of Oto-Rhino-Laryngology. 267 (11), 1705-1711 (2010).
- Kakehata, S., Watanabe, T., Ito, T., Kubota, T., Furukawa, T. Extension of indications for transcanal endoscopic ear surgery using an ultrasonic bone curette for cholesteatomas. Otology and Neurotology. 35 (1), 101-107 (2014).
- Mehta, R., Mankekar, G., Mayland, E., Melder, K., Arriaga, M. A. Endoscopic inside-out mastoidectomy with the ultrasonic bone aspirator. OTO Open. 3 (1), 1-4 (2019).
- Vincenti, V., Magnan, J., Saccardi, M. S., Zini, C. Chemically assisted dissection by means of mesna in cholesteatoma surgery. Otology and Neurotology. 35 (10), 1819-1824 (2014).
- de la Torre, C., Villamor, P. Chemically assisted dissection with sodium 2 mercaptoethanesulfonate (MESNA) in the surgical management of pediatric cholesteatoma. Otology and Neurotology. 40 (5), 645-650 (2019).
- Lee, C. H., Kim, M. K., Kim, H. M., Won, C., Shin, T. H., Kim, S. Y. Endaural laser-assisted single-stage inside-out cholesteatoma surgery (LASIC) to treat advanced congenital cholesteatoma. Otology and Neurotology. 40 (7), 927-935 (2019).
- Lucidi, D., et al. Use of IMAGE1 S technology for detection of cholesteatoma in endoscopic ear surgery: a retrospective case series on 45 patients. European Archives of Oto-Rhino-Laryngology. 278 (5), 1373-1380 (2021).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved