Method Article
Human Egg Maturity Assessment and Its Clinical Application
In This Article
Summary
We provide an outline of the clinical protocol for non-invasive assessment of human egg maturity using polarized light microscopy.
Abstract
The optimal timing of intracytoplasmic sperm injection (ICSI) is of a serious concern for fertility programs because untimely sperm entry diminishes the egg's developmental competence. Presence of the first polar body (PB) together with the meiotic spindle indicates completion of the oocyte maturation and the egg's readiness for fertilization. In clinical practice, it is customary to assume that all oocytes displaying a PB are mature metaphase (MII) oocytes. However, PB extrusion precedes the formation of the bipolar MII spindle. This asynchrony makes the mere presence of PB an unreliable marker of oocyte maturity. Noninvasive spindle imaging using polarized light microscopy (PLM) allows quick and easy inspection of whether the PB-displaying oocyte actually reassembled a meiotic spindle prior to ICSI. Here, we present a standard protocol to perform human egg maturity assessment in the clinical laboratory. We also show how to optimize the time of ICSI with respect to the oocyte's developmental stage in order to prevent premature sperm injection of late-maturing oocytes. Using this approach, even immature oocytes extruding PB in vitro can be clinically utilized. Affirmation that MII spindle is present prior to sperm injection and individual adjustment of the time of ICSI is particularly important in poor prognosis in-vitro fertilization (IVF) cycles with a low number of oocytes available for fertilization.
Introduction
To become a fertilizable haploid egg, the diploid oocyte has to extrude half of its genetic information into an adjacent cell, called the first polar body (PB), and align chromosomes in the equator of the bipolar metaphase II (MII) spindle. While PB can be clearly observed by conventional light microscopy, detection of genetic material and cytoskeletal structures typically requires invasive preparatory procedures that are incompatible with the oocyte's further use for fertility treatment. Hence, in clinical practice, the presence of the PB is regarded as a hallmark of oocyte maturity. However, live imaging of microtubule and chromosome dynamics during human oocyte maturation revealed that PB becomes visible a couple of hours before bipolar MII spindle is assembled and chromosomes are aligned1. Nevertheless, in the transmitted light, the MII arrested eggs are indistinguishable from the oocytes which just entered the process of chromosome segregation. Thus, a cohort of oocytes, classified as MII oocytes based only on the PB presence, might contain latematuring oocytes that have not yet completed their development and thus are not ready for fertilization.
The delay of oocyte maturation is likely to affect the population of poor responders with a low number of MII oocytes and a high proportion of immature oocytes collected unexpectedly in stimulated cycles2. In vivo, only a single, best-quality egg achieves maturity and becomes ovulated. In in-vitro fertilization (IVF) cycles, controlled ovarian hyperstimulation is used to recruit multiple oocytes for maturation. Gonadotropin surge triggers a resumption of the meiotic program and egg progenitors are supposed to reach the MII arrest stage within 36 hours3. However, oocytes retrieved from preovulatory follicles often constitute an assortment of PBdisplaying MII oocytes and immature oocytes, either at metaphase I (MI) or germinal vesicle stage (GV) (Figure 1). Only MII oocytes are subjected to intracytoplasmic sperm injection (ICSI) while immature oocytes are typically discarded. Yet, when cultivated in vitro, MI oocytes are commonly observed to extrude PB in vitro. Despite their general inferiority, late-maturing oocytes which spontaneously completed the first meiotic division during overnight culture have been successfully used as last resource oocytes, and live births have been reported4,5,6,7,8. Hence, the untimely injection of the sperm might be a primary reason underlying poor developmental outcomes of late-maturing oocytes reported in previous studies9,10,11.
Polarized light microscopy (PLM) combined with an image processing software allows for non-invasive visualization of the meiotic spindle in the live oocyte. The double reflection is generated by the interaction of polarized light beam with the highly ordered assembly of microtubules building the bipolar spindle. Since the polarized light is of normal intensity, the technique could be safely used in clinical settings to view the dynamics of the division apparatus11,12,13,14. The presence of the MII spindle birefringence within the oocyte has been identified as a marker of an egg's developmental competence9,15,16,17,18,19,20,21,22,23. Thus, it has been suggested that non-invasive meiotic spindle imaging could be used for egg quality control in clinical practice11,14,20.
Since the timeline for the microtubular dynamics during oocyte meiosis has been resolved1, the observed PLM pattern can be better related to the time course of MI to MII transition. Shortly after PB emission, the nascent MII spindle becomes undetectable by PLM. However, if the oocytes are kept in the culture, the birefringence signal may emerge later when the bipolar MII spindle reassembles9,10,11. Thus, in oocytes extruding a PB in vitro, the absence of the spindle might be only temporary corresponding to the physiological transition of the late-maturing oocyte from MI to MII stage. If the MII spindle signal is undetectable, sperm injection can be deferred to a later time point providing extra time for the MII spindle formation. PLM-aided optimization of ICSI time maximizes the chance of late-maturing oocytes to be clinically utilized and make a difference for poor prognosis patients9.
Below, we provide a step-by-step protocol of how to perform non-invasive spindle imaging in human oocytes. We also demonstrate how PLM can be employed to avoid the risk of premature fertilization of late-maturing oocytes.
Protocol
This protocol describes the clinical procedure which is an ‘add-on’ to standard IVF treatment. It should be performed by experienced personnel in compliance with good laboratory practice and clinical guidelines24,25. Obtaining written informed consent of from the eligible patients is recommended. This protocol was approved by the institutional Ethics Committee.
1. Egg retrieval and denudation
- Induce ovarian stimulation using conventional stimulation protocols3. Adjust the dose to individual response. When two or more follicles, visualized by ultrasound scan, reach a diameter of 18 mm, induce oocyte maturation with application of 250 μg human chorionic gonadotropin (hCG). Schedule oocyte pick-up (OPU) at 35−36 h post hCG injection.
- Collect retrieved cumulus-oocyte complexes (COCs) in CO2-independent handling medium (Table of Materials). Following a short incubation period (10−15 min) in a CO2-independent incubator, briefly (up to 30 s) expose collected COCs to hyaluronidase solution (Table of Materials). Under a stereomicroscope, mechanically remove cumulus-corona cells by gently pipetting COCs with a 200 µL filter tip.
- Using denudation micropipettes with a gradually decreasing diameter (200 µm, 180 µm and 150 µm), gently strip the oocytes from the remaining follicular cells and wash the oocytes 3x in handling medium.
- Assess the number and developmental status of the denuded oocytes according to the presence or absence of the nucleus and first PB (Figure 1).
- Check the inclusion criteria for PLM examination. Carry out an egg maturity assessment if there is (1) an unexpected poor response to conventional stimulation with fewer than 6 MII oocytes collected at OPU and (2) a history of previous fertilization failure or oocyte immaturity.
- Place GV, MI and MII oocytes into separate wells in an IVF dish, each containing 500 µL of preequilibrated CO2-dependent culture medium (Table of Materials) covered with mineral oil (Table of Materials).
- Incubate for an additional 3−4 h at 37 °C in a humidified atmosphere of 5% O2 and 6% CO2.
2. Preparation for PLM examination and subsequent ICSI
NOTE: The protocol provided here describes the PLM assessment performed using the OCTAX Polar AIDE system (Table of Materials). Alternatively, other commercially available spindle view systems can be used.
- Prepare plates for embryo cultivation.
- Depending on the number of oocytes to be examined (total of MII oocytes, and MI oocytes extruding a PB during preincubation period), prepare either a 4-well plate or a 12-well plate, fill each well with 500 µL or 30 µL of culture medium, respectively, and cover with previously equilibrated mineral oil.
- Ensure that both culture medium and mineral oil have been equilibrated in the CO2 incubator overnight. Keep the prepared dish in the CO2-dependent incubator for at least 2 h. Number the wells if necessary to track the developmental fate of individual oocytes.
- Prepare the ICSI dish.
- Use assigned plastic dish and make 5 µL droplet of prewarmed handling medium for each PB-displaying oocyte and one extra droplet for needle washing. Make an additional droplet of polyvinylpyrrolidone (PVP) solution (Table of Materials) for sperm immobilization prior to ICSI (add sperm just before ICSI) and overlay with prewarmed mineral oil.
- Keep the prepared ICSI dish in the CO2-independent incubator for at least 20 min. Number the wells if necessary to track the oocytes after ICSI.
- Prepare the PLM examination dish.
- Use assigned glass bottom dish and make 5 µL droplets of prewarmed handling medium for each PB-displaying oocyte. Overlay with prewarmed mineral oil.
- Keep the dish in the CO2-independent incubator for at least 20 min. Number the droplets if necessary to track the oocytes after PLM examination.
- Set the microscope ready for PLM examination.
- Switch the heated stage on the inverted microscope on well in advance to achieve correct warming temperature. Ensure that the settings are accurately adjusted to maintain 37 °C in the handling medium droplets in the PLM/ICSI dish during micromanipulation procedures.
- Fit the sterile holding and ICSI needle into microinjection holders and bring them into focus. Alternatively, use a hatching needle.
- Select the appropriate objective (20x and 25x are the most suitable) and ensure that the condenser is in bright field position.
- Insert green interference filter (the light turns green) and set the liquid crystal analysis slider into working position.
- Set the shutter to ~50% and adjust circular polarizer to decrease background noise.
- Set the computer ready for PLM examination.
- Launch the imaging software.
- Select Video | Video Source | polarAIDE in the video menu in the top menu bar.
- Switch to live video by going to the Video page and activate spindle and zona analysis by hitting on the icon (Supplemental Figure 1) in the video toolbar.
- Select display mode for dynamic scaling during spindle imaging: (1) red (birefringence)/green (background) combined view, or (2) white (birefringence)/and black (background) view. The dynamic scoring mode is used for autoscoring of zona pellucida.
3. Examination of egg maturity
- After the preincubation period (3−4 h), perform a PLM examination revealing the oocyte maturity status at the standard time of ICSI (39−40 h after hCG trigger).
- Transfer all oocytes into individual droplets on the PLM dish and place it under the inverted microscope prepared for spindle imaging. Remember to remove the plastic lid from the glass bottom dish before starting the examination.
- Bring the first oocyte into focus. If it is difficult to search for the cell under green light, pull out the green filter temporarily. Make sure the green filter is inserted before analysis.
- Observe the detected oocyte birefringence image (red/orange on green background) as it is computer-processed and displayed in real time on the computer screen. Remember that the signal is not visible in the eyepiece.
- If the message announcing light exposure is too low/high pops up, adjust the brightness to the suitable intensity using the microscope’s light intensity knob.
- Use a holding and ICSI needle to turn the oocyte so the PB is in the 12 o’clock position and focus to the PB.
- If the spindle birefringence is not visible at first sight in the vicinity of PB, gently turn the oocyte around each axis by slightly touching the zona pellucida to ensure the alignment of the polarized light with the array spindle fibers (Supplemental Video). Declare the absence of the MII spindle as long as the oocyte fails to show the spindle signal despite rigorous rotation.
- Based on the observed birefringence pattern, classify the oocytes into the following categories (Figure 2): (A) oocytes with bright signal of bipolar barrel-shaped MII spindle with clearly delineated boundaries and even distribution of birefringence; (B) oocytes with dysmorphic, apolar and translucent MII spindle with irregular boundaries and uneven distribution of the signal; (C) oocytes with no detectable MII spindle birefringence in ooplasm; (D) anaphase I/telophase I oocytes, showing a microtubular bridge (a connective strand between first PB and the oocyte) instead of MII spindle.
NOTE: Oocyte with detectable MII spindle signal (grade A or B) are suitable for immediate ICSI. - Take a snapshot (F9) or record video for a report and/or subsequent image analysis. Keep documentation of image pattern to reduce subjectivity of the operator.
- Move to the position of a next oocyte and repeat steps 3.6−3.9.
4. Optimizing ICSI timing
- Transfer all spindle-positive oocytes (grade A or B, step 3.8) into the ICSI dish and subject them to ICSI according to standard protocols24,25.
- If the oocytes show no detectable MII spindle signal, place the PLM dish into the CO2- independent incubator and shift the ICSI into a later time.
- Perform PLM re-examination ~2−3 h later following steps 3.3−3.9. If some oocyte(s) still lack a MII spindle, further delay ICSI for additional 1−2 h.
- Transfer all oocytes into the ICSI dish and inject them according to standard protocols24. If the PLM dish is compatible with the bending angle of the microinjection needle, perform ICSI immediately in the PLM dish after switching to a bright field mode.
- Upon ICSI, transfer oocytes to prepared plates for embryo cultivation and culture until the blastocyst stage.
Results
Polarized light microscopy makes it possible to instantly inspect whether the oocyte completed nuclear maturation and assembled MII spindle prior to ICSI. Due to its non-invasive character, it can be used to safely assess the human egg's readiness for fertilization in clinical settings11,12,13,14. Spindled oocytes are more likely to give rise to viable embryos than oocytes without a spindle9,15,16,17,18,19,20,21,22,23. Also, oocytes featuring a distinct bipolar spindle appear to have a higher developmental competence than oocytes with dysmorphic spindles9,21,22. Taken together, spindle imaging can serve as a tool to identify the oocytes with the greatest potential to be successfully fertilized, undergo preimplantation development and support full-term pregnancy9,15,16,17,18,19,20,21,22,23.
The reported incidence of the spindle varies (44−97%) reflecting the diversity of the studied population9,15,16,17,18,19,20,21,22,23,26,27,28. In vivo matured oocytes from normal responders typically show bipolar MII spindle at 40 h after hCG trigger9,18,27,29. However, in slow responders, the pool of oocytes retrieved from preovulatory follicles is affected by maturation delay9,27. Here, spindle imaging should be carried out to discriminate the oocytes arrested in the MII stage from those undergoing important maturational transition (Figure 3). We recommend the removal of follicular cells immediately upon retrieval, and the incubation of MI and MII oocytes in separate wells to be able to distinguish the In vivo matured oocytes and late-maturing oocytes extruding PB in vitro, shortly before ICSI. In case the denudation is performed just before ICSI, these two populations of oocytes are indistinguishable based on the PB appearance.
The phase-specific changes of the PLM pattern should be interpreted in the context of knowledge of the spindle dynamics during meiotic maturation. During the interkinesis, division apparatus undergoes extensive structural reorganization and PLM signal transiently disappears1,9,10,11. Thus, in developmentally delayed oocytes extruding PB in vitro, the absence of the MII spindle signal may not necessarily reflect cellular disturbance but it could indicate the oocyte's progression from MI to MII stage (Figure 3). If the sperm is injected at an unphysiological time point, the egg's developmental potential is compromised. Postponing ICSI provides late-maturing oocytes with more time to assemble an MII spindle whose presence is associated with better clinical results9,10,11. In the clinical study involving slow/poor responders, nearly 60% of initially spindle-negative oocytes developed spindle signal before PLM re-examination approximately 2 h later9. Depending on the developmental stage and overall fitness of late-maturing oocytes, the MII spindle appearance after PB extrusion typically takes 2−6 h (unpublished observation). The oocytes exhibiting a microtubule bridge (anaphase/telophase, grade D) during the first PLM examination require a longer time to develop MII spindle signal than oocytes with no visible spindle (emerging spindles, grade C). Individual adjustment of the time of ICSI to the egg's developmental stage prevents premature activation of the oocyte and results in an improved fertilization rate and successful embryo development9.
Although late-maturing oocytes extruding PB in vitro generally have a lower developmental competence than In vivo matured oocytes, the rate of embryo development is acceptable if they manage to assemble a detectable spindle prior to delayed ICSI (blastulation rate of 41.32%)9. Using this approach, even immature oocytes, which are normally rejected for fertility treatment, can be clinically utilized, produce transferable embryos, and give rise to full-term pregnancies. Evaluation of the maturational stage of each individual oocyte is especially beneficial in poor prognosis cycles yielding a small number of MII oocytes and/or after performing a rescue in vitro maturation of immature oocytes9.
Apart from egg maturity assessment, spindle imaging is also recommended prior to PB biopsy in order to avoid spindle destruction in anaphase I/telophase oocytes. In experimental embryology, visualization of the meiotic spindle is used during egg enucleation and/or spindle transfer procedure13.
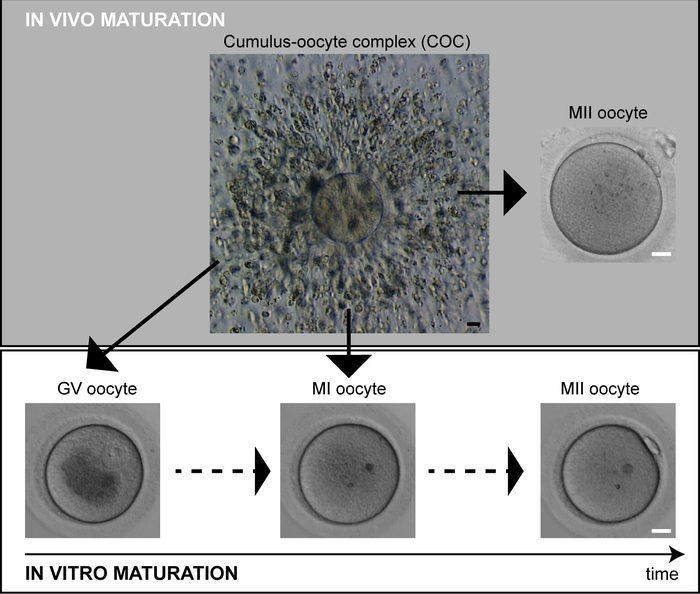
Figure 1: Human oocyte maturation. In vivo matured oocytes (MII) exhibit PB at the time of retrieval. Immature oocytes (GV, MI) can spontaneously complete maturation in vitro. Scale bar = 20 µm. Please click here to view a larger version of this figure.
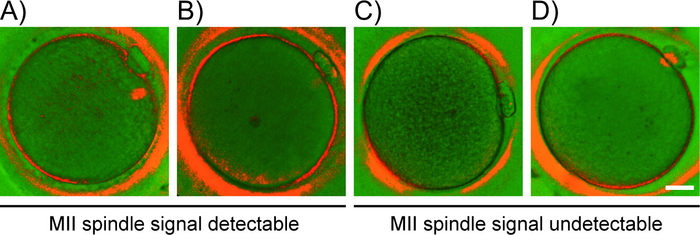
Figure 2: Oocyte classification based on PLM-detected pattern. Representative examples of oocyte grades (A-D) based on the appearance of the spindle signal. PLM-detected pattern: (A) prominent signal of bipolar spindle, (B) translucent apolar MII spindle spindle, (C) no detectable spindle, and (D) microtubule bridge. Scale bar = 20 µm. Please click here to view a larger version of this figure.
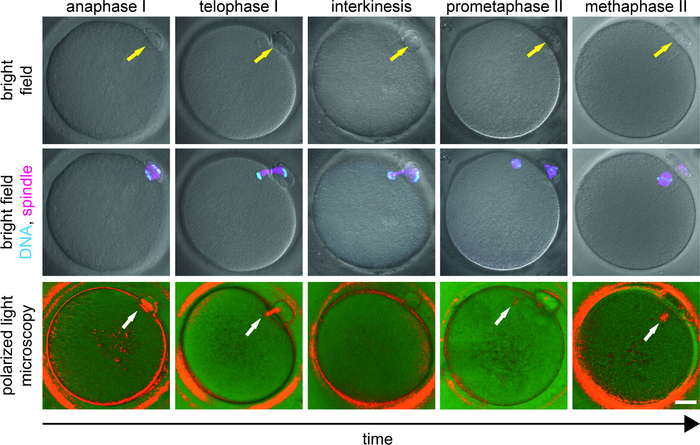
Figure 3: Stages of MI to MII transition in oocyte maturation. The appearance of oocytes in bright field (top row), combined with a fluorescence signal of chromosomes (cyan) and microtubules (magenta) (middle row), and in polarized light (bottom row) is shown. Each oocyte was first PLM-examined and immediately fixed. Fixed oocytes were (immuno)labeled with Hoechst (DNA) and anti-α-tubulin antibody (microtubules). The yellow arrow indicates the presence of PB and the white arrow highlights the position of birefringent microtubules. Scale bar = 20 µm. This figure has been modified from Holubcová et al., JARG 20199. Please click here to view a larger version of this figure.
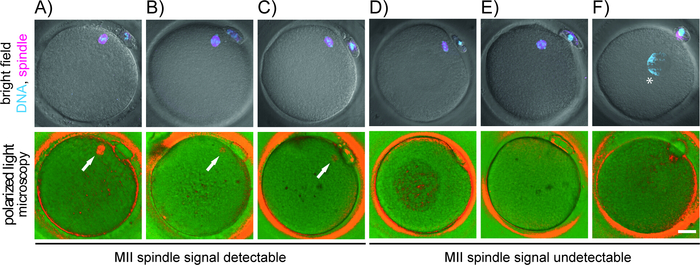
Figure 4: Correlation of chromosome-microtubule organization with birefringence pattern detected by polarized light microscopy. The appearance of oocytes in the bright field combined with a fluorescent signal for chromosomes (cyan) and microtubules (magenta) (top row), and in polarized light (bottom row) is shown. Each oocyte was fixed immediately after PLM-examination. DNA (Hoechst) and microtubule (α-tubulin) were stained. (A-C) oocytes with PLM-detectable spindle yet misaligned chromosomes (A, B) or loosely focused spindle poles (C); (D-F) abnormal oocytes without PLM-detectable MII spindle showing underdeveloped (D), apolar (E) or no spindle (F). The white arrow highlights the position of birefringent microtubules, and asterisk (*) indicates the position of decondensed chromatin. Scale bar = 20 µm. Please click here to view a larger version of this figure.
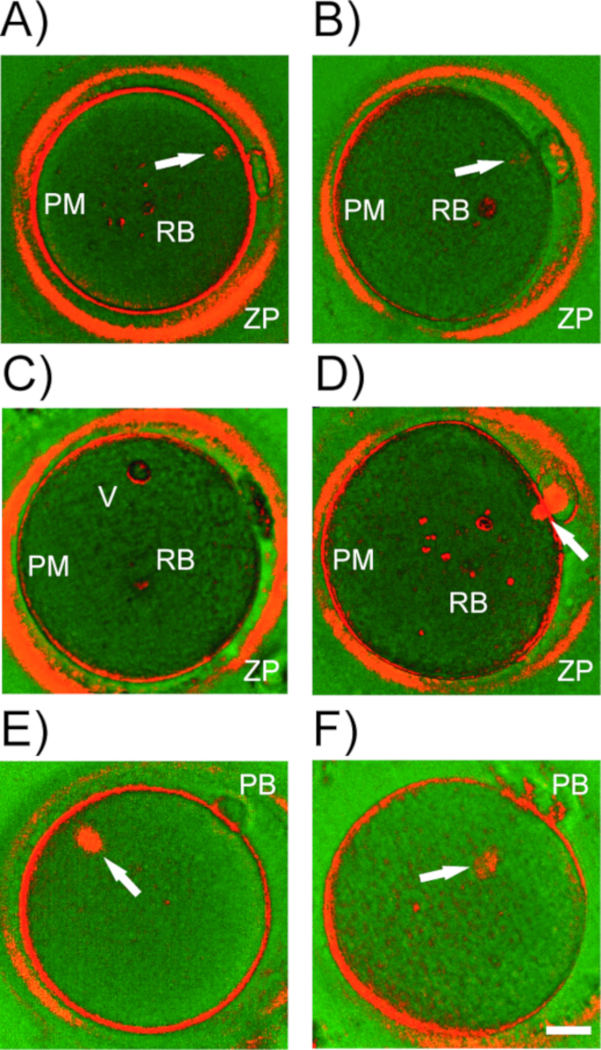
Figure 5: Birefringence structures in human oocytes. Representative examples of (A-D) birefringent structures detected by PLM in human oocytes. ZP = zona pellucida; PM = plasma membrane (oolema); RB = refractile bodies, vacuoles. White arrow, meiotic spindle in different stages of maturation. (E) MII spindle misalignment with polar body (PB). (F) Spindle detachment from plasma membrane. Scale bar = 20 µm. Please click here to view a larger version of this figure.
Supplemental Figure 1: Desktop layout of the image analysis software. Please click here to download this file.
Supplemental Video: PLM examination procedure. Rotation of the oocyte is required to exclude the presence of the spindle (arrow). Scale bar = 20 µm. Please click here to download this file.
Discussion
The acentrosomal meiotic spindle in human oocytes is highly dynamic and a delicate structure1. Under suboptimal conditions, the microtubule fibers quickly depolymerize and meiotic spindle disassembles30,31,32,33. Hence, it is critically important to ensure that the oocyte culture and micromanipulation conditions, namely temperature and pH are in the optimal range. To minimize the risk of spindle disruption, the oocytes should be kept in a temperature-controlled environment maintaining 37 ± 0.5 °C in the oocyte media. Use of microscopes and microinjection setup equipped with a heated stage is strictly required. All manipulation with oocytes outside of the incubator must be carried out in HEPES/MOPS buffered media to avoid pH fluctulations. To avoid potential adverse effects of excessive oocyte handing in ambient condition, the total time of PLM examination should not exceed 10 minutes. The oocytes have to be analyzed on the glass bottom dish with the plastic lid removed because positioning of a standard plastic in the beam path impairs image analysis. Because plastic and glass bottom dishes have different thermal characteristics, the temperature should be checked directly in the droplets of handling medium in the examination dish.
In addition to laboratory conditions, procedural differences and operator's micromanipulation skills could have an impact on PLM examination accuracy. Only highly assembled bipolar spindles can be noninvasively visualized. Observed signal is proportional to the degree of structural organization of the spindle. Nascent, apolar, loosened or disarrayed spindles display only blurred birefringence or none at all (Figure 3 and Figure 4). Besides, imperfect alignment of polarized light with microtubule arrays produces only a translucent and ill-defined birefringence despite the actual presence of welldeveloped bipolar spindle (Figure 4). Unless properly oriented, the spindle signal might be easily missed and oocyte maturity misdiagnosed (Supplemental Video). For optimal spindle imaging, the oocyte has to be properly turned around each axis. Since birefringence is not visible in eyepieces, the operator has to watch the computer screen while performing rotation of the oocyte. Previous experience with micromanipulation and training of spindle imaging in surplus in vitro matured oocytes is desirable before switching to clinical application.
Besides the spindle, the cumulus cells surrounding the oocyte, oolema, the inner layer of the zona pellucida and some cytoplasmic structures (e.g., refractile bodies, vacuoles) exhibit birefringence (Figure 5A-D). Unless thoroughly removed from the oocyte before imaging, tightly attached follicular cells produce background noise and compromise meiotic spindle detection. Be careful not to mistake a large refractile body for the spindle. Many cytoplasmic inclusions residing in the cytoplasm display high brightness which sharply contrasts with the dark background. Meiotic spindle, on the other hand, exhibit only moderate signal, blurred boundaries and typically attaches to the oolema beneath or adjacent to the first PB. Occasionally, PLM examination reveals a gross spindle deviation from its standard position (Figure 5E,F). If there is a major misalignment between the division apparatus and the PB, PLM helps to orient the oocyte to avoid the risk of spindle injury during microinjection. The relative position of the spindle within the oocyte does not appear to influence the developmental potential of the resulting embryos17,34. However, when the spindle competely detaches from the oolema, fertilization abnormalities occur. Interestingly, some poor-quality oocytes undergo chromatin decondensation immediately after PB extrusion instead of starting microtubule nucleation (Figure 4F). Using conventional light microscopy and the PB as the only marker of oocyte maturity, such sub-competent oocytes would be considered as fertilizable. Thus, on top of the routine morphological assessment, spindle imaging adds important information about the egg's maturity and can serve as an indirect marker of its quality.
The incidence of spindled MII oocytes is likely to be affected by characteristics of the study population (e.g., genetic background, medical condition, maternal age). In addition, the proportion of developmentally delayed oocytes within the cohort will influence the actual number of detected spindle-negative oocytes9,27. Meiotic spindle visualization makes it possible to clearly identify fertilizable oocytes arrested in the MII stage. Furthermore, the second inspection at a later time may reveal whether the spindle-negative oocyte is abnormal or has only recently progressed through MI/MII transition9,10,11. When allowed to develop a spindle prior to ICSI, even immature oocytes, which are routinely discarded, can produce viable embryos9. In cycles with very few oocytes available for fertilization, finely-timed ICSI of oocytes extruding PB can serve as a rescue strategy and alternative to cycle cancellation.
Nevertheless, extending the preincubation time should not be generalized to all oocytes. In vivo matured oocytes from normal responders typically exhibit an MII spindle9,20,21,27. Here, the chance of successful spindle imaging decreases with time as a consequence of post-ovulatory in vitro aging35. If possible, ICSI should be performed on the day of retrieval and should not exceed 9 hours (45 hours post hCG), the period associated with a decline in resulting embryo quality36,37. Oocytes displaying distinct bipolar spindles ought to be subjected to ICSI without further delay. In summary, individualized optimization of ICSI timing is worthwhile in poor-prognosis patients to exclude any risk of premature sperm injection. However, it is unnecessary, too time-consuming and laborious to be performed in all IVF cycles.
PLM analysis reveals whether the oocyte reached the MII stage. However, noninvasive visualization of the meiotic spindle provides no information about chromosome organization. There might be severe chromosome misalignment and/or maternal age-related chromatid splitting in oocytes featuring a bipolar spindle (Figure 5). Various other factors have significant impact on reproduction success (e.g., sperm factor, mitochondria, embryonic genome activation, irregular cleavage, epigenetics, endometrium, maternal immunity). Therefore, detection of the MII spindle per se, does not guarantee a positive clinical outcome of the IVF procedure.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We would like to thank the embryology laboratory of Reprofit International. We also acknowledge the core facility CELLIM of CEITEC supported by MEYS CR (LM2015062 Czech-Bioimaging) for their support with obtaining immunofluorescence imaging data presented here.
Materials
| Name | Company | Catalog Number | Comments |
| Continuous Single Culture Complete with Human Serum Albumin | Irvine Scientific | 90164 | bicarbonate based single-step culture medium for embryo culture |
| Denuding micropipette 150 µm | Microtech IVF | 005-150C | |
| Denuding micropipette 180 µm | Microtech IVF | 005-180B | suitable for oocyte transfer between dishes |
| Denuding micropipette 200 µm | Microtech IVF | 005-250-A | suitable for oocyte transfer between dishes |
| FluoroDish | World Precision Instruments | FD 5040-100 | glass-bottom dish |
| (alternative: WillCo-dish GWST-5040 WillCo Wells) | |||
| Holding micropipette | Microtech | 001-120-30 | sterile glass microneedles |
| Hyaluronidase solution | Irvine Scientific | 90101 | for oocyte denudation |
| ICSI micropipette | Microtech | 002-5-30 | sterile glass microneedles |
| Micro Droplet Culture Dish | Vitrolife | 16003 | 12-well plate for embryo culture |
| Multipurpose Handling Medium (MHM) with Gentamicin | Irvine Scientific | 90163 | handling medium, MOPS/HEPES buffered |
| Nikon Eclipse TE 2000-U | Nikon | inverted microscope with heated stage | |
| Nunc IVF Petri Dish, 60 mm | Thermo Fisher Scientific | 150270 | plastic ICSI dish |
| Nunc non-treated 4-well IVF dish | Thermo Fisher Scientific | 179830 | 4-well plate for embryo culture |
| OCTAX polarAide | MTG | integrated PLM system | |
| Oil for embryo culture | Irvine Scientific | 9305 | oil for overlay |
| Polyvinylpyrrolidone | Irvine Scientific | 90123 | for sperm immobilization prior to ICSI |
References
- Holubcova, Z., Blayney, M., Elder, K., Schuh, M. Human oocytes. Error-prone chromosome-mediated spindle assembly favors chromosome segregation defects in human oocytes. Science. 348 (6239), 1143-1147 (2015).
- Oudendijk, J. F., Yarde, F., Eijkemans, M. J., Broekmans, F. J., Broer, S. L. The poor responder in IVF: is the prognosis always poor?: a systematic review. Human Reproduction Update. 18 (1), 1-11 (2012).
- Gautam, N., Allahbadia, Y. M. . Ovarian Stimulation Protocols. , (2016).
- Piqueras, P., et al. Live birth after replacement of an embryo obtained from a spontaneously in vitro matured metaphase-I oocyte. Systems Biology in Reproductive Medicine. 63 (3), 209-211 (2017).
- Liu, J., Lu, G., Qian, Y., Mao, Y., Ding, W. Pregnancies and births achieved from in vitro matured oocytes retrieved from poor responders undergoing stimulation in in vitro fertilization cycles. Fertility and Sterility. 80 (2), 447-449 (2003).
- Shu, Y., et al. Fertilization, embryo development, and clinical outcome of immature oocytes from stimulated intracytoplasmic sperm injection cycles. Fertility and Sterility. 87 (5), 1022-1027 (2007).
- Sachdev, N. M., Grifo, J. A., Licciardi, F. Delayed intracytoplasmic sperm injection (ICSI) with trophectoderm biopsy and preimplantation genetic screening (PGS) show increased aneuploidy rates but can lead to live births with single thawed euploid embryo transfer (STEET). Journal of Assisted Reproduction and Genetics. 33 (11), 1501-1505 (2016).
- De Vos, A., Van de Velde, H., Joris, H., Van Steirteghem, A. In-vitro matured metaphase-I oocytes have a lower fertilization rate but similar embryo quality as mature metaphase-II oocytes after intracytoplasmic sperm injection. Human Reproduction. 14 (7), 1859-1863 (1999).
- Holubcova, Z., et al. Egg maturity assessment prior to ICSI prevents premature fertilization of late-maturing oocytes. Journal of Assisted Reproduction and Genetics. 36 (3), 445-452 (2019).
- Montag, M., Schimming, T., van der Ven, H. Spindle imaging in human oocytes: the impact of the meiotic cell cycle. Reproductive BioMedicine Online. 12 (4), 442-446 (2006).
- Montag, M., van der Ven, H. Symposium: innovative techniques in human embryo viability assessment. Oocyte assessment and embryo viability prediction: birefringence imaging. Reproductive BioMedicine Online. 17 (4), 454-460 (2008).
- Keefe, D., Liu, L., Wang, W., Silva, C. Imaging meiotic spindles by polarization light microscopy: principles and applications to IVF. Reproductive BioMedicine Online. 7 (1), 24-29 (2003).
- Caamano, J. N., Munoz, M., Diez, C., Gomez, E. Polarized light microscopy in mammalian oocytes. Reproduction in Domestic Animals. 45, 49-56 (2010).
- Eichenlaub-Ritter, U., Shen, Y., Tinneberg, H. R. Manipulation of the oocyte: possible damage to the spindle apparatus. Reproductive BioMedicine Online. 5 (2), 117-124 (2002).
- Wang, W. H., Meng, L., Hackett, R. J., Odenbourg, R., Keefe, D. L. The spindle observation and its relationship with fertilization after intracytoplasmic sperm injection in living human oocytes. Fertility and Sterility. 75 (2), 348-353 (2001).
- Wang, W. H., Meng, L., Hackett, R. J., Keefe, D. L. Developmental ability of human oocytes with or without birefringent spindles imaged by Polscope before insemination. Human Reproduction. 16 (7), 1464-1468 (2001).
- Moon, J. H., et al. Visualization of the metaphase II meiotic spindle in living human oocytes using the Polscope enables the prediction of embryonic developmental competence after ICSI. Human Reproduction. 18 (4), 817-820 (2003).
- Cohen, Y., et al. Spindle imaging: a new marker for optimal timing of ICSI?. Human Reproduction. 19 (3), 649-654 (2004).
- Rama Raju, G. A., Prakash, G. J., Krishna, K. M., Madan, K. Meiotic spindle and zona pellucida characteristics as predictors of embryonic development: a preliminary study using PolScope imaging. Reproductive BioMedicine Online. 14 (2), 166-174 (2007).
- Heindryckx, B., De Gheselle, S., Lierman, S., Gerris, J., De Sutter, P. Efficiency of polarized microscopy as a predictive tool for human oocyte quality. Human Reproduction. 26 (3), 535-544 (2011).
- Kilani, S., Cooke, S., Tilia, L., Chapman, M. Does meiotic spindle normality predict improved blastocyst development, implantation and live birth rates?. Fertility and Sterility. 96 (2), 389-393 (2011).
- Kilani, S., Chapman, M. G. Meiotic spindle normality predicts live birth in patients with recurrent in vitro fertilization failure. Fertility and Sterility. 101 (2), 403-406 (2014).
- Tilia, L., Venetis, C., Kilani, S., Cooke, S., Chapman, M. Is oocyte meiotic spindle morphology associated with embryo ploidy? A prospective cohort study. Fertility and Sterility. 105 (4), 1085-1092 (2016).
- ESHRE Guideline Group on Good Practice in IVF Labs, De los Santos, M. J., et al. Revised guidelines for good practice in IVF laboratories (2015). Human Reproduction. 31 (4), 685-686 (2016).
- Montag, M., Morbeck, D. . Principles of IVF Laboratory Practice: Optimizing Performance and Outcomes. , (2017).
- Chamayou, S., et al. Meiotic spindle presence and oocyte morphology do not predict clinical ICSI outcomes: a study of 967 transferred embryos. Reproductive BioMedicine Online. 13 (5), 661-667 (2006).
- Rienzi, L., et al. Relationship between meiotic spindle location with regard to the polar body position and oocyte developmental potential after ICSI. Human Reproduction. 18 (6), 1289-1293 (2003).
- Woodward, B. J., Montgomery, S. J., Hartshorne, G. M., Campbell, K. H., Kennedy, R. Spindle position assessment prior to ICSI does not benefit fertilization or early embryo quality. Reproductive BioMedicine Online. 16 (2), 232-238 (2008).
- Kilani, S., Cooke, S., Chapman, M. Time course of meiotic spindle development in MII oocytes. Zygote. 19 (1), 55-62 (2011).
- Wang, W. H., Meng, L., Hackett, R. J., Odenbourg, R., Keefe, D. L. Limited recovery of meiotic spindles in living human oocytes after cooling-rewarming observed using polarized light microscopy. Human Reproduction. 16 (11), 2374-2378 (2001).
- Sun, X. F., Wang, W. H., Keefe, D. L. Overheating is detrimental to meiotic spindles within in vitro matured human oocytes. Zygote. 12 (1), 65-70 (2004).
- Mullen, S. F., et al. The effect of osmotic stress on the metaphase II spindle of human oocytes, and the relevance to cryopreservation. Human Reproduction. 19 (5), 1148-1154 (2004).
- Swearman, H., et al. pH: the silent variable significantly impacting meiotic spindle assembly in mouse oocytes. Reproductive BioMedicine Online. 37 (3), 279-290 (2018).
- Rienzi, L., Vajta, G., Ubaldi, F. Predictive value of oocyte morphology in human IVF: a systematic review of the literature. Human Reproduction Update. 17 (1), 34-45 (2011).
- Miao, Y. L., Kikuchi, K., Sun, Q. Y., Schatten, H. Oocyte aging: cellular and molecular changes, developmental potential and reversal possibility. Human Reproduction Update. 15 (5), 573-585 (2009).
- Pujol, A., Garcia, D., Obradors, A., Rodriguez, A., Vassena, R. Is there a relation between the time to ICSI and the reproductive outcomes?. Human Reproduction. 33 (5), 797-806 (2018).
- Yanagida, K., et al. Influence of oocyte preincubation time on fertilization after intracytoplasmic sperm injection. Human Reproduction. 13 (8), 2223-2226 (1998).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved