A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Transtubular Endoscopic Posterolateral Decompression for L5-S1 Lumbar Lateral Disc Herniation
In This Article
Summary
Presented here is a novel technique of C-arm free transtubular posterolateral decompression for lumbar foraminal stenosis and lateral disc herniation under O-arm navigation.
Abstract
We report a novel technique for C-arm free transtubular L5 nerve decompression under CT-based navigation to reduce the radiation hazard. This procedure is performed under general anesthesia and neuromonitoring. The patient is placed in a prone position on an operating carbon table. A navigation reference frame is placed percutaneously into the contralateral sacroiliac joint or spinous process. Then, CT scan images are obtained. After instrument registration, the L5-S1 foraminal level is confirmed with a navigated probe, and the entry point is marked. Using an approximately 2 cm skin incision, the subcutaneous tissue and muscles are dissected. The navigated first dilator is aimed at the L5-S1 Kambin's triangle, and sequential dilation is performed. The 18 mm tube is used and fixed to the frame. The bone around the Kambin's triangle is removed with a navigated burr. For lateral disc herniation, the L5 nerve root is identified and retracted, and the disc fragment is removed. The navigation-guided tubular endoscopic decompression is an effective procedure. There is no radiation hazard to the surgeon or the operating room staff.
Introduction
Diagnosis and surgeries for lumbar foraminal stenosis (LFS) and lumbar lateral disc herniation (LLDH) at the L5-S1 level are challenging for spine surgeons because of this level's unique structure1. The iliac crest, broad L5 transverse process (TP), small space between the sacral ala and the L5 TP, and osteophytes make the operating window very narrow2. If the bony resection is not enough, inadequate decompression to the L5 nerve root may lead to residual symptoms. Massive bony removal causes postoperative instability. These issues limit surgeons' competencies with foraminal/extraforaminal L5 root decompression. Several reports have shown good results with minimally invasive spine surgeries, such as microscopic or endoscopic procedures in this area to decompress the L5 nerve root3,4. Recently, the use of navigation for foraminal decompression of the L5 root has been reported with good surgical outcomes5.
Fully endoscopic discectomy is becoming popular for removing lateral lumbar disc herniation6. Furthermore, microendoscopic procedures in combination with navigation can help the surgeon to decompress the L5 root with precision2. Usually, these techniques require intraoperative C-arm usage. The goal of this method is to decompress the L5 root precisely with minimum bony resection without a C-arm.
The indications for this technique are extraforaminal lumbar disc herniation and herniation/stenosis of the lateral half of the foraminal lumbar disc. The contraindications are herniation/stenosis of the medial one-third of the foraminal lumbar disc because the scope cannot reach the targeted area2.
Protocol
This study was approved by the ethics committee of Okayama Rosai Hospital (No. 305).
1. Patient history taking
- Ensure that the patient has a herniated disc that causes severe sciatica. Usually, the patient will have a history of some prodromal low back pain. They may correlate their symptoms with an episode of trauma.
- Ask the patient to describe their radiating leg pain, including its location. Also ask them about the activities that make it better or worse when LFS or LLDH is suspected.
2. Physical examination
- To determine the nerve level, check for the signs of the loss of sensation and weakness in the leg.
- Perform a range of lumbar motion tests by asking the patient to bend forward and backward.
- Check for the induction of low back pain in the patient with a herniated disc when forward bending is done.
- Elevate the patient's leg in a supine position. If the angle between the bed and the leg is less than 70° due to sciatica, this is a strong suggestion that the patient has a herniated disc, which means the straight leg raise (SLR) test is positive.
NOTE: The SLR test is very useful to distinguish between lumbar canal stenosis (SLR-) and lumbar disc herniation (SLR+).
- Perform deep tendon reflex, and check muscle weakness in the patient.
- Perform the Kemp test7. Fix the patient's opposite ilium from the side being tested with one hand in a standing position. Grab the patient's shoulder with the other hand and lead the patient to extension, ipsilateral side bending, and rotation.
NOTE: LFS is characterized by exacerbation with foraminal narrowing caused by lumbar extension (Kemp's sign)7. If the Kemp test is positive, foraminal nerve compression by disc herniation or stenosis is likely.
3. Evaluation of radiograms (XP) and magnetic resonance imaging (MRI)
- Perform anteroposterior and lateral radiography in a standing position to check lumbar deformity and spondylolisthesis. If the patient has severe deformity, spinal fusion is indicated.
- Perform functional radiography in a standing position. Check the functional radiograms to confirm lumbar instability by measuring vertebral abnormal movement (Figure 1A, B).
NOTE: If there is severe instability that indicates more than 10° or more than 3 mm slip at the L5-S1 level, L5-S1 fusion should be considered. - Perform MRI to accurately assess the nerve compression site.
- For lateral lumbar disc herniation (LLDH), take a coronal T2 weighted image to identify the location of the herniated disc (Figure 1C-E).

Figure 1: Preoperative radiograms and MRI. (A) Lateral extension radiogram, (B) Lateral flexion radiogram, (C) Parasagittal T2 weighted MRI image, (D) Coronal T2 weighted MRI image, (E) Axial T2 weighted MR imaging at the L5-S1. The arrow indicates FLDH. Please click here to view a larger version of this figure.
4. Evaluation of computed tomography (CT) and MRI-CT fusion images
- Perform CT to check if there is a calcified disc (Figure 2A, D) or foraminal osteophyte (Figure 2B, C) not by the disc.
- Take an MRI-CT fusion image to understand the exact 3D location of the herniated disc (Figure 3).

Figure 2: Preoperative CT. (A,B) Parasagittal reconstruction CT, (C) Coronal reconstruction CT, (D) Axial CT at L5-S1. The white arrows indicate calcified FLDH; a black arrow shows an osteophyte. Please click here to view a larger version of this figure.

Figure 3: CT MRI fusion images. (A) Posterior view, (B) Posterolateral view. The white arrow indicates FLDH. Please click here to view a larger version of this figure.
5. Patient positioning and neuromonitoring (NM)
- Provide general anesthesia to the patient.
- Then, place the patient in a prone position on a carbon table.
- Ensure that the patient's eyes are not compressed with a special face cover. Pay attention to the bolster position not to compress the abdomen of the patient.
- Perform neuromonitoring using a multi-modality intraoperative monitoring system that assesses spinal cord integrity and provides a warning of potential harm to critical neural pathways (Figure 4A).Transcranial motor evoked potentials (MEPs) generate a stimulus at the motor cortex.
- Use recording electrodes to measure the signals at predetermined peripheral upper and lower extremity muscle group sites.
NOTE: If neuromonitoring is used, nerve decompression is also confirmed with this. For a muscle of which the innervated nerve is decompressed adequately, the amplitude of the MCV usually increases.
- Use recording electrodes to measure the signals at predetermined peripheral upper and lower extremity muscle group sites.
6. Intraoperative CT scan and spinal navigation
- Place a navigation reference frame (RF) percutaneously into the spinous process or sacroiliac joint. Obtain intraoperative CT scan images with a mobile CT scanner (Figure 4B).
- Transmit the CT 3D images to the navigation system automatically using a cable (Figure 4C).
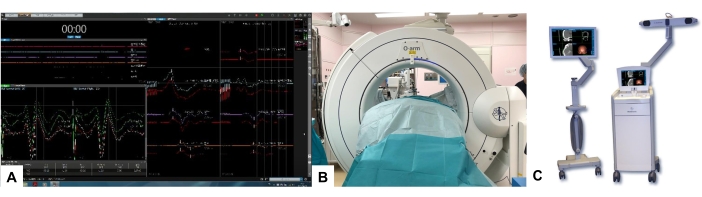
Figure 4: Neuromonitoring, O-arm, and navigation. (A) Neuromonitoring, (B) O-arm, (C) Navigation. Please click here to view a larger version of this figure.
7. Navigated instrument registration
- Register the navigated pointer, dilater, and high-speed burr by tapping the tip to the RF hole manually. Then, perform the accuracy check by touching the bony surface.
8. Incision and muscle dissection
- With the help of a navigated pointer, confirm the location of the L5-S1 foraminal level by a 50-60 mm extended image from the pointer tip and mark the entry point for the skin incision (Figure 5A).
- Make an approximately 2 cm longitudinal skin incision, and then dissect the subcutaneous tissue, lumbar iliocostalis, and multifidus muscle along the muscle fibers.
- Dock the navigated first dilator at the base of the L5 transverse process using a navigation system (Figure 5B). Then, insert the sequential dilators (5.3 mm, 9.4 mm).
- Insert the final tube (14 mm) and fix it to the flexible arm assembly firmly (Figure 5C). Confirm the position of the tube with a navigation system and the anatomy through endoscopy.

Figure 5: Skin incision and sequential dilation. (A) Navigated pointer, (B) Navigation monitor, (C) Tubular retractor. Please click here to view a larger version of this figure.
9. Bone resection with the navigated high-speed burr
- Check the level with the navigated probe. Check the L5-S1 level with a navigated pointer in the navigation monitor.
- Remove the bone at the lower base of the transverse process and the lateral part of the facet joint with a navigated high-speed burr or conventional high-speed burr (Figure 6).
NOTE: Further surgical steps are planned according to the disc herniation or canal stenosis. - In the case of canal stenosis, remove the bony element that compresses the nerve root completely.
CAUTION: Before using the navigated instruments, the surgeon should check the accuracy of navigation because sometimes the reference frame is moved.
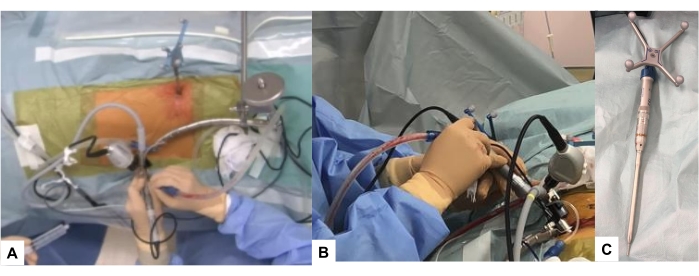
Figure 6: Navigated high-speed burr. (A,B): Intraoperative image, (B): Navigated high-speed burr. Please click here to view a larger version of this figure.
10. Endoscopic disc resection
- For LLDH, identify the L5 nerve root and retract cranially by a nerve retractor. Then, remove the disc fragment using pituitary forceps carefully.
- In the case of LFS, widen the L5 foramen using a navigated high-speed burr under navigation guidance.
- Remove every compressing soft tissue and bony element by pituitary forceps and Kerrison rongeurs. Identify the L5 root by its surrounding perineural fat and vessels (Figure 7).
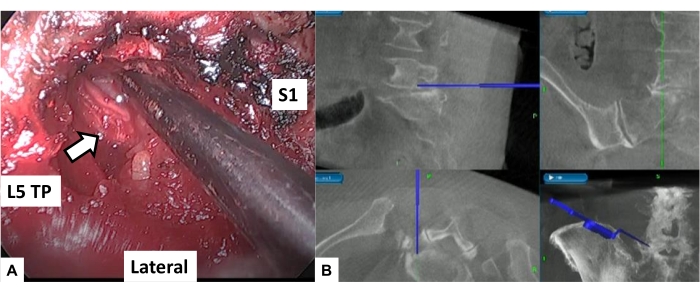
Figure 7: Nerve root decompression. (A) Endoscope image; identifying and decompressing the L5 root (white arrow); the inter-vertebral foramen is widened by burring down the osteophytes with the help of a navigated burr. (B) Navigation monitor; during operation, the surgeons can view the one monitor indicating four pieces of information simultaneously: the surgical field, intraoperative neuromonitoring, intraoperative navigation, and microendoscope view. Please click here to view a larger version of this figure.
11. Skin closure
- After irrigation with saline water to remove the debris, place a wound suction tube at L5-S1.
- Then, close the skin with an absorbable suture.
- Postoperatively, remove the drain after 48 h.
NOTE: Postoperative images are shown in Figure 8.
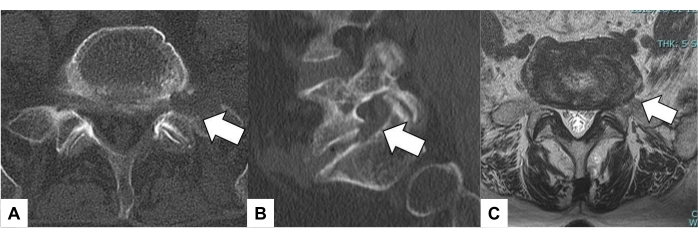
Figure 8: Postoperative images. (A) Axial CT image at L5-S1, (B) Parasagittal reconstruction CT, (C) Axial T2 weighted MR imaging at L5-S1. The white arrows indicate the decompression area. Please click here to view a larger version of this figure.
Results
Eight cases (four men, four women) underwent surgery using this new technique. The average age was 72.0 years, and the average follow-up period was 1.5 years. There were five patients with L5/S1 foraminal stenosis, two patients with L5/S foraminal disc herniation, and one patient with L3/4 foraminal disc herniation. We could perform all surgeries without a C-arm. The average surgical time and blood loss were 143 min ± 14 min and 134 ± 18 mL, respectively.
The average recovery percent...
Discussion
L5 radicular symptoms are caused mainly by L4-L5 disc herniation or stenosis. These symptoms may also occur due to L5 lumbar foraminal stenosis or L5-S1 lateral lumbar disc herniation (LLDH)9. Of all the symptomatic lumbar disc herniations, L5-S1 FLDH accounts for approximately 3%10. For L5-S1 foraminal lesions, a posterolateral or transforaminal approach is recommended. For this approach, there are three main techniques, such as the microscopic, tube with endoscopic, and f...
Disclosures
The authors declare that there are no conflicts of interest.
Acknowledgements
This study was supported by the Okayama Spine Group.
Materials
| Name | Company | Catalog Number | Comments |
| 1488 HD 3-Chip camera system | Stryker | 1000902487 | |
| 16mm Endoscope Attachment, Sterile | Medtronic | 9560160 | |
| 18mm Endoscope Attachment, Sterile | Medtronic | 9560180 | |
| 4K 32" surgical display | Stryker | 0240-031-050 | |
| Adjustable hinged operating carbon table | Mizuho OSI | 6988A-PV-ACP | OSI Axis Jackson table |
| L10 AIM light source | Stryker | 1000902487 | |
| METRx MED System Endoscope, Long | Medtronic | 9560102 | |
| METRx MED System Reusable Endoscope | Medtronic | 9560101 | Metrx |
| METRx MED System Reusable Endoscope | Medtronic | 9560101 M | |
| METRx MED System Reusable Endoscope, Long | Medtronic | 9560102 | |
| Navigated high speed bur | Medtronic | EM200N | Stelth |
| Navigated passive pointer | Medtronic | 960-559 | |
| NIM Eclipse system | Medtronic | ECLC | Neuromonitouring |
| O-arm | Medtronic | 224ABBZX00042000 | Intraoperative CT |
| Stealth station navigation system Spine 7R | Medtronic | 9733990 | Navigation |
| Surgical Carts | Stryker | F-NSK-006-00 | |
| Tubular Retractor, 16mm | Medtronic | 955-524 | |
| Tubular Retractor, 16mm, Long | Medtronic | 9560216 | |
| Tubular Retractor, 18mm | Medtronic | 9560118 | |
| Tubular Retractor, 18mm, Long | Medtronic | 9560218 |
References
- Shawky, A. A., Babic, D., Siam, A. E., Ezzati, A. Extraforaminal microscopic assisted percutaneous nucleotomy for foraminal and extraforaminal lumbar disc herniations. The Spine Journal. 18 (4), 620-625 (2018).
- Mehta, R., et al. Transtubular endoscopic posterolateral decompression of the L5 root under navigation and O-arm: A technical note. Acta Medica Okayama. 75 (5), 637-640 (2021).
- Pirris, S. M., Dhall, S., Mummaneni, P. V., Kanter, A. S. Minimally invasive approach to extraforaminal disc herniations at the lumbosacral junction using an operating microscope: Case series and review of the literature. Neurosurgical Focus. 25 (2), 10 (2008).
- Kotil, K., Akcetin, M., Bilge, T. A minimally invasive transmuscular approach to far-lateral L5-S1 level disc herniations: A prospective study. Journal of Spinal Disorders and Techniques. 20 (2), 132-138 (2007).
- Stavrinou, P., et al. Navigated transtubular extraforaminal decompression of the L5 nerve root at the lumbosacral junction: Clinical data, radiographic features, and outcome analysis. BioMed Research International. 2016, 3487437 (2016).
- Heo, D. H., Sharma, S., Park, C. K. Endoscopic treatment of extraforaminal entrapment of L5 nerve root (far out syndrome) by unilateral biportal endoscopic approach: Technical report and preliminary clinical results. Neurospine. 16 (1), 130-137 (2019).
- Watanabe, K., et al. Clinical outcomes of posterior lumbar interbody fusion for lumbar foraminal stenosis: preoperative diagnosis and surgical strategy. Journal of Spinal Disorders and Techniques. 24 (3), 137-141 (2011).
- Fukui, M., et al. Japanese Orthopaedic Association Back Pain Evaluation Questionnaire. Part 2. Verification of its reliability: The Subcommittee on Low Back Pain and Cervical Myelopathy Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association. Journal of Orthopaedic Science. 12 (6), 526-532 (2007).
- Wiltse, L. L., Guyer, R. D., Spencer, C. W., Glenn, W. V., Porter, I. S. Alar transverse process impingement of the L5 spinal nerve: The far-out syndrome. Spine. 9 (1), 31-41 (1984).
- Haher, T. R., et al. The role of the lumbar facet joints in spinal stability. Identification of alternative paths of loading. Spine. 19 (23), 2667-2670 (1994).
- Foley, K. T., Smith, M. M. Microendoscopic discectomy. Techniques in Neurosurgery. 3, 301-307 (1997).
- Tanaka, M., et al. Comparison of navigated expandable vertebral cage with conventional expandable vertebral cage for minimally invasive lumbar/thoracolumbar corpectomy. Medicina. 58 (3), 364 (2022).
- Zhang, W., et al. Accuracy of pedicle screw insertion in posterior scoliosis surgery: A comparison between intraoperative navigation and preoperative navigation techniques. European Spine Journal. 26 (6), 1756-1764 (2017).
- Ikuta, K., et al. Surgical complications of microendoscopic procedures for lumbar spinal stenosis. Minimally Invasive Neurosurgery. 50 (3), 145-149 (2007).
- Frank, E. Endoscopically assisted open removal of laterally herniated lumbar discs. Surgical Neurology. 48 (5), 430-433 (1997).
- Li, Y. Z., et al. Efficacy and safety of percutaneous endoscopic decompression via transforaminal and interlaminar approaches for lumbar spine stenosis: Protocol for a systematic review and meta-analysis. Medicine. 99 (1), 18555 (2020).
- Prod'homme, M., Sans-Merce, M., Pitteloud, N., Damet, J., Lascombes, P. Intraoperative 2D C-arm and 3D O-arm in children: A comparative phantom study. Journal of Children's Orthopaedics. 12 (5), 550-557 (2018).
- Tanaka, M., et al. Percutaneous C-arm free O-arm navigated biopsy for spinal pathologies: A technical note. Diagnostics. 11 (4), 636 (2021).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved