Method Article
Allotrapianto dermico e bicipite Ricostruzione della capsula superiore per lacerazioni massicce e irreparabili della cuffia dei rotatori
In questo articolo
Riepilogo
Qui, descriviamo una tecnica modificata per l'allotrapianto dermico e la ricostruzione della capsula superiore del tendine del capo lungo del bicipite per le lacerazioni massicce e irreparabili della cuffia dei rotatori.
Abstract
Dall'uso della fascia lata autologa per la ricostruzione della capsula superiore di lesioni massicce irreparabili della cuffia dei rotatori (MIRCT), la tecnica si è evoluta in varie modifiche, tra cui allotrapianti dermici, capo lungo del tendine del bicipite (LHBT) e combinazioni di entrambi, che saranno discussi in questo articolo. Dopo essersi assicurati che la cuffia residua non possa essere ripristinata sull'impronta anatomica del sovraspinato, viene inserita un'ancora a doppio o triplo caricamento, basata su sutura, 5-8 mm posteriormente al solco bicipitale per fissare inizialmente il capo lungo del bicipite (LHBT). Una depressione ossea è realizzata 5 mm posteriormente al solco bicipitale. Uno o due anelli lazologici vengono creati attraverso l'LHBT prima del rilascio completo del legamento omerale trasverso senza tenotomia dell'LHBT distale al punto di fissazione, con conseguente reindirizzamento posteriore dell'LHBT. Viene mantenuta la conservazione dell'attacco prossimale del bicipite sul lato glenoideo, garantendo una fissazione nativa.
Successivamente, viene utilizzato un alloinnesto dermico di 3 x 3 cm di 2 mm di spessore per coprire l'LHBT reindirizzato, migliorandone la resistenza e fornendo un effetto di trazione. Per il fissaggio vengono poi impiegate quattro ancore: due ancore a doppio carico sul lato glenoideo e due ancore a fila laterale sulla maggiore tuberosità. Dopo l'introduzione dell'alloinnesto dermico nell'articolazione, le suture degli ancoraggi glenoidei vengono fissate e la tensione ottimale dell'alloinnesto viene misurata durante l'inserimento degli ancoraggi della fila laterale all'abduzione della spalla a 45°. L'allotrapianto dermico può coprire l'LHBT per aumentare l'effetto distanziatore. Non sono necessari ancoraggi di fila mediali. Le porzioni rimanenti del sovraspinato e dell'infraspinato possono essere riparate utilizzando suture passate attraverso le ancore della fila laterale o riparate con l'allotrapianto dermico insieme per migliorare la stabilità.
Introduzione
Da quando Mihata et al.1 hanno pubblicato la loro tecnica utilizzando la fascia lata autologa per riprodurre la capsula superiore della spalla, l'idea della ricostruzione della capsula superiore (SCR) è diventata molto popolare nel trattamento delle lacerazioni massicce e irreparabili della cuffia dei rotatori (MIRCT). Ci sono state molte modifiche dell'SCR, tra cui l'uso di allotrapianti dermici 2,3,4,5, tendini gracile e semitendinoso6, capo lungo del tendine del bicipite (LHBT)7,8,9, nonché combinazioni di allotrapianti dermici e LHBT10 autologo.
Ogni tecnica ha i suoi pro e i suoi contro per quanto riguarda la copertura dell'impronta, lo spessore dell'innesto e le diverse proprietà biomeccaniche. Sulla base dell'articolo11 originale di Mihata, è stato creato un innesto di 5 mm di spessore piegando la fascia lata due o tre volte e suturando attorno al bordo delle pieghe. Al contrario, Denard et al. hanno raggiunto un tasso di successo dell'80% con un tasso di revisione a breve termine del 19% utilizzando allotrapianti dermici acellulari di 1-3 mm di spessore invece della fascia lata autologa.
Barth et al. hanno reindirizzato posteriormente LHBT autologo in MIRCT e hanno scoperto che potrebbe prevenire le lacerazioni dell'infraspinato7. Kim et al. hanno confrontato i risultati dell'SCR utilizzando LHBT autologo o allotrapianti dermici e non hanno riscontrato differenze tra i due gruppi a 2 anni dall'intervento, ad eccezione del fatto che l'autotrapianto era più spesso12, poiché lo spessore medio era di 6 mm, che era simile alla fascia lata autologa di 6-8 mm utilizzata da Mihata et al9. Questo articolo presenta la nostra tecnica di combinazione di un allotrapianto dermico di 2 mm di spessore e LHBT autologo per il trattamento dei MIRCT.
Protocollo
Questa tecnica è stata approvata dal Comitato Etico della nostra istituzione (IRB 20230107080) ed è stato ottenuto il consenso informato di tutti i pazienti.
1. Selezione del paziente
- Selezionare i pazienti per le seguenti indicazioni: MIRCT inferiore all'artropatia della cuffia dei rotatori di grado 2 di Hamada (Figura 1A, B), retrazione del tendine sovraspinato allo stadio III di Patte (Figura 1C), nessuna pseudoparesi preoperatoria, infiltrazione di grasso del muscolo sovraspinato (FI) uguale o superiore allo stadio 2 di Goutallier ( Figura 1D) e presenza di LHBT13.
- Impostare i seguenti criteri di esclusione: pazienti con grave tenuta capsulare, limitazione del movimento definita come rotazione passiva interna o esterna inferiore a 30°, precedente intervento chirurgico alla spalla omolaterale, > Lafosse di Lafosse tipo 314, fratture, patologie correlate all'infezione, lesione parziale o completa di LHBT, grave artrosi dell'articolazione gleno-omerale e deformità della testa omerale alla radiografia preoperatoria.
2. Procedura chirurgica
- Mettere il paziente in una posizione di sedia a sdraio con un supporto per le braccia.
- Eseguire un completo rilascio artroscopico della cuffia dei rotatori rimanente.
- Definire la lesione sottoscapolare secondo la classificazione di Lafosse (Figura 2A)14 e riparare di conseguenza (Figura 2B).
- Rilasciare artroscopicamente tutte le fibre verticali sotto il sovraspinato.
- Inserire un'ancora a doppio o triplo caricamento, basata su sutura, 5 mm posteriormente al solco bicipitale per fissare inizialmente l'LHBT (Figura 2C).
- Creare un anello lazo attraverso l'LHBT (Figura 2D).
- Realizzare un trogolo osseo di 5 mm posteriormente al boschetto bicipitale (Figura 2E).
- Rilascio completo del legamento omerale trasverso.
- Legare gli anelli del lazo fatti passare attraverso l'LHBT e reindirizzare posteriormente l'LHBT dall'anello del lazo appena realizzato (Figura 2F).
NOTA: Non eseguire una tenotomia per preservare l'integrità dell'LHBT. - Mantenere l'attacco prossimale dell'LHBT sul lato glenoideo, garantendo la fissazione nativa.
- Utilizzare l'altra sutura dell'ancora per riparare la cuffia anteriore residua, fornendo una maggiore copertura dei tessuti molli sopra l'LHBT reindirizzato (Figura 2G).
- Inserire due ancore basate su sutura a doppio carico attraverso il portale Naviaser nella parte superiore della glenoide, consentendo quattro paia di suture (Figura 2H), e trasportarle attraverso il portale anterolaterale per un ulteriore utilizzo.
- Far passare tutte e otto le suture (quattro paia di suture) dalle due ancore attraverso un lato di un alloinnesto dermico di 3 x 3 cm con uno spessore di 2 mm, all'esterno della spalla.
- Legare insieme una sutura da ciascuna ancora per fornire una moda a doppia puleggia (Figura 2I). Le altre 2 paia di suture attraverso l'allotrapianto dermico funzionano con una sutura a materasso.
- Utilizzare una siringa da 10 ml tagliata a metà come cannula fatta a mano abbastanza lunga da avvicinarsi approssimativamente alla glenoide, facilitando la doppia puleggia e le due suture del materasso che fissano l'allotrapianto dermico sopra la glenoide mediale (Figura 2J).
- Passare i due arti di suture libere o una sutura FiberTape dal lato laterale dell'innesto, che viene utilizzata per il fissaggio della fila laterale (Figura 2K).
- Introdurre e fissare l'allotrapianto dermico sulla glenoide.
- Inserire un'ancora alla maggiore tuberosità.
- Fissare la parte laterale dell'allotrapianto dermico con le suture pre-passate.
- Coprire l'impronta sovraspinato con l'innesto, che è determinata da dove fissare l'allotrapianto dermico tramite l'ancoraggio della fila laterale.
- Ottimizzare la tensione dell'alloinnesto durante l'inserimento dell'ancoraggio laterale all'abduzione della spalla a 45° (Figura 2L)15.
- Coprire l'allotrapianto dermico sopra l'LHBT per aumentare l'effetto distanziatore.
NOTA: Non sono necessari ancoraggi di fila mediali. - Eseguire ulteriori suture da un lato all'altro tra l'allotrapianto dermico fisso e l'infraspinato (Figura 2M, N).
- Riparare le parti rimanenti del sovraspinato e dell'infraspinato utilizzando suture passate attraverso l'ancora per migliorare la stabilità.
NOTA: Non è necessaria alcuna sutura tra il sottoscapolare e l'allotrapianto dermico fisso. Tutta l'impronta esposta dell'omero prossimale è coperta da LHBT, allotrapianto dermico e cuffia dei rotatori residua (Figura 2O).
Risultati
Un totale di 39 pazienti ha soddisfatto i criteri di inclusione; Quattro sono stati esclusi, lasciando 8 maschi e 27 femmine per lo studio. I dati demografici dei pazienti sono elencati nella Tabella 1. Non vi è stato alcun cambiamento significativo per quanto riguarda il range di movimento attivo della spalla (ROM) e la distanza acromio-omerale (AHD) prima e dopo l'intervento chirurgico (Tabella 2). C'è stato un miglioramento significativo nelle scale del dolore e negli esiti funzionali al follow-up di 2 anni. Il punteggio analogo visivo (VAS) ha dimostrato miglioramenti sostanziali, diminuendo da 8,2 ± 0,6 a 1,3 ± 0,6, il valore soggettivo della spalla (SSV) è migliorato da 23,1 ± 9 a 79,3 ± 11,6, il punteggio di Constant-Murley (CMS) da 37 ± 7,6 a 81,1 ± 8,1 e i punteggi dei chirurghi americani della spalla e del gomito (ASES) da 38,7 ± 10,6 a 80,7 ± 5,3 al follow-up finale (tutti P < 0,001) (Tabella 2). Trentatré pazienti hanno dimostrato una guarigione dell'allotrapianto dermico sull'impronta del sovraspinato durante l'esame di risonanza magnetica di follow-up di 1 anno (Figura 3). Due pazienti (5,7%) hanno manifestato un reperimento del lato omerale. Entrambi sono stati sottoposti ad artroplastica totale della spalla (RSA) inversa durante l'intervento chirurgico di revisione, portando a un recupero senza incidenti.
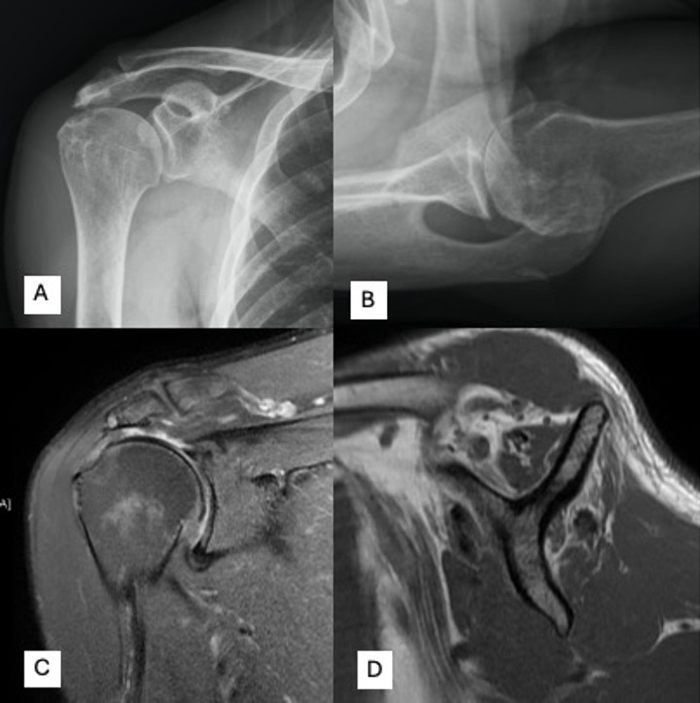
Figura 1: Valutazione radiologica preoperatoria. (A,B) I pazienti che si sottopongono a questa tecnica devono avere un'artropatia da rottura della cuffia dei rotatori di grado inferiore a Hamada 2. (C) Retrazione del tendine sovraspinato allo stadio III di Patte e (D) Infiltrazione di grasso del muscolo sovraspinato uguale o superiore allo stadio 2 di Goutallier. Clicca qui per visualizzare una versione più grande di questa figura.
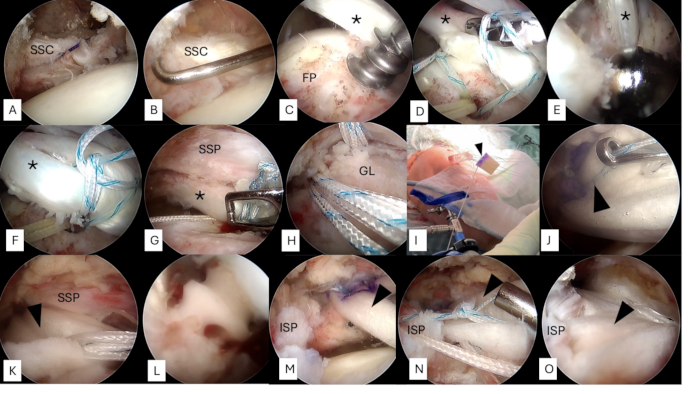
Figura 2: Spalla destra, vista dal portale laterale in posizione di sedia a sdraio. (A,B) Qualsiasi lesione sottoscapolare viene definita e riparata. (C) Un'ancora a doppio o triplo caricamento, basata su sutura, viene inserita 5 mm posteriormente al solco bicipitale. (D) Un anello lazo viene utilizzato per fissare l'LHBT. (E) Viene realizzata una depressione ossea 5 mm posteriormente al boschetto bicipitale. (F) Dopo il completo rilascio del legamento omerale trasverso, l'ansa lazologica passata attraverso l'LHBT viene legata e l'LHBT viene reindirizzato posteriormente. Non viene eseguita alcuna tenotomia distale per preservare l'integrità dell'LHBT. (G) L'altra sutura può essere utilizzata per riparare la cuffia anteriore residua, se necessario, fornendo una maggiore copertura dei tessuti molli sopra l'LHBT reindirizzato. (H) Due ancore basate su sutura a doppio carico vengono inserite nella parte superiore della glenoide, consentendo quattro suture. (I) Un paio di suture di ciascuna ancora glenoidea viene fatto passare attraverso un lato di un alloinnesto dermico di 3 x 3 cm con uno spessore di 2 mm, fornendo una doppia puleggia. Le altre due paia di suture vengono fatte passare attraverso l'allotrapianto dermico in modo da materasso. (J) Una siringa da 10 ml tagliata a metà può essere utilizzata come cannula fatta a mano abbastanza lunga da avvicinarsi approssimativamente alla glenoide, facilitando la doppia puleggia e le due suture a materasso che fissano l'allotrapianto dermico sopra la glenoide mediale. (K) Due arti di suture libere o suture vengono fatti passare dal lato laterale dell'innesto, che viene utilizzato per la fissazione della fila laterale. (L) Inserendo un'ancora di fila laterale in corrispondenza della maggiore tuberosità, la parte laterale dell'allotrapianto dermico viene fissata con le suture pre-passate. (M, N) Le suture aggiuntive da un lato all'altro possono essere eseguite tra l'allotrapianto dermico fisso e l'infraspinato. (O) Infine, tutta l'impronta esposta dell'omero prossimale è coperta da LHBT, allotrapianto dermico e cuffia dei rotatori residua. Gli asterischi indicano LHBT; Le punte di freccia nere puntano all'allotrapianto dermico. Abbreviazioni: SSC = sottoscapolare; FP = impronta; LHBT = capo lungo del bicipite; GL = glenoide; SSP = sovraspinato; ISP = infraspinato. Clicca qui per visualizzare una versione più grande di questa figura.

Figura 3: Immagini preoperatorie e postoperatorie di un paziente che riceve questa tecnica. (A) Una paziente di 70 anni con riparazione della cuffia dei rotatori precedentemente fallita presentava un'artropatia della cuffia dei rotatori di tipo 1 di Hamada. La radiografia anteroposteriore ha rivelato una distanza acromio-omerale superiore a 7 mm, (B) e una retrazione della cuffia dei rotatori di stadio III di Patte. (C) L'infiltrazione adiposa del muscolo sovraspinato era allo stadio Goutallier 2. (D) La radiografia anteroposteriore postoperatoria si presentava con una distanza acromio-omerale conservata. (E,F) La risonanza magnetica coronale e sagittale ha rivelato un allotrapianto dermico guarito sull'impronta del sovraspinato all'esame di risonanza magnetica di follow-up di 1 anno. La punta della freccia punta verso l'allotrapianto dermico. Clicca qui per visualizzare una versione più grande di questa figura.
| No. di pazienti | 35 |
| Età (anno) | 63,8 ± 7,7 |
| Maschio /femmina | 8 / 27 |
| Indice di massa corporea (kg/m2) | 24,2 ± 4,4 |
| Durata del follow-up (mesi) | 24,2 ± 5,3 |
| Lato dell'ambulatorio, destra/sinistra | 14 / 21 |
| Malattia sistematica, (diabete, ipertensione), n / % | 22, 9% |
| Radiografia preoperatoria | |
| AHD (mm) | 7,8 ± 2,2 |
| Risonanza magnetica preoperatoria | |
| Classificazione di Patte con retrazione SSP | |
| (I/II/III, n) | 0 / 0 / 35 |
| Grado di cambio grasso (0 / 1 / 2 / 3 / 4) | |
| SSC | 18 / 13 / 3 / 1 / 0 |
| SSP | 0 / 0 / 2 / 23 /10 |
| Fornitore di servizi | 4 / 23 / 8 / 0 / 0 |
| ROM attivo preoperatorio della spalla | |
| FF (°) | 132,9 ± 34,6 |
| ER 1 (°) | 56,3 ± 15,2 |
| IR (1~18) | 11,4 ± 3,4 |
Tabella 1: Caratteristiche dei pazienti. Abbreviazioni: ROM = gamma di movimento; AHD = distanza acromio-omerale; SSC = sottoscapolare; SSP = sovraspinato; ISP = infraspinato; FF = prospetto anteriore; ER1 = rotazione esterna; IR = rotazione interna.
| Preoperatorio | Postoperatorio | Valore P | |
| Radiografia | |||
| AHD (mm) | 7,8 ± 2,2 | 7,2 ± 2,5 | 0.296 |
| ROM attiva | |||
| FF (°) | 132,9 ± 34,6 | 148,6 ± 19,4 | 0.022 |
| ER 1(°) | 56,3 ± 15,2 | 60,3 ± 12 | 0.225 |
| IR | 11,4 ± 3,4 | 10,7 ± 3,2 | 0.43 |
| Intensità del dolore | |||
| VAS | 8,2 ± 0,6 | 1,3 ± 0,6 | <0,001 |
| Punteggio funzionale | |||
| SSV | 23.1 ± 9 | 79,3 ± 11,6 | <0,001 |
| CMS | 37 ± 7,6 | 81,1 ± 8,1 | <0,001 |
| ASES | 38,7 ± 10,6 | 80,7 ± 5,3 | <0,001 |
Tabella 2: Esiti postoperatori. Abbreviazioni: ROM = gamma di movimento; AHD = distanza acromio-omerale; FF = flessione in avanti, ER = rotazione esterna; IR = rotazione interna; VAS = scala analogica visiva; SSV = Valore soggettivo della spalla; ASES = chirurghi americani della spalla e del gomito; CMS = Punteggio di Murley costante.
Discussione
Il passaggio critico in questo protocollo è che non inseriamo ancore di fila mediali come nella tecnica SCR convenzionale proposta da Mihata et al.11 Secondo la tecnica originale, una misurazione precisa delle dimensioni dell'innesto è importante per fornire una tensione adeguata. Invece, trasportiamo la sutura Fibertape da un'ancora Swivelock per realizzare una sutura a materasso inversa sul lato laterale dell'allotrapianto dermico, che viene utilizzata per fissare l'innesto sull'impronta quando l'ancora Swivelock viene inserita nella maggiore tuberosità all'abduzione della spalla a 45°. L'angolo di fissazione dell'abduzione della spalla a 45° mantiene una tensione appropriata a 90° dell'abduzione della spalla e previene le lacerazioni dell'innesto a 0° dell'abduzione della spalla11. In questo modo, è possibile ottenere la massima tensione durante il serraggio durante l'inserimento dell'ancora Swivelock e non sarà influenzata dalla posizione dell'ancora della fila mediale.
Questa tecnica modificata offre flessibilità nella fissazione dermica dell'allotrapianto perché la posizione effettiva della fissazione dermica dell'alloinnesto dipende dalla posizione per coprire la parte più esposta dell'impronta determinata dalla posizione inserita degli ancoraggi laterali. Se l'infraspinato può essere ridotto alla sua posizione anatomica, l'allotrapianto dermico può essere fissato più anteriormente, sopra l'LHBT reindirizzato posteriormente per creare un maggiore effetto spaziatore, perché la parte antero-superiore della capsula anatomica è più spessa, con una media di 2,3 mm. Dopotutto, include il legamento gleno-omerale superiore16. Se l'infraspinato non può essere tirato indietro per coprire la sua impronta, l'autore fisserà l'allotrapianto più posteriormente, coprendo l'impronta più esposta. Come riportato da Mirzayan et al., una lacerazione dell'innesto che lascia la tuberosità coperta ha un dolore inferiore e punteggi funzionali più elevati rispetto a coloro in cui l'innesto strappato lascia la tuberosità scoperta17. Pertanto, coprire la maggior parte dell'ingombro potrebbe essere importante quanto fornire un forte effetto distanziatore. Inoltre, le porzioni rimanenti del sovraspinato e dell'infraspinato possono essere riparate utilizzando suture passate attraverso l'ancora Swivelock per migliorare la stabilità. L'allotrapianto dermico può anche fungere da ponte biologico quando il residuo del sovraspinato e dell'infraspinato vengono suturati con esso.
Ci sono due limitazioni a questa tecnica. In primo luogo, la qualità dell'LHBT non può essere controllata prima dell'intervento. Sono stati esclusi solo i pazienti in cui l'LHBT era assente prima dell'intervento chirurgico. Se l'LHBT era presente, lo abbiamo considerato un aumento biologico ed abbiamo eseguito la tecnica bio-SCR indipendentemente dalle dimensioni o dalla qualità del tendine del bicipite, come riportato da McClatchy et al.18. In secondo luogo, non abbiamo un gruppo di controllo, come la riparazione parziale della cuffia dei rotatori o del bicipite SCR da solo, poiché questo è un rapporto per un protocollo chirurgico.
Il significato del metodo è che combina i vantaggi del bicipite e dell'SCR dermico ed evita la complicazione del prelievo della fascia lata. Inoltre, questa tecnica consente la copertura dell'impronta senza l'uso di ancoraggi mediali della fila, il che può portare a una procedura più economica. Non tagliamo la parte prossimale dell'LHBT che è già fissata alla glenoide attraverso il sito di ancoraggio nativo, il che ovvia alla necessità di fissazione dell'ancora e di un'altra interfaccia per potenziali guasti. Inoltre, non tagliamo la parte distale dell'LHBT, ma creiamo un nuovo avvallamento poiché Kim et al.19 hanno proposto di fissare l'LHBT reindirizzato posteriormente, lasciando l'LHBT intatto per fornire un effetto spazio.
Questa tecnica può essere potenzialmente applicata a tutti i MIRCT quando l'LHBT è presente e il paziente è senza ritardo di rotazione esterna. C'è ancora dibattito tra la biomeccanica dell'SCR e il trasferimento del trapezio inferiore (LTT) per i MIRCT. Mentre sia l'SCR che l'LTT riducono la traslazione e la pressione di contatto superiori gleno-omerali rispetto alle condizioni di MIRCT postero-superiore, l'LTT era superiore all'SCR in termini di traslazione superiore della testa omerale a un angolo di abduzione della spalla più elevato. Al contrario, l'SCR ha mostrato caratteristiche di contatto subacromiale più vantaggiose rispetto all'LTT20. Ulteriori studi dovrebbero concentrarsi sulla corretta posizione di attacco dell'innesto e sullo spessore dell'innesto. In sintesi, la tecnica SCR combinata che utilizza un allotrapianto dermico da 2 mm e LHBT autologo per i MIRCT migliora significativamente gli esiti riportati dai pazienti.
Divulgazioni
Gli autori non hanno conflitti di interesse da dichiarare.
Riconoscimenti
Gli autori ringraziano con gratitudine il Ministro della Scienza e della Tecnologia di Taiwan e il Linkou Chang Gung Memorial Hospital per il sostegno finanziario di questo studio (Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, CMRPG5K0092, CMRPG3M2032, CMRPG5K021, SMRPG3N0011)
Materiali
| Name | Company | Catalog Number | Comments |
| 3 x 3 cm dermal allograft of 2 mm thickness | Megaderm; L&C BIO Inc., Seongnam, Korea | ||
| BioComposite SwiveLock C anchor | Arthrex, Naples, FL | anchor | |
| FiberTape | Arthrex, Naples, FL | suture |
Riferimenti
- Mihata, T., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 29 (3), 459-470 (2013).
- Denard, P. J., Brady, P. C., Adams, C. R., Tokish, J. M., Burkhart, S. S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 34 (1), 93-99 (2018).
- Hirahara, A. M., Adams, C. R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 4 (6), e637-e641 (2015).
- Pennington, W. T., Bartz, B. A., Pauli, J. M., Walker, C. E., Schmidt, W. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: Short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 34 (6), 1764-1773 (2018).
- Burkhart, S. S., Denard, P. J., Adams, C. R., Brady, P. C., Hartzler, R. U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 5 (6), e1407-e1418 (2016).
- Protais, M., et al. Use of gracile and semi-tendinosus tendons (grast) for the reconstruction of irreparable rotator cuff tears. BMC Musculoskelet Disord. 22, 1-8 (2021).
- Barth, J., et al. Superior capsular reconstruction with the long head of the biceps autograft prevents infraspinatus retear in massive posterosuperior retracted rotator cuff tears. Am J Sports Med. 48 (6), 1430-1438 (2020).
- Boutsiadis, A., et al. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: "The Chinese way". Arthrosc Tech. 6 (5), e1559-e1566 (2017).
- Chiang, C. -. H., et al. Modified superior capsule reconstruction using the long head of the biceps tendon as reinforcement to rotator cuff repair lowers retear rate in large to massive reparable rotator cuff tears. Arthroscopy. 37 (8), 2420-2431 (2021).
- Chiu, C. -. H., et al. Anatomical dermal allograft and autologous biceps long head superior capsule reconstruction for irreparable posterosuperior rotator cuff tears. Arthrosc Tech. 10 (10), e2237-e2243 (2021).
- Mihata, T., Mcgarry, M. H., Pirolo, J. M., Kinoshita, M., Lee, T. Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 40 (10), 2248-2255 (2012).
- Kim, D. S., Han, J. Y., Park, Y. J., Kwak, J. W., Lee, B. S. Comparative analysis of superior capsule reconstruction between long head of biceps tendon autograft and human dermis allograft. J Shoulder Elbow Surg. 32 (4), 820-831 (2023).
- Chiu, C. H., et al. Anatomical dermal allograft and autologous biceps long head superior capsule reconstruction for irreparable posterosuperior rotator cuff tears. Arthrosc Tech. 10 (10), e2237-e2243 (2021).
- Lafosse, L., et al. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 89 (6), 1184-1193 (2007).
- Mihata, T., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 29 (3), 459-470 (2013).
- Clavert, P., et al. An anatomical study of the fetal superior capsule of the glenohumeral joint. Orthop & Traumatol Surg Res. 107 (8), 103073 (2021).
- Mirzayan, R., Stone, M. A., Batech, M., Acevedo, D. C., Singh, A. Failed dermal allograft procedures for irreparable rotator cuff tears can still improve pain and function: The "biologic tuberoplasty effect". Orthop J Sports Med. 7 (8), 2325967119863432 (2019).
- Mcclatchy, S. G., Parsell, D. E., Hobgood, E. R., Field, L. D. Augmentation of massive rotator cuff repairs using biceps transposition without tenotomy improves clinical and patient-reported outcomes: The biological superior capsular reconstruction technique. Arthroscopy. 40 (1), 47-54 (2024).
- Kim, D., Um, J., Lee, J., Kim, J. Improved clinical and radiologic outcomes seen after superior capsule reconstruction using long head biceps tendon autograft. Arthroscopy. 37 (9), 2756-2767 (2021).
- Baek, G., et al. Biomechanical comparison between superior capsular reconstruction and lower trapezius tendon transfer in irreparable posterosuperior rotator cuff tears. Am J Sports Med. 52 (6), 1419-1427 (2024).
Ristampe e Autorizzazioni
Richiedi autorizzazione per utilizzare il testo o le figure di questo articolo JoVE
Richiedi AutorizzazioneEsplora altri articoli
This article has been published
Video Coming Soon