Method Article
Robotic Pancreatoduodenectomy for Pancreatic Head Cancer: a Case Report of a Standardized Technique
* These authors contributed equally
In This Article
Summary
Robotic pancreatoduodenctomy (RPD) has been highly standardized in recent years and may be used in selected patients with pancreatic head cancer, including those with a replaced right hepatic artery. This case report describes a standardized and reproducible technique for RPD, which includes the approach of the Dutch LAELAPS-3 training program to an aberrant vasculature.
Abstract
Robotic pancreatoduodenectomy (RPD) for pancreatic cancer is a challenging procedure. Aberrant vasculature may increase the technical difficulty. Several studies have described the safety of RPD in case of a replaced or aberrant right hepatic artery, but detailed video descriptions of the approach are lacking. This case report describes a step-by-step technical video in case of a replaced right hepatic artery. A 58-year-old woman presented with an incidental finding of a 1.7 cm pancreatic head mass. RPD was performed using the da Vinci Xi system and involves a robotic-assisted pancreatico- and hepatico-jejunostomy and open gastro-jejunostomy at the specimen extraction site. The operation time was 410 min with 220 mL of blood loss. The patient had an uncomplicated postoperative course and was discharged after 5 days. Pathology revealed a pancreatic head cancer. RPD is a feasible and safe procedure in case of a replaced hepatic artery when performed in selected patients in high-volume centers by experienced surgeons.
Introduction
The combination of surgery and systemic therapy provides the most effective way of prolonging life expectancy in patients with resectable pancreatic cancer1. In recent years, interest in minimally invasive pancreatoduodenectomy has increased, aiming to decrease the impact of surgery and thereby enhancing postoperative recovery2.
Robotic pancreatoduodenectomy (RPD) aims to overcome compromises made by laparoscopy, by the ability of wrist movements, scaled down movements, and enhanced 3D vision combined with benefits of the minimally invasive approach for more precision and improved surgical ability. RPD is associated with a learning curve3,4; an experienced single center study reported that the learning curve based on operative time was overcome after 80 RPD procedures5. A dedicated training program can have a positive impact on this learning curve6. The University of Pittsburgh Medical Center (UPMC) group found improved outcomes after the implementation of a training program for RPD5. In the Netherlands, the LAELAPS-3 multicenter training program for RPD was started by the Dutch Pancreatic Cancer Group (DPCG) in collaboration with the UPMC team and demonstrated good results, including a learning curve based on operative time that was overcome after 22 RPD procedures7. Currently, this is being followed by the European LEARNBOT multicenter training program for RPD.
Aberrant hepatic vasculature is present in 15-20% of patients undergoing RPD, most commonly a replaced right hepatic artery, which may complicate the resection phase8. Currently, specific teaching material for RPD in patients with a replaced right hepatic artery is lacking. Detailed descriptions are crucial to prepare an optimal surgical strategy, also highlighting the importance of preoperative imaging for detecting any aberrant vasculature. The safety of RPD with aberrant hepatic vasculature was confirmed by several studies as long as these procedures are performed by specifically trained and experienced surgeons, working in high volume centers6,8,9,10,11,12.
This case report describes and shows a step-by-step technical approach to RPD in case of a replaced right hepatic artery performed in the Netherlands, aimed to facilitate ongoing (i.e., LEARNBOT) and future training programs. The Amsterdam UMC currently performs >40 RPD procedures per year and therefore conforms to the Miami guidelines volume cut-off of >20 RPD procedures2, as do all Dutch centers that participated in the LAELAPS-3 program. The described technique was standardized after 32 procedures (since November 2019) and a total of 115 procedures have been performed (until February 2022).
The described approach is reproducible and compatible for both normal and aberrant anatomy and includes additional steps for a replaced right hepatic artery.
A 58-year-old woman presented with an incidental finding of a 1.7 cm pancreatic head mass suspect for pancreatic ductal adenocarcinoma. No distant metastases and lymph node involvement was identified on the preoperative CT-scan. However, the CT-scan revealed a replaced right hepatic artery originating from the superior mesenteric artery (SMA) (Figure 1). Patient had a history of cholecystectomy, body mass index 30 kg/m2, and was ASA 1. The pancreatic duct measured 3 mm at the neck of the pancreas, and the hepatic duct measured 7 mm at the intended transection plane. The patient did not receive neoadjuvant chemotherapy, as no definitive preoperative histological diagnosis of pancreatic ductal adenocarcinoma could be made. The patient appeared suitable for a minimally invasive approach.
Protocol
The present protocol follows the ethics guidelines of the Amsterdam UMC. Written and oral consent was obtained from the patient to use her medical data and operative video for publication of this article. A copy of written consent is available for review by the Editor-in-Chief of this journal.
1. Preoperative work-up
- Evaluate the CT scan for the extent of the tumor and check for any aberrant vasculature and determine a surgical approach accordingly.
- Check for the relative contraindications for RPD, such as a BMI >35 kg/m2 and tumor involvement in the portal vein or superior mesenteric vein requiring vascular reconstruction and previous major abdominal surgery with possible adhesions.
NOTE: It is possible to perform a vascular reconstruction during RPD, once the surgical team has sufficient experience (i.e., experience >80-100 RPDs).
2. Installation
NOTE: The procedure is performed by two experienced surgeons: the console surgeon and the tableside surgeon. These two surgeons may swap positions after the resection phase has been completed. Alternatively, some centers report an approach where the tableside surgeon is replaced by an experienced surgical fellow, resident or scrub nurse. The advice is to complete the full learning curve with a two-surgeon approach.
- Patient positioning
- Place the patient in a supine 20° reverse Trendelenburg position with 20° left-tilt, right arm lowered on an arm board and left arm abducted. Part the lower limbs in the French position with the left leg horizontal to facilitate the tableside surgeon's position.
- Position the compression stockings, sequential compression device, warming device for legs and a urinary catheter.
- Surgeon position
- Apply chlorohexidine and create a sterile exposition.
- Position the first surgeon between the patient's legs and the second surgeon at the left side and the assistant at the right side of the patient.
- Pneumoperitoneum and trocar measurement
- Start the procedure laparoscopically.
- Place a Veress needle at the Palmer's point to induce a CO2 pneumoperitoneum pressure up to 10-12 mmHg.
- Measure and mark the position of the robot and tableside surgeon trocars. Mark the camera port 11-12 cm from the costal margin towards a position 2-3 cm to the right of the umbilicus (Figure 2).
- Mark the vision port and second 12 mm port position 7 cm away from the camera port.
- Mark a robotic port 7 cm to the left of the camera port in the left midclavicular line (arm 4) and a robotic port 7 cm to the right of the camera port in the right midclavicular line (arm 2).
- Mark the robot port for arm 1, 7 cm cranio-lateral from the arm 2 trocar.
- Port placement
- Place the vision port, second 12 mm port and all 4 robotic ports on the marked locations.
- Place a 5 mm port in the left upper quadrant, through which an angulated (45°) snake liver retractor is placed under liver segment 3-4.
- Optionally, retract the Teres ligament cranially using a percutaneous straight needle.
- Diagnostic laparoscopy and initial mobilization
- Perform a full diagnostic laparoscopy for metastases.
3. Resection
NOTE: The sequence of instruments during each operative step is seen in Table 1.
- Ligament of Treitz
- Cranialize the greater omentum and colon.
- Dissect the left side of the ligament of Treitz to free the most distal part of the duodenum and the first part of the jejunum from the aorta.
- Mobilization ascending colon
- Dissect along the greater curvature towards the pylorus and fully mobilize the ascending colon and the hepatic flexure to facilitate safe uncinate dissection.
- Dissect the gastrocolic ligament.
- Docking
- Position and dock the robot over the right shoulder of the patient to the previously positioned trocars. Robot arm 1 is equipped with cadiere forceps, arm 2 is equipped with fenestrated bipolar forceps, arm 3 is equipped with the camera, and arm 4 is equipped with cautery hook. The tableside surgeon is equipped with a blunt tip vessel sealing device.
NOTE: If the entire operating table is rotated 45° with the patient's legs to the left in the operating room, the robot can enter cranially over the right shoulder to provide sufficient space for the 3D-screen next to the robot and provide space for the scrub nurse with a table. In this way the tableside surgeon can comfortably use the 3D screen with limited neck rotation.
- Position and dock the robot over the right shoulder of the patient to the previously positioned trocars. Robot arm 1 is equipped with cadiere forceps, arm 2 is equipped with fenestrated bipolar forceps, arm 3 is equipped with the camera, and arm 4 is equipped with cautery hook. The tableside surgeon is equipped with a blunt tip vessel sealing device.
- Omental bursa (Lesser sac)
- Retract the stomach cranially.
- Open the omental bursa (lesser sac) by dividing the gastrocolic ligament approximately 2 cm below the gastroepiploic pedicle.
- Continue the mobilization towards the hepatic flexure.
- Kocher maneuver
- Kocher until the left renal vein, while arm 1 is retracting the stomach and duodenum to the patients' left.
- Retract the proximal jejunum through the ligament of Treitz defect into the right supracolic upper quadrant (creation of the jejunal loop for the reconstruction phase).
NOTE: Be careful of tearing the branches of the SMV due to traction from the duodenum. The traction can be minimized by retracting the colon to the patients' left.
- Transection of the proximal jejunum
- Transect the jejunum approximately 10 cm distally from the pancreas with a 60 mm vascular linear stapler.
- Linearization of the duodenum
- Mobilize the duodenum until the pancreatic head with a blunt tip vessel sealing device.
- Dissection and transection of right gastric artery (RGA)
- Mobilize, clip, and transected the right gastric artery using a blunt tip vessel sealing device.
- Transection of the distal stomach
- Skeletonize the distal stomach just before the pylorus.
- Retract the nasogastric tube 10 cm and transect the stomach 1-2 cm proximal to the pylorus with a 60 mm thick linear stapler.
- Portal dissection
- Start the portal dissection with arm 1 retracting the staple line to the right lower quadrant.
- Hepatic artery lymph node (8a)
- Identify lymph node station 8a (hepatic artery lymph node), mobilize, extract in an extraction bag (alternatively: cut finger of surgical glove), and send to pathology.
- Mobilize the common hepatic artery.
- Skeletonization of gastroduodenal artery (GDA) and replaced right hepatic artery
- Skeletonize the replaced right hepatic artery and GDA. Place vessel loops around both vessels and fixate with clips as a means of retraction as shown in Figure 3.
- Rotate the specimen to the patients' left so the hepato-duodenal ligament can be visualized from the right side. Lift the neck of the gallbladder using robot arm 1 and mobilize the replaced right hepatic artery. Place vessel loops and fixate with clips.
- Dissection and transection of the common hepatic duct
- Dissect and transect the biliary system. Then transect the common hepatic duct with cold scissors between bulldogs (alternatively stapled using a vascular cartridge).
- Transection of GDA
- After the arterial anatomy has been confirmed, test-clamp the GDA and transect.
- Transect using a 60 mm vascular linear stapler and place two additional metal clips at the hepatic artery side.
- Exposure of the pancreas and superior mesenteric vein.
- Expose the lower border of the pancreas
- Tunneling the pancreas
- Create a wide tunnel under pancreas, tunneling the pancreas using a blunt tip vessel sealing device.
- Pancreatic transection
- Circle the pancreas with a vessel loop, fixate with a clip, and retract cranially with arm 1.
- Transect the pancreas with diathermic scissors but be careful not to close the pancreatic duct with the diathermia.
- Identification of pancreatic duct
- Identify pancreatic duct for 'cold' transection and hemostasis.
- Using the scissors bluntly, carefully mobilize the porto-mesenteric vein away from the pancreatic head to expose the 'mesopancreas'.
- Uncinate process
- Dissect in the following three phases.
- Venous mobilization
- Mobilize the entire ventral side of superior mesenteric vein from the pancreatic neck down to the uncinate process using a diathermia hook on robot arm 4.
NOTE: Take care of the right gastro-epiploic vein and (potentially) the right colonic vein.
- Mobilize the entire ventral side of superior mesenteric vein from the pancreatic neck down to the uncinate process using a diathermia hook on robot arm 4.
- Transection of the right gastro-epiploic vein
- Clip the right gastro-epiploic vein and transect between the clips using a blunt tip vessel sealing device.
- Dissection along the SMA
- Use robot arm 1 to retract the duodenum close to the uncinate process to the patients right lower quadrant.
- Dissect between the pancreatic head and the superior mesenteric artery using a blunt tip vessel sealing device.
- Identify the origin of the inferior pancreaticoduodenal artery and secure with (metal) clip(s) before transecting with a blunt tip vessel sealing device.
NOTE: Take care not to damage the first jejunal venous branch.
- Dissection along the right hepatic artery
- Further dissect the pancreatic head by dissecting proximally with a blunt tip vessel sealing device along superior mesenteric vein and portal vein.
- Transect any venous branches originating from the pancreatic head. Identify and clip the superior lateral pancreaticoduodenal vein (Belcher's vein) before transecting with a blunt tip vessel sealing device.
NOTE: In case of a replaced right hepatic artery, the inferior and superior pancreaticoduodenal artery can have anatomical variations.
- Lymphadenectomy and endobag
NOTE: Because this patient has a replaced right hepatic artery the lymph nodes behind the portal vein and right hepatic artery may have to be dissected separately.- Place the specimen (and lymph nodes if applicable) in a large endobag.
- Place the endobag in the right lower quadrant.
- Cholecystectomy (if applicable)
NOTE: This patient had a history of cholecystectomy; otherwise cholecystectomy is performed as the final part of the dissection phase.- Place the gallbladder in a separate endobag and place this (smaller) endobag on top of the liver.
NOTE: Cholecystectomy is a good procedure for an experienced surgical resident or fellow who completed basic robot training previously.
- Place the gallbladder in a separate endobag and place this (smaller) endobag on top of the liver.
4. Reconstruction
- Drain placement
- Place a surgical drain fully in the abdomen.
- Position the drain (#1) through Winslow, and retract far to the left, with the end of the drain under the endobag.
NOTE: After completion of the pancreatic and bile duct anastomoses, this drain's end section will be extracted via the robot port for arm 1, such that it drains both anastomoses.
- Pancreatico- and hepatico-jejunostomy
- Equip robotic arm 1 with cadiere forceps.
- Equip robotic arm 2 with large needle driver with suture cut.
- Equip robotic arm 4 with large needle driver and switch to monopolar curved scissors for both enterotomies.
- Set up the jejunal loop.
- Pancreatico-jejunostomy (PJ)
- Perform the PJ in a two-layer, end to side, duct-to-mucosa method, according to the modified Blumgart technique.
- Mattrass
- Place three 2-0 18 cm silk mattress sutures. Drive the 2-0 silk suture at the cranial side of the pancreas through the entire pancreas, approximately 1 cm from the cut margin.
- Drive the suture through the jejunum from a cranial to caudal position. Drive the needle back through the pancreas towards the anterior plane and hold both ends with arm 1.
- Repeat this at the central position of the pancreas around the pancreatic duct and hold with arm 1.
- Lastly repeat this at the caudal position of the pancreas.
- Tie the suture at the caudal position of the pancreas.
- Put a 7 French 6 cm single loop urology stent in the pancreatic duct. Tie the suture at the central position of the pancreas and remove stent after tying.
NOTE: Be gentle to avoid suturing the pancreatic duct. - Lastly tie the suture at the cranial side of the pancreas and leave all the needles on the sutures.
- Duct-to-mucosa (DTM)
- Perform enterotomy with diathermic scissors on arm 4.
- Place 3 to 5 posterior wall 5-0 (polydioxanone) PDS 8 cm duct-to-mucosa sutures, starting with the 8 o'clock position. Retract both ends with arm 1.
- Replace the pancreatic duct stent. This can be used to prevent accidental closing of the duct with anterior sutures in case of a narrow pancreatic duct.
- Now place 3-5 anterior 5-0 PDS 8 cm sutures, initially without tying to allow for optimal view on the (often narrow) duct.
- After placing, tie all PDS sutures.
- Buttress
- Reuse the same three silk needles, previously used for the posterior layer, for the anterior layer of the PJ.
- Drive the suture through the jejunum in an oblique direction in the corners and in a lateral direction in the middle and tie these to complete the anastomosis.
NOTE: It is essential that the jejunum "overlaps" on the pancreas.
- Hepatico-jejunostomy (HJ)
- Create a loop of about 10 cm between PJ and HJ.
- Using diathermic scissors on arm 4, open the bowel antimesenteric.
- Perform a single layer anastomosis using 8 to 10 interrupted 5-0 PDS 8 cm sutures or two running 4-0 barbed 15 cm sutures. Both techniques are described below.
- Running technique
- Use monopolar curved scissors to perform the enterotomy.
- Anchor the first barbed suture at the 7 o'clock position (bile duct inside-out). Run the suture twice when anchoring because of the lack of hooks in the first cm of the suture.
- Anchor the second barbed suture at the 9 o'clock position (bile duct outside-in), again twice, and hang with arm 1.
- Run the suture for the posterior row towards the 3 o'clock position.
- Run the suture for the posterior row towards the 3 o'clock position.
- Tie the two barbed sutures to complete the anastomosis.
- Place a gauze on the HJ anastomosis to check for possible bile leakage.
NOTE: Only use barbed sutures for a thick bile duct wall to prevent perforation due to the hooks.
- Interrupted technique
- Start with placing the posterior sutures.
- Start at the posterior row at the 6 o'clock position and tie, then place 2 sutures on either side and tie.
- Place the sutures in the corners and tie.
- Place and tie the sutures on the anterior row to complete the anastomosis.
- Place gauze on the HJ anastomosis to check for possible bile leakage.
NOTE: In case of a thin bile duct wall a stay suture may be placed between the jejunum and the gallbladder bed.
- Gastrojejunostomy (GJ) preparation
- Introduce one end of a 60 cm long barbed suture (with needle), and grab with arm 1 at the lever of the HJ.
- Use robot arms 2 and 4 and 'walk' 60 cm on the bowel together with the suture.
- Place two 3-0 silk marking stitches on the jejunum to mark the correct bowel position for the GJ: double end on the proximal side ('double = duodenum') and a single just distal.
- Reflect the omentum and mesocolon cephalad by the laparoscopic assistant and locate the jejunal loop and both sutures.
- Position the loop next to the stomach, which is held by arm 1, with the double end suture to the left.
- Suture this loop to the posterior surface of the stapled end of the stomach with stay sutures.
- Drain extraction
- Check the gauze on HJ for bile leakage and remove.
- Remove robot arm 1. Extract the end-section of the earlier placed drain #1 using a laparoscopic grasper and fixate on the skin.
- Ligament patch and laparoscopic graspers
- Mobilize and position the round ligament on top of the portal vein, between the gastroduodenal artery (GDA) stump and the PJ.
- Secure both ends of the endobag with clips and grab this and the gastro-jejunostomy location with two laparoscopic graspers.
- Remove the liver retractor.
- Undocking
- Undock the robot from the trocars and remove the robot from the operating table.
- Gastrojejunostomy and specimen extraction
- Make a muscle-sparing transverse incision in the left upper quadrant from the 5 mm trocar to medial, through the rectus sheath.
- Introduce a medium hand port and extract both endobags.
- Extract the gastrojejunostomy site.
- Perform a single-layer gastrojejunostomy (GJ) with running PDS 3-0 sutures. This is a child type anastomosis.
- Enterotomy and GJ anastomosis
- Remove staple lines on the stomach side and perform enterotomy on the jejunum.
- Suture the posterior and anterior walls of the anastomosis in a running fashion.
- Efferent marking
- Inject 2 mL of tattoo-blue in the efferent limb of jejunum to facilitate endoscopic placement of a naso-jejunal feeding tube ('blue is for you'), if needed.
- Perform the GJ through the transverse, muscle sparing, incision.
NOTE: The GJ is a hand sewn, antecolic, end-to-side anastomosis.
5. Closure
- Extraction site closure
- Close the fascia in two layers, using two single needle PDS 2-0 sutures.
- Drain placement #2
- Re-insufflate and check GJ anastomosis laparoscopically. Remove any fluid using suction.
- Place drain #2 through robot trocar 4 until under liver segment 3 and fixate.
- Trocar site closure
- Close the fascia of all 12 mm trocar sites and skin intracutaneously.
6. Post-operative management
- Close the nasogastric tube at 06:00 h the next morning. If retention is <200 mL, remove after 4 h and start with a soft liquid diet for 72 h.
- Assess drain amylase on day one and three and serum CRP on day three and four.
- Start supervised walking on the first postoperative day.
- Perform a CT abdomen if CRP does not decrease between day three and four with at least 10%.
- Discharge patients once all medical or surgical complications have been completely managed.
- Remove drains when amylase is less than three times the upper limit of normal serum amylase and the production is less than 250 mL/24 hours.
Results
During routine work-up, the pancreatic CT-scan revealed a replaced right hepatic artery originating from the superior mesenteric artery (SMA) (Figure 1). Vessel loops used in the hepatic ligament, including the replaced right hepatic artery, are shown in Figure 3.
The sequence of instruments during each operative step are shown in Table 1 and specified in the Table of Materials.
Representative results are shown in Table 2. The operation time was 410 min (including 15 min break between the resection and anastomotic phase) with 220 mL of measured intraoperative blood loss. The postoperative course was unremarkable, with a total postoperative hospital stay of five days without complications. Oral intake was possible after two days with normal diet at day four. Patient started walking on the first postoperative day and expanded this to 200 m on day three. On the early morning of postoperative day three, drain amylase was low (86 U/L)and the drain was removed. The patient was discharged two days later on postoperative day five.
Pathology assessment revealed a 1.7 cm adenocarcinoma of the head cancer. The resection margins were microscopically radical (R0) with >3 mm margin and five of 17 retrieved lymph nodes were positive for tumor. Patient started with adjuvant chemotherapy capecitabine as part of a randomized trial.
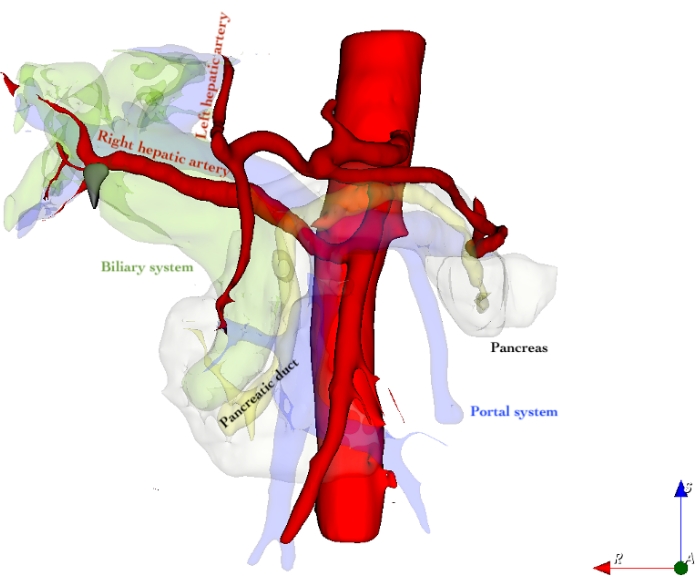
Figure 1: 3D reconstruction of hepatic vasculature including replaced right hepatic artery Please click here to view a larger version of this figure.
Red: Arterial system
Translucent yellow: Pancreatic duct
Translucent green: Biliary system
Translucent blue/purple: Portal system
Translucent white: Pancreatic tissue
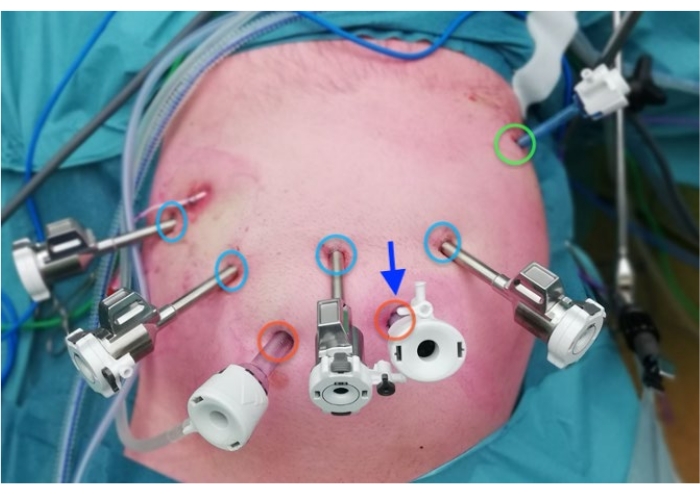
Figure 2: Port placement Please click here to view a larger version of this figure.
Blue: 8 mm robotic ports
Red: 12 mm laparoscopic ports
Green: 5 mm port for liver retractor
Arrow: Umbilicus
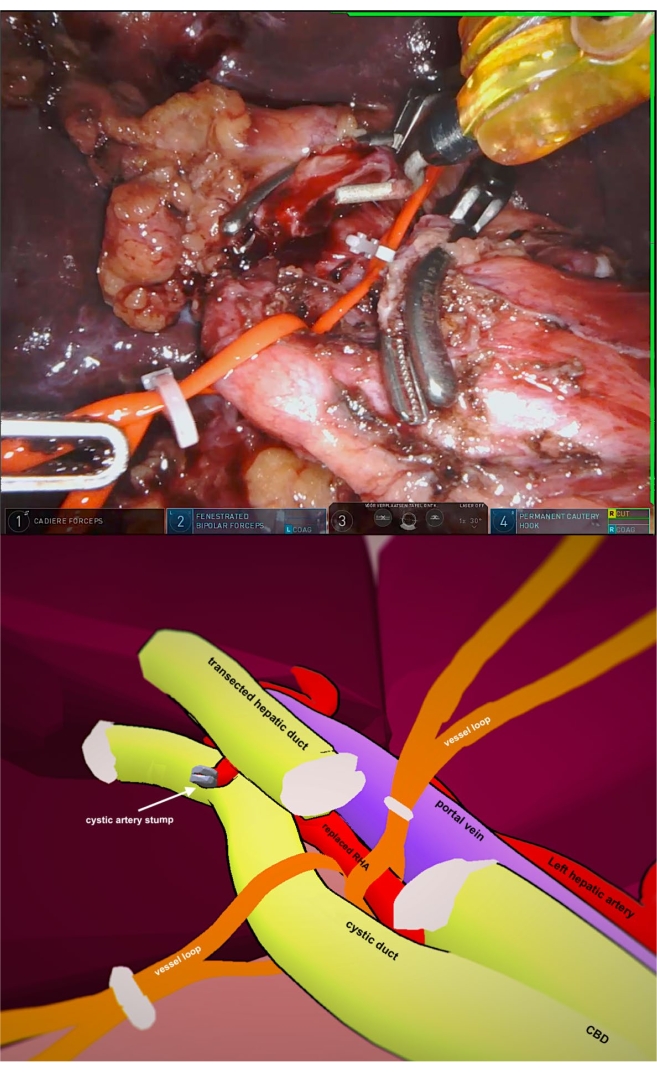
Figure 3: Vessel loops hepatic ligament Please click here to view a larger version of this figure.
| Instruments Used | |||||
| Robotic | Laparoscopic | ||||
| (console surgeon) | (assistant surgeon) | ||||
| Operative steps | Arm 1 | Arm 2 | Arm 4 | ||
| 2.5 Mobilization | Cadiere forceps | Fenestrated bipolar forceps | Permanent cautery hook | Sealing device, suction, clip-applier, stapler | |
| 3.10 Portal dissection | Cadiere forceps | Fenestrated bipolar forceps | Permanent cautery hook | Sealing device, suction, clip-applier, stapler | |
| 3.17 Pancreatic neck transection | Cadiere forceps | Fenestrated bipolar forceps | Monopolar curved scissors | Sealing device, suction, clip-applier | |
| 2.18-2.23 Pancreatic head dissection | Cadiere forceps | Fenestrated bipolar forceps | Cadiere forceps | Sealing device, suction, clip-applier | |
| 4.1 Drain placement | Cadiere forceps | Fenestrated bipolar forceps | Cadiere forceps | Fenestrated grasper | |
| 4.4-4.5 PJ and HJ | PJ | Cadiere forceps | Large needle driver | Large needle driver with suture cut | Fenestrated grasper |
| HJ | Cadiere forceps | Large needle driver | Large needle driver with suture cut | Fenestrated grasper | |
| 4.10 Specimen extraction | GJ preparation | Cadiere forceps | Large needle driver | Cadiere forceps | Fenestrated grasper |
Table 1: Sequence of instruments during each operative step
| Variable | Outcome |
| Intraoperative | |
| Operative time, minutes | 410 |
| Resection, minutes | 202 |
| Reconstruction, minutes | 179 |
| Estimated intraoperative blood loss, mL | 220 |
| Postoperative | |
| Clavien-Dindo complication grade | 0 |
| Drain removal, postoperative day | 3 |
| Postoperative hospital stay, days | 5 |
| Pathological diagnosis | Adenocarcinoma of the head cancer |
| Legend: Operative time comprises steps 2.3-5.3, Resection comprises steps 3-3.25, reconstruction comprises steps 4-4.13 | |
Table 2: Representative results
Discussion
This case report shows that RPD is feasible to perform in case of a replaced right hepatic artery when performed in selected patients by trained surgeons in high-volume centers with an annual volume of at least 20 RPD procedures per center, following the Miami guidelines2. RPD combines the benefits of a minimal invasive approach with enhanced 3D vision and the use of articulating instruments and therefore the inherent possibility of wrist movements. Moreover, the large external movements of the surgeon are scaled down to limited internal movements of the "robotic hands". This improves ergonomics that results in higher precision and greater ability of the surgeon to perform technically difficult procedures in a limited space.
Aberrant vasculature, most commonly a replaced right hepatic artery, can increase the technical difficulty of the resection phase of RPD8. A replaced right hepatic artery can make it more challenging to dissect the pancreatic head and perform an adequate lymph node dissection. Damage to an aberrant hepatic artery can induce bile duct and liver ischemia13,14. The safety of RPD in patients with a replaced right hepatic artery has been shown by several studies9,10. Adequate description of the preoperative imaging is essential to identify aberrant vascularization such as a replaced hepatic artery or other arterial abnormalities such as a celiac trunk stenosis. It is crucial during surgery to identify the replaced right hepatic artery early, and to circle and retract the artery using a vessel loop to facilitate safe dissection of the pancreatic head and lymph node harvesting.
One of the limitations of the robotic approach compared to the open approach is the loss of haptic feedback2. Furthermore, the robotic approach is a more costly approach, although improved time to functional recovery and shortened hospital stay can partly compensate for this15. Lastly, no randomized trials have been conducted to date, to suggest superiority of RPD as compared to the open approach. The potential improved clinical and oncological outcomes of RPD vs OPD should be researched in future randomized trials such as in two ongoing trials in Heidelberg16 and Johns Hopkins Medical Institutes and by the European Consortium on Minimally Invasive Pancreatic Surgery (E-MIPS)4,5,17.
This case report shows a RPD for pancreatic head cancer in a patient with a replaced right hepatic artery and described the surgical technique in detail. In conclusion, RPD for pancreatic head cancer is a feasible procedure in case of a replaced right hepatic artery when performed by experienced surgeons (after overcoming the first learning phase after 22 cases7) in high volume centers, based on the Miami guidelines advice of 20 annual procedures per center per year2.
Disclosures
M.J.W Zwart, L.R. Jones and M.G. Besselink received funding from Intuitive for the European LEARNBOT training program for robotic pancreatoduodenectomy. (Grant Reference꞉ Impact of a European training program for robot pancreatoduodenectomy using a video databank, da Vinci simulator and robot biotissue anastomoses on clinical outcomes (LEARNBOT): a pan-European prospective study) and MEH received funding from Intuitive for studies on safe implementation of robot-assisted pancreatic surgery.
J.A.M.G. Tol, M. Abu Hilal, F. Daams, S. Festen and O.R. Buschhave no conflict of interest or financial ties to disclose.
Acknowledgements
We would like to acknowledge Amer Zureikat, Melissa Hogg, Olivier Saint-Marc, Ugo Boggi, and Herbert Zeh III who supported and trained us in robotic pancreatic surgery in the Dutch Pancreatic Cancer Group - LAELAPS-3 program.
Materials
| Name | Company | Catalog Number | Comments |
| Sutures: | |||
| Internal pancreatic duct stent (12cm) 4 Fr Hobbs stent | Hobbs medical | ||
| PDS, RB-1, 8cm 5-0 x6; Z320: taper point. ½ circle 13/17mm | Ethicon | Z320 | |
| Silk, SH, 18cm 2-0 x5; C016D: taper point, ½ circle 26mm | Ethicon | C016D | |
| Straight needle Monocryl | Ethicon | Y523H | For retraction lig. teres |
| Vicryl suture without needle 60cm | Ethicon | e.g. D7818 | For measuring distance HJ-G |
| V-loc L0803: taper point, ½ circle 17mm, CV-23, 15cm 4-0 | Medtronic | L0803 | In case of thick wall, dilated bile duct x2 |
| Instruments laparoscopy: | |||
| Autosuture Endo Clip applier 5 mm | Covidien | 176620 | |
| ECHELON FLEX ENDOPATH 60mm Stapler | Ethicon | Powered surgical stapler with gripping surface technology | |
| o White filling 60mm x2 (for transection of jejunum, gastroduodenal artery) | Ethicon | GST60W | |
| o Black filling 60mm (for transection of stomach) | Ethicon | GST60T | |
| Endo Catch II Pouch 15mm | Covidien | 173049 | Bag for specimen extraction. For single lymph node extractions a cut off finger surgical glove can be used. |
| LigaSure Dolphin Tip Laparoscopic Sealer/Divider | Medtronic | LS1500 | Dolphin-nose tip sealer and divider, 37 cm shaft |
| Mediflex retractor liver | Mediflex | ||
| Set of laparoscopic bulldog clamps | Aesculap | This set consists of several bulldog clamps (of different shape and size) with dedicated laparoscopic instruments to be used to apply and remove the clamps | |
| Instruments robot: | |||
| Cadiere x2 (470049) | Intuitive Surgical | 470049 | |
| Endoscope 30º (470026) | Intuitive Surgical | 470026 | |
| Fenestrated Bipolar Forceps (470205) | Intuitive Surgical | 470205 | |
| Hot Shears, Monopolar Curved Scissors (470179) | Intuitive Surgical | 470179 | |
| Large Needle Driver x 1 (470006) | Intuitive Surgical | 470006 | |
| Medium hem-o-lok Clip applier | Intuitive Surgical | 470327 | |
| Permanent Cautery Hook (470183) | Intuitive Surgical | 470183 | |
| Suture Cut Needle Driver x1 (470296) | Intuitive Surgical | 470296 | |
| Other: | |||
| Hem-o-lok Clips MLX | Weck Surgical Instuments, Teleflex Medical, Durham, NC | 544230 | Vascular clip 3mm - 10mm Size Range |
| Hem-o-lok Clips XI | Weck Surgical Instuments, Teleflex Medical, Durham, NC | 544250 | Vascular clip 7mm - 16mm Size Range |
| Medium extraction port (double ring) | |||
| Vessel loops | Omnia Drains | NVMR61 | Disposible silicon rubber stripes, typically used to tag relevant anatomical structures |
References
- Torphy, R. J., Fujiwara, Y., Schulick, R. D. Pancreatic cancer treatment: better, but a long way to go. Surgery Today. 50 (10), 1117-1125 (2020).
- Asbun, H. J., et al. The Miami International Evidence-based Guidelines on Minimally Invasive Pancreas Resection. Annals of Surgery. 271 (1), 1-14 (2020).
- Boone, B. A., et al. Assessment of Quality Outcomes for Robotic Pancreaticoduodenectomy. JAMA Surgery. 150 (5), 416 (2015).
- Cai, J., et al. Robotic Pancreaticoduodenectomy Is Associated with Decreased Clinically Relevant Pancreatic Fistulas: a Propensity-Matched Analysis. Journal of Gastrointestinal Surgery. 24 (5), 1111-1118 (2020).
- Zureikat, A. H., et al. 500 Minimally Invasive Robotic Pancreatoduodenectomies. Annals of Surgery. 273 (5), 966-972 (2019).
- Jones, L. R., et al. Robotic Pancreatoduodenectomy: Patient Selection, Volume Criteria, and Training Programs. Scandinavian Journal of Surgery. 109 (1), 29-33 (2020).
- Zwart, M. J. W., et al. Outcomes of a Multicenter Training Program in Robotic Pancreatoduodenectomy (LAELAPS-3). Annals of Surgery. 269 (2), 344-350 (2021).
- Balzan, S. M. P., et al. Prevalence of hepatic arterial variations with implications in pancreatoduodenectomy. Arquivos Brasileiros de Cirurgia Digestiva. 32 (3), 1455 (2019).
- Nguyen, T. K., et al. Robotic pancreaticoduodenectomy in the presence of aberrant or anomalous hepatic arterial anatomy: safety and oncologic outcomes. HPB. 17 (7), 594-599 (2015).
- Kim, J. H., Gonzalez-Heredia, R., Daskalaki, D., Rashdan, M., Masrur, M., Giulianotti, P. C. Totally replaced right hepatic artery in pancreaticoduodenectomy: is this anatomical condition a contraindication to minimally invasive surgery. HPB. 18 (7), 580-585 (2016).
- Lee, J. -. M., Lee, Y. -. J., Kim, C. -. W., Moon, K. -. M., Kim, M. -. W. Clinical Implications of an Aberrant Right Hepatic Artery in Patients Undergoing Pancreaticoduodenectomy. World Journal of Surgery. 33 (8), 1727-1732 (2009).
- MacKenzie, S., Kosari, K., Sielaff, T., Johnson, E. The robotic Whipple: operative strategy and technical considerations. Journal of Robotic Surgery. 5 (1), 3-9 (2011).
- Stauffer, J. A., Bridges, M. D., Turan, N., Nguyen, J. H., Martin, J. K. Aberrant right hepatic arterial anatomy and pancreaticoduodenectomy: recognition, prevalence and management. HPB. 11 (2), 161-165 (2009).
- Abdullah, S. S., et al. Anatomical variations of the hepatic artery: study of 932 cases in liver transplantation. Surgical and Radiologic Anatomy. 28 (5), 468-473 (2006).
- Kowalsky, S. J., et al. A Combination of Robotic Approach and ERAS Pathway Optimizes Outcomes and Cost for Pancreatoduodenectomy. Annals of Surgery. 269 (6), 1138-1145 (2019).
- Klotz, R., et al. Evaluation of robotic versus open partial pancreatoduodenectomy-study protocol for a randomised controlled pilot trial (EUROPA, DRKS00020407). Trials. 22 (1), 40 (2021).
- Baimas-George, M., et al. Robotic pancreaticoduodenectomy may offer improved oncologic outcomes over open surgery: a propensity-matched single-institution study. Surgical Endoscopy. 34 (8), 3644-3649 (2020).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved