Method Article
Piezo High Accuracy Surgical Osteal Removal (PHASOR): A Technique for Improved Cranial Window Surgery in Mice
In This Article
Summary
Piezoelectric surgery has led to improvements in human maxillofacial and dental surgery. We have developed a protocol to optimize piezoelectric surgery for cranial window surgery in mice.
Abstract
Multiphoton microscopy has been widely adapted for imaging neurons in vivo. Repeated imaging requires implantation of a cranial window or repeated thinning of the skull. Cranial window surgery is typically performed with a high speed rotary drill, and many investigators find it challenging to prevent the drill from damaging the delicate dura and blood vessels. Extensive training and practice is required to remove the bone without damage to underlying tissue and thus cranial window surgery can be difficult, time consuming, and produce tissue damage. Piezoelectric surgery, which is extensively used for maxillofacial and dental surgery, utilizes ultrasonic vibrations to remove bone without damaging soft tissues. We have developed a method applying piezoelectric surgery to improve cranial window surgery in mice in preparation for multiphoton imaging. Comparisons within our lab find that the method requires less surgery time and has a lower average rate of complications due to dural bleeding than cranial window surgery with a rotary drill.
Introduction
Cranial window surgery to prepare rodents for multiphoton imaging in vivo has become an important technique in neuroscience. The removal or thinning of bone is necessary to prepare the mouse for optical imaging with a multiphoton microscope. This surgery is performed either by completely removing an area of bone to expose the underlying dura1, or by thinning a region of bone without full removal from the dura2. The thin skull approach may produce less inflammation and activation of microglia3 but provides a shallower depth of imaging, a smaller imaging window size (200 µm) and a limited time period during which the window can be imaged due to bone regrowth2. The addition of a polished and reinforced glass window (PoRTS) can increase the imaging size and imaging period but is difficult to perform4.
Both current surgeries use a high speed rotary drill to thin or remove the bone from the skull. The thin skull technique also uses a scalpel after the drill to further thin the bone2. The PoRTS technique requires the extra step of high speed polishing with grit4. In a high speed rotary drill, an air powered turbine or electric motor causes the drill bit to spin at a high velocity. As rotary drills section both bone and soft tissue, there is a risk of damaging the dura and underlying blood vessels. The success of the surgery depends on the skill of the surgeon. In addition to these windows prepared with mechanical surgical methods, a chemical method of optically clearing the skull with different solutions has been developed5,6. However, since piezoelectric surgery is a mechanical method of surgery, our comparisons here will be limited to other mechanical methods.
Piezoelectric surgical devices utilize ultrasonic vibrations to break down mineralized bone without damaging underlying soft tissue, and thus offer an approach to rapidly thin a large area of bone. In a piezoelectric surgical handpiece, the turbine is replaced by a stack of ceramic disks and when current is applied, the disks vibrate at ultrasonic frequencies. The vibrations are transferred through the handpiece to diamond coated tips to cut through bone without damaging soft tissues, an advantage over rotary drills that do not discriminate between tissue types. Piezoelectric surgery was originally developed for use in human by Tomaso Vercellotti and has led to improvements in dental and cranio-maxilofacial surgery7,8,9,10,11.
Piezoelectric surgery has been used to create an osteotomy in Wistar rats and was found by magnetic resonance imaging (MRI) and histology to produce significantly less damage than a traditional dental drill12. The authors concluded that piezoelectric surgery was safe for removing the bone near soft brain tissue. Mice, however, have a thinner dura that is more easily damaged, and that study did not prepare windows for chronic optical imaging. Chronic imaging requires that blood vessels are not damaged and that blood clots do not form under the window. Damage to the dura leads to inflammation that causes the window to cloud, and activates microglia and the proliferation of reactive astrocytes. Here we have optimized piezoelectric surgery for mice to create both thin skull and full bone removal cranial windows suitable for chronic imaging. We compared this surgical technique to cranial window surgeries prepared with a high speed rotary drill.
Protocol
All procedures involving animals were performed according to the standards set by the Columbia University Medical Center Institutional Animal Care and Use Committee (IACUC). Euthanasia was performed via cervical dislocation under anesthesia with ketamine 100 mg/kg and xylazine 10 mg/kg injected intraperitoneally. All surgical procedures were performed in a sterile manner (surgeon was wearing head cap, face mask, sterile gloves, and clean disposable lab coat) and surgical tools were autoclaved between each use.
1. Presurgical Steps
- Autoclave all surgical instruments to ensure sterility.
- Anesthetize C57bl6 mice with isoflurane (4% for induction and 1.5-2% for surgery). Pinch the hind toe every 10 min to ensure proper depth of anesthesia. Increase anesthesia if vocalization or hind limb retraction is seen.
- Apply veterinary eye lubricant to the eyes to prevent drying.
- Remove the hair over the scalp with a 3 min application of hair removal gel or by shaving with an electric razor.
- Place the mouse in the stereotaxic frame on a heating pad or calibrated water recirculating blanket set to 38°C.
- Administer buprenorphine (0.1 mg/kg) subcutaneously to provide presurgical analgesia.
- Disinfect the scalp with three alternating applications of chlorhexidine or betadine and 70% ethanol using a cotton tipped applicator.
- Inject 100 mL of bupivacaine diluted 50% in saline under the scalp to provide local anesthesia.
2. Piezoelectric Cranial Window Surgery
- Using autoclaved sterile surgical instruments, remove a 1 cm circle of scalp over the skull by cutting with surgical scissors in a circular pattern. Lift the scalp off the skull exposing the periosteum tissue over the bone.
- Use the tip of forceps to scrape the exposed bone clear of any remaining periosteum tissue. This is important to ensure that the dental cement will not fall off later.
- Set the piezoelectric surgery unit to vibrate on the lowest setting. Note that higher settings may break blood vessels due to intense vibrations.
- Fix the sterile circular tip to the handpiece.
NOTE: The 4 mm circular tip is well suited for surgeries. The large tip size contributes to the speed of the surgery as the entire window can be thinned simultaneously. - Fill a 10 mL syringe with ice cold artificial cerebrospinal fluid (ACSF) and hold it in the hand not holding the piezoelectric handpiece.
- Irrigate the skull by dripping the ACSF from the syringe onto the skull at a rate of 1 mL/min. Alternatively, use a peristaltic pump positioned over the skull to free the use of the other hand.
NOTE: Irrigation with cold ACSF is important to prevent overheating due to the friction from the high frequency vibrations. - Gently apply the vibrating surgical tip to the skull with a light circular motion (3 circles per 1 s) and thin the bone to the desired depth to perform a thin skull preparation (5 to 10 min).
NOTE: Here, 4 mm windows were made that were thinned to 20 µm. However, the size of the window will vary with the size of the surgical tip. The thickness of the bone can be adjusted to the desired depth based on the length of time spent applying the tip to the skull. - Gently adjust the angle of the handpiece and change the angle of the tip while applying pressure to the skull to thin the skull uniformly.
- To perform a complete bone removal without leaving any thin bone behind, thin the bone until cracks are visible around the window area. Remove the remaining flakes of thin bone with forceps without damaging the underlying dura.
- Soak a 1 mm piece of hemostatic collagen foam in cold ACSF. Hold the wet foam with forceps and place it on the thin skull. Allow it to sit on the thin skull for about 30 s to stop any micro bleeds from developing.
- Use forceps to place a 4 mm glass coverslip laterally over the window that has been thinned into the bone.
- Use the back of a small plastic or wooden cotton tipped applicator to apply approximately 100 µL of dental acrylic to the skull to hold the window in place.
3. Post Surgical Care
- Remove the mouse from the surgical apparatus and place it in a heated cage for recovery. Monitor it continuously until it has regained full consciousness (assessed by normal mobility, gait, and behavior).
- Assess the animals twice a day for three days for manifestations of post-surgical pain including decreased activity, grooming, food, and water consumption, guarding behavior (e.g. limping or a hunched posture) or increased aggression. Do not return the animal to the company of other animals until it has fully recovered.
- Administer Buprenorphine (0.05–0.1 mg/kg) subcutaneously as an analgesic 8–12 h after the surgery for 3 days. Monitor the area of the window closely following surgery for dehiscence, inflammation, and signs of infection. If the animal does not return to baseline feeding and grooming behaviors, consult a veterinarian regarding possible interventions or euthanasia.
Results
Before proceeding with piezoelectric surgery, remove any residual periosteum from the skull. Once the skull is opaque and smooth (Figure 1a), the surgeon may begin piezoelectric surgery. When removing bone with the vibrating piezo tip, it is critical to irrigate the skull with ice cold ACSF. Proper irrigation is achieved when the bottom 1 mm of the tip is submerged in ACSF (Figure 1b). Without proper irrigation, the bone will overheat and damage the brain. After the skull has been thinned to the desired depth chosen by the surgeon, there may be some residual bleeding from blood vessels located in the bone. In order to rapidly cease all bleeding, apply a small 1 mm piece of collagen foam soaked in ACSF to the area of the window. Let the collagen sit on the skull for approximately 30 s (Figure 1c). After the collagen foam is removed, the window will appear translucent, allowing clear visualization of the blood vessels in the dura. The dura will be intact without significant bruising. (Figure 1d). If the dura appears red and inflamed, it is likely due to broken blood vessels from too much pressure applied to the tip during the surgery. To protect the new window and prepare it for chronic imaging, a glass coverslip must be placed over the area. A properly applied glass coverslip will gently sit on top of the window and will not cause any damage to the area. The glass coverslip must cover the entire window. If the glass coverslip is properly applied to the skull, the window will remain translucent under the glass. All the blood vessels in the dura will still be visible (Figure 1e). Dental acrylic must be applied around the glass coverslip to permanently adhere it to the surface of the skull. The edges of the glass coverslip must also be covered in dental acrylic (Figure 1f).
We found that piezoelectric surgery is typically much faster than a traditional cranial window, taking around 10-12 min per surgery (Figure 2A). We also found that there were less complications due to dura bruising and bleeding as observed by eye (Figure 2B). A properly prepared window will allow multiphoton imaging of fluorescent indicators in cortical neurons in vivo. We chose to image the red calcium indicator JRGECO1a in cell bodies of layer 4 cortical neurons (Figure 3A-3B). We could observe calcium transients in these cell bodies through the window prepared using PHASOR.

Figure 1: Piezoelectric surgery. (a) The skull after it has been properly prepared for PHASOR. All the periosteal tissue has been removed, leaving a smooth and clean surface. (b) A representative image of PHASOR in progress. The bottom 1 mm of the vibrating surgical tip is submerged in ice cold ACSF. The fluid is applied to the skull at a rate of 1 mL/min. A light circular motion is applied to the skull and the bone is thinned via ultrasonic vibrations. (c) After the skull has been thinned, a 1 mm circular piece of collagen foam soaked in cold ACSF is allowed to rest on the window to stop any micro bleeds from the bone. (d) A successful window with a translucent dura displays all of the intact blood vessels. There is no visible damage or bruising to the surface of the brain. (e) A glass coverslip is placed over the window to protect the surface of the brain. (f) Dental acrylic is applied to the skull to permanently fix the glass coverslip over the window. Scale bar 1 mm in all images.
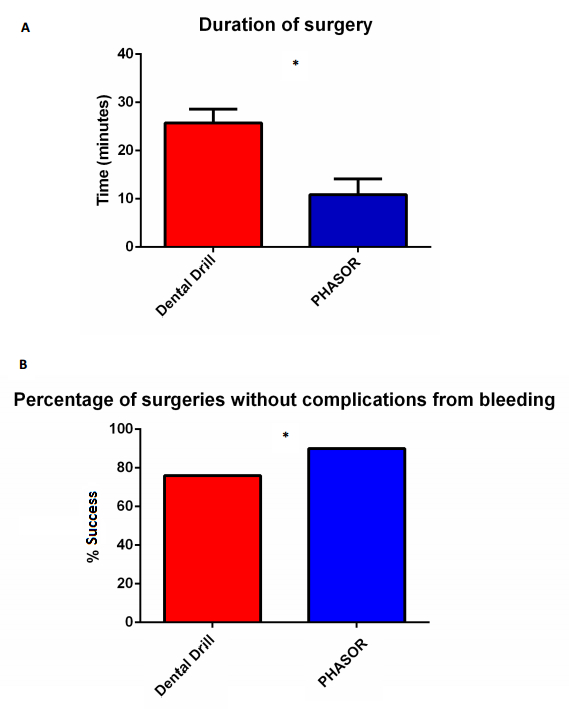
Figure 2. Comparison of success rate in training for PHASOR or dental drill surgery. (A) Average time per surgery was lower for PHASOR than dental drill surgeries (p<0.05, two tailed t test) n= 30 surgeries per group and average 10 surgeries per surgeon. (B) The percentage of successful surgeries (defined as no bleeding or visible damage to the dura as observed by the surgeon's eye through the objective set to 350X zoom) was higher for PHASOR than dental drill surgeries (n = 30 surgeries for each group, one tailed z test). Error bars show SD.
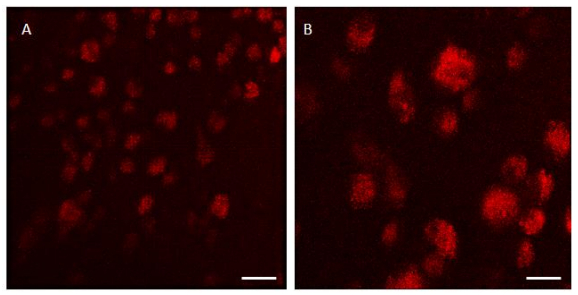
Figure 3. Multiphoton imaging in vivo through a cranial window thinned with PHASOR. (A) Calcium transients observed with the red calcium indicator JRGECO1a were imaged in layer 4 pyramidal neurons in murine motor cortex in vivo. Scale bar = 100 µm. (B) The same window but different region of layer 4 motor cortex. Headfixed mouse with 3 mm window prepared with PHASOR. Scale bar = 30 µm. Imaged with a multiphoton microscope, 40X objective, 1040 nm excitation wavelength.
Discussion
The surgery can be modified by changing the surgical tip. There are many different sizes of tip that can be applied to the handpiece. Changing the size or shape of the tip will result in different sized windows. In addition to the 4 mm tip, we also tried a 3 mm tip and found it also worked well. Even with irrigation with ice cold ACSF, we were not able to get good results with tips that were too narrow (approximately 0.25 mm) due to the concentrated vibrations causing too much heat and burning the bone leading to damage to the underlying dura. We have not tried the multitude of other tips that are available, and we anticipate that other labs may find new applications for these different tips. While the surgery is relatively straightforward, we found that there are several steps that may require troubleshooting. The first is that the vibrating tip produces a lot of turbulence in the ACSF, which diminishes visibility and produces difficulty in ascertaining bone depth during the bone thinning step of the surgery. We recommend that if it is too difficult to see how thin the bone is, take a break to dry the skull and window by applying a sterile cotton swab to the side of the bone. Do not apply the cotton swab directly to the window, since the rough surface is damaging to thin bone. After checking the depth, reapply ACSF and continue with the surgery. We also found that if there is damage to the dura, it is usually due to the surgeon putting too much pressure on the tip. Holding the handpiece more gently and applying less force will likely fix this problem. If the surgeon is forcibly scraping the tip on the bone, it will cause a break in the thin bone and damage the skull. Finally, if after thinning the bone, the underlying dura appears bruised, it is likely due to excess heat from the vibrations. Increasing the rate of ACSF flow will fix this issue.
The main limitation of PHASOR is that the handpiece can thin the bone, but cannot remove all the bone over the dura. The diamond coated tip has small rough bumps. The rubbing needed to thin the skull would abrade the dura and cause bleeding if it were used to remove all the bone. Thus, the use of forceps is required to remove the remaining thin layer. While there is ongoing debate on whether imaging through a thin skull produces less inflammation and less proliferation of microglia and reactive astrocytes, in some cases a window with no bone remaining is preferred, e.g., to provide a greater depth of imaging3.
We have optimized cranial window preparation for multiphoton imaging in mice. PHASOR is, to our knowledge, the first application of piezoelectric technique to rodent cranial window surgery for optical imaging. We find that the use of piezoelectric surgery in mice shares the advantages of increased speed and decreased adverse events also reported in humans7,8,9,10. Utilization of the piezoelectric device resulted in faster surgeries (Figure 2A) and fewer adverse events of bleeding when compared to a high-speed rotary drill (Figure 2B). We also found, within our lab, that PHASOR was easier for new surgeons to learn than traditional approaches to cranial window surgery. Advantages of speed and ease of use are likely to differ among surgeons. Thin skull preparations typically require 30-45 min to thin the bone with a drill and scalpel2, while the PHASOR approach typically requires less than 10 min.
We found that in windows prepared with PHASOR we could image calcium transients in layer 4 pyramidal neurons in motor cortex that had been transfected with adeno associated virus encoding the calcium indicator JRGECO1a (AAV9.Syn.NES-jRGECO1a.WPRE.SV40). We also found that, compared to a thin skull cranial window prepared with a rotary drill and scalpel, the imaging region was larger, while a thin skull prepared with a rotary drill and scalpel has an imaging window of 20 µm diameter2. With PHASOR, we were able to quickly thin an area of 3-4 mm. This is similar to the imaging window reported with PoRTS4. This larger window retains the benefit of rapid imaging reported for thin skull windows prepared with a dental drill and scalpel. Moreover, the window prepared with PHASOR can be immediately imaged, as opposed to traditional bone removal windows that may require weeks to heal before the window can be optimally imaged3.
This technique can be applied to study alterations in blood flow in the vessels under the dura. An important future study is to compare immunoreactivity of PHASOR with other methods of cranial window. This would be important to determine if PHASOR produces less inflammation in comparison to existing methods. We hope that the piezoelectric surgical technique documented here will allow more labs to perform cranial windows and successfully use multiphoton imaging in vivo.
Make sure that the handpiece is set to vibrate on the lowest setting and that the ACSF is being irrigated at a constant rate. The ice cold ACSF must be applied constantly or it will heat up and damage the dura. We found that ACSF must be applied at a rate of at least 1 mL/min. Either use a syringe held in the hand, or use a peristaltic pump, rather than the built-in irrigation in the handpiece. The irrigation system in the handpiece ejects ACSF too forcefully and produces too much turbulence, which will significantly impair visibility.
Disclosures
There are no disclosures.
Acknowledgements
Tamara Zeric for helping to obtain the multiphoton image in this paper. Supported by the Brain & Behavior, Parkinson's and JPB Foundations, R01 MH108186 and R01 DA07418. F31 fellowship 1F31MH109293-01A1 to S C.
Materials
| Name | Company | Catalog Number | Comments |
| Piezosurgery Touch | Mectron | 5120062 | Piezosurgery GP model has the same settings |
| Circular 4mm flat piezosurgery tip (# OT11) | Mectron | 3370019 | This tip was ideal for our windows but there are many other tips of different sizes availible. |
| Stereotax frame | Kopf | 963 | |
| Mouse adaptor | Stoelting | 51625 | |
| Peristaltic pump for irrigation. | Cole-Parmer | WU-77120-42 | Makes it easier to irrigate and frees up the other hand to provide stability. Irrigation can be performed by hand with a syringe if necessary. |
| Avitene Ultrafoam | Bard-Davol | 1050020 | Important to stop any minor bleeding instantly. |
| C&B Metabond | Parkell | S380 | Much stronger than regular dental acrylic. |
| Artificial cerebro spinal fluid (ACSF) | Tocris | 3525 | |
| Puralube opthalmic ointment | Dechra | 17033-211-38 | |
| Mice | JAX | 664 | |
| Prairie Ultima multiphoton microscope | Bruker | ||
| JRGECO1a (AAV9.Syn.NES-jRGECO1a.WPRE.SV40) | UPENN Vector Core |
References
- Holtmaat, A., et al. Long-term, high-resolution imaging in the mouse neocortex through a chronic cranial window. Nat Protoc. 4, 1128-1144 (2009).
- Yang, G., Pan, F., Parkhurst, C. N., Grutzendler, J., Gan, W. Thinned-skull cranial window technique for long term imaging of the cortex in live mice. Nat protoc. 12, 213-220 (2010).
- Dorand, D. R., Barkauskas, D. S., Evans, T. A., Petrosiute, A., Huang, A. Y. Comparison of intravital thinned skull and cranial window approaches to study CNS immunobiology in the mouse cortex. Intravital. 3, e29728-1-e29728-8 (2014).
- Drew, P. J., et al. Chronic optical access through a polished and reinforced thinned skull. Nat Methods. 7, 981-984 (2010).
- Wang, J., Zhang, Y., Xu, T. H., Luo, Q. M., Zhu, D. An innovative transparent cranial window based on skull optical clearing. Laser Physics Letters. 9, (2012).
- Yang, X., et al. Skull Optical Clearing Solution for Enhancing Ultrasonic and Photoacoustic Imaging. IEEE Trans Med Imaging. 35, (2016).
- Vercellotti, T. Piezoelectric surgery in implantology: a case report--a new piezoelectric ridge expansion technique. Int J Periodontics Restorative Dent. 4, 358-365 (2000).
- Vercellotti, T., De Paoli, S., Nevins, M. The piezoelectric bony window osteotomy and sinus membrane elevation: introduction of a new technique for simplification of the sinus augmentation procedure. Int J Periodontics Restorative Dent. 6, 561-567 (2001).
- Vercellotti, T., Podesta, A. Orthodontic microsurgery: a new surgically guided technique for dental movement. Int J Periodontics Restorative Dent. 4, 325-331 (2007).
- Stubinger, S., Stricker, A., Berg, B. I. Piezoelectric surgery in implant dentistry. Clin Cosmet Investig Dent. 7, 115-124 (2015).
- Basheer, S. A., Govind, R. J., Daniel, A., Sam, G., Adarsh, V. J., Rao, A. Comparative Study of Piezoelectric and Rotary Osteotomy Technique for Third Molar Impaction. J Contemp Dent Pract. 18, 60-64 (2017).
- Pavlikova, G., et al. Piezoelectric surgery prevents brain tissue damage: an experimental study on a new rat model. Int J Oral Maxillofac Surg. 40, 840-844 (2011).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved