Method Article
Laparoscopy-endoscopy Cooperative Surgery for the Treatment of Gastric Gastrointestinal Stromal Tumors
* These authors contributed equally
In This Article
Summary
Laparoscopy-endoscopy cooperative surgery is appropriate for the treatment of gastric gastrointestinal stromal tumors less than 5 cm in size. It can achieve the respective advantages of endoscopic and laparoscopic surgeries while avoiding their drawbacks.
Abstract
In view of the shortcomings of endoscopic or laparoscopic surgeries alone in the treatment of gastric gastrointestinal stromal tumors (G-GISTs), this approach makes an innovative improvement in the treatment of G-GISTs that are less than 5 cm in size. Laparoscopy-endoscopy cooperative surgery (LECS) is used to combine endoscopic and laparoscopic surgeries, fully realizing their respective advantages and avoiding their drawbacks. The main steps are as follows. First, gastroscopy and laparoscopy are combined to confirm the location and boundary of the tumor. Tumor resection is carried out laparoscopically, guided by a gastroscope. The specimen is removed orally and the gastric wound closed laparoscopically. Then, gastroscopy and laparoscopy are combined to determine whether there is wound bleeding, if the suture is satisfactory, and if the gastric cavity is deformed.
LECS has natural advantages in the treatment of G-GISTs that are less than 5 cm in size. The accurate estimation of tumor location and boundary greatly improves the complete resection rate of tumors. The risk of tumor rupture is substantially reduced, and the long-term prognosis of patients is significantly improved. The process allows for accurate resection of the tumor, maximum preservation of normal gastric tissue and organ function, and avoids postoperative gastric deformation. The patient's postoperative rehabilitation is greatly accelerated, and oral feeding can resume on the day of the operation. The specimen is taken out through the mouth to avoid the need for an extended abdominal incision. This greatly reduces the patient's postoperative pain and scarring. The method greatly shortens the postoperative hospital stay (i.e., discharge is possible on the day after the operation), increasing the turnover of hospital beds.
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common subepithelial lesions in the gastrointestinal tract1. Endoscopic or laparoscopic surgeries are common surgical methods for treating gastric gastrointestinal stromal tumors (G-GIST) less than 5 cm in size2,3,4. However, endoscopic surgery alone has some disadvantages, such as inaccurate tumor localization and boundary judgment, tumor rupture, low-quality wound closure, bleeding. Therefore, according to the guidelines, endoscopic surgery alone is not presently recommended as a surgical method for the treatment of G-GISTs5,6. There are also disputes regarding the treatment of G-GISTs through endoscopic surgery alone in practical clinical work. Compared to endoscopic surgery, laparoscopic surgery has the advantages of a clearer field of vision, fuller exposure, and larger resection range7,8. However, laparoscopic surgery alone also has difficulties in terms of judging the tumor location (for endogenous tumors) and inaccurate judgment of tumor boundaries, resulting in tumor rupture, especially when the tumor is located near the lesser curvature or cardia of the posterior wall of the stomach. Additionally, if the tumor boundary is not judged correctly, the resection range will be too large, resulting in gastric deformation.
In view of the shortcomings of endoscopic and laparoscopic surgeries performed separately, we developed an innovative, improved approach in the treatment of G-GISTs less than 5 cm in size. Laparoscopy-endoscopy cooperative surgery (LECS) is used to organically combine endoscopic and laparoscopic surgical techniques, fully leveraging their respective advantages while avoiding their respective drawbacks. The goals of this method include reducing trauma, preserving gastric function, promoting postoperative rehabilitation, and improving postoperative quality of life while still safely and accurately removing G-GISTs less than 5 cm in size.
Protocol
This study was conducted with the approval of the Research Ethics Committee (Institutional Review Board) of The First Affiliated Hospital, Sun Yat-sen University (Guangzhou, China) (No. 2022085) and the Seventh Affiliated Hospital, Sun Yat-sen University (Shenzhen, China) (No. KY-2022-006-01).
1. Preoperative preparation
- Put the patient on 3 h of preoperative fasting for fluid and 6 h fasting for solid food.
- Administer general anesthesia via tracheal intubation.
- Administer prophylactic antibiotics with second-generation cephalosporins 30 min before surgery.
2. Gastroscopic exploration
- After administering general anesthesia, perform gastroscopy on the patient with CO2 insufflation.
- Next, aspirate the residual gastric fluid, and confirm the location of the tumor.
- After the exploration, completely aspirate the CO2 and fluid in the stomach and the fluid and mucus in the esophagus and throat.
NOTE: In this hospital, GI surgeons perform gastroscopy.
3. Laparoscopic exploration
- Place the patient in a supine position with legs open. Have the surgeon stand to the left, the assistant to the right, and the camera holder between the patient's legs.
- Use a four-trocar method with two 10 mm and two 5 mm trocars, and apply a CO2 pressure of 10 to 12 mmHg.
- First, confirm the location and boundary of the tumor in the stomach with the help of gastroscopy, if necessary. Then, perform a wide intraabdominal exploration to exclude any other lesions.
4. Laparoscopic tumor resection guided by gastroscopy
- Dissect the omentum tissue around the mass. Ensure the dissection plane is just above the muscle to avoid vagal trunk injury.
- Resect the mass en bloc with a 5 mm visual negative margin.
- After resection, place the specimen in the gastric cavity through the gastric wall defect.
NOTE: Before resection, it is recommended to make a 4-0 absorbable seromuscular suture ~5 mm from the tumor margin to facilitate retraction during the resection.
5. Laparoscopic closure of the gastric wall defect
- First, perform a full-thickness running suture with an absorbable 3-0 V-lock suture to close the defect in the gastric wall.
- Then, perform a seromuscular running suture with the same 3-0 V-lock suture to strengthen the closure.
6. Stomach wound check
- After laparoscopic closure, conduct a leakage test using a combination of laparoscopy and gastroscopy.
- Laparoscopically check if there are any bubbles coming out of the wound after flushing with water.
- Check if there is wound bleeding, whether the suture is satisfactory, and whether the gastric cavity has been deformed by the gastroscopy.
7. Oral specimen harvest
- Pull the specimen out through the mouth using an endoscopic basket.
NOTE: If the tumor size is more than 3 cm, temporary deflation of the intubation tube sac may be necessary.
8. Specimen management
- After the procedure, check the specimen visually to confirm the margin status.
- Then, immerse the specimen in a neutral 10% formalin solution.
NOTE: Slice the tumor every 1 cm if the tumor is more than 2 cm in size to ensure full fixation.
Results
From 2017 to 2020, 10 patients with G-GISTs received LECS (Table 1). Every GIST diagnosis was confirmed through pathological examination. None were converted to open surgery. The average age was 49 years. The average tumor size was 2.7 cm. Location of the tumor: 7 at the anterior wall, 2 at the posterior wall, and 1 at lesser curvature. The average operation duration was 112 min, and the average intraoperative blood loss was 8 mL. All patients resumed oral fluid consumption 2 h after surgery, and the average postoperative hospital stay was 73 h. All cases had negative tumor margins, and there were no perioperative complications. Every patient received regular follow-up, including gastroscopy. There were no gastric deformities (Figure 1) or recurrences.
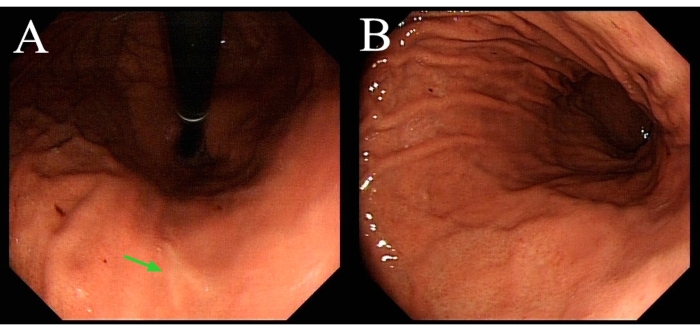
Figure 1: Gastroscopy of the same patient demonstrated in the video three months after surgery. (A) The green arrow indicates the healed wound. (B) The gastric cavity shows no deformity. Please click here to view a larger version of this figure.
| Case | Gender | Age (years) | Tumor Size (cm) | Operation Duration (min) | Blood Loss (mL) | Postoperative Hospital Stay (h) |
| 1 | F | 46 | 2 | 80 | 5 | 46 |
| 2 | F | 33 | 2.5 | 80 | 5 | 67 |
| 3 | F | 71 | 1.5 | 105 | 2 | 42 |
| 4 | F | 47 | 2.5 | 130 | 10 | 70 |
| 5 | M | 35 | 4 | 185 | 20 | 134 |
| 6 | F | 42 | 4 | 190 | 10 | 69 |
| 7 | M | 63 | 4.5 | 135 | 20 | 69 |
| 8 | F | 57 | 2.2 | 88 | 5 | 68 |
| 9 | M | 51 | 1.8 | 65 | 5 | 93 |
| 10 | M | 46 | 2.1 | 63 | 5 | 74 |
| Average | 49 | 2.7 | 112 | 8 | 73 |
Table 1: Clinical parameters of 10 cases.
Discussion
LECS has natural advantages for the treatment of G-GISTs that are less than 5 cm in size. The accurate judgment of tumor location and boundary greatly improves the complete resection rate of the tumor. The process substantially reduces the risk of tumor rupture and significantly improves the long-term prognosis. The method allows for accurate resection of the tumor, maximum preservation of normal gastric tissue and organ function, and avoids postoperative gastric deformation. The patient's postoperative rehabilitation is greatly accelerated, and oral feeding can be resumed on the day of operation. The specimen is taken out through the mouth to avoid removal through an extended abdominal incision. This greatly reduces the patient's postoperative pain and scarring. The process greatly shortens the postoperative hospital stay (allowing the patient to be discharged on the first day after the operation) and speeds up the turnover of hospital beds9,10,11,12.
Some technical elements are noteworthy. First, complete suction of the residual fluid in the stomach during gastroscopic exploration is essential to prevent intraoperative pollution. Second, continuously holding the tumor with a seromuscular suture during laparoscopic resection is also necessary to prevent intraoperative pollution. Third, when closing the gastric wall defect, suture as little of the gastric mucosal tissue as possible to ensure the inversion effect of suturing and eventually guarantee the postoperative healing quality of the wound.
All patients in this cohort received excellent oncological results with minimal invasiveness and reservation of stomach function, no positive tumor margin or recurrence, intraoperative blood loss of less than 10 mm, and operation duration of less than 2 h. All patients had an enhanced and smooth postoperative recovery, with the average postoperative hospital stay being three days.
There are some limitations to this method. First, compared with other forms of LECS without opening the gastric wall, such as NEWS or CLEAN-NET, this method has the risk of intraoperative gastric content dissemination. However, the risk is very low with complete gastroscopic suction before opening the stomach. Moreover, this low risk is reasonable and acceptable compared to the far-shortened operation duration. Second, although the maximum tumor diameter of this cohort reached up to 4.5 cm, tumors more than 4 cm diameter are challenging for oral retrieval. Third, although laparoscopic resection guided by gastroscopy is safe and efficient in most cases, gastroscopic preresection may be needed for some tumors with ingrown patterns.
We did not discuss the application of LECS in the treatment of G-GISTs that are more than 5 cm in size. Future application of LECS may include comparisons to endoscopic or laparoscopic surgery in prospective randomized trials. In conclusion, laparoscopy-endoscopy cooperative surgery is appropriate for the treatment of gastric gastrointestinal stromal tumors that are less than 5 cm in size, achieving the respective advantages of endoscopic and laparoscopic surgeries while avoiding their drawbacks.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 82172637), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No. 2021-JKCS-004) and the Guangdong Provincial Key Laboratory of Digestive Cancer Research (No. 2021B1212040006).
Materials
| Name | Company | Catalog Number | Comments |
| Eneoscopic facilites | |||
| Camera Control Unit | Olympus, Tokyo, Japan | CV-290 | |
| Disposable Grasping Forceps with Net | Changzhou Jiuhong Medical Instrument, Changzhou, China | JHY-FG-25-230-C1-5 | |
| Electronic Gastroscope | Olympus, Tokyo, Japan | GIF-HQ290 | |
| LCD Monitor | Olympus, Tokyo, Japan | OEV262H | |
| Xenon Light Source | Olympus, Tokyo, Japan | CLV-290 | |
| Laparoscopic facilities | |||
| Camera Control Unit | Olympus, Tokyo, Japan | OTV-S400 | |
| Camera Head | Olympus, Tokyo, Japan | CH-S400-XZ-EB | |
| HARMONIC ACE+7 | Johnson & Johnson, New Brunswick, USA | HARH36 | |
| LCD Monitor | Olympus, Tokyo, Japan | LMD-X550S/LMD-X310S | |
| Ultrasonic Surgical & Electrosurgical Generator | Johnson & Johnson, New Brunswick, USA | GEN11CN | |
| ULTRA Telescope | Olympus, Tokyo, Japan | WA4KL130 | |
| V-Loc Suture | Medtronic, Minneapolis, USA | 3-0. | |
| Xenon Light Source | Olympus, Tokyo, Japan | CLV-S400 |
References
- Rubin, B. P., Heinrich, M. C., Corless, C. L. Gastrointestinal stromal tumour. Lancet. 369 (9574), 1731-1741 (2007).
- Chen, K., et al. Systematic review and meta-analysis of safety and efficacy of laparoscopic resection for gastrointestinal stromal tumors of the stomach. Surgical Endoscopy. 29 (2), 355-367 (2015).
- Koh, Y. X., et al. A systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Annals of Surgical Oncology. 20 (11), 3549-3560 (2013).
- Zhou, P. H., et al. Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surgical Endoscopy. 25 (9), 2926-2931 (2011).
- Li, J., et al. Chinese consensus guidelines for diagnosis and management of gastrointestinal stromal tumor. Chinese Journal of Cancer Research. 29 (4), 281-293 (2017).
- Mantese, G. Gastrointestinal stromal tumor: epidemiology, diagnosis, and treatment. Current Opinion in Gastroenterology. 35 (6), 555-559 (2019).
- Karakousis, G. C., et al. Laparoscopic versus open gastric resections for primary gastrointestinal stromal tumors (GISTs): a size-matched comparison. Annals of Surgical Oncology. 18 (6), 1599-1605 (2011).
- Melstrom, L. G., Phillips, J. D., Bentrem, D. J., Wayne, J. D. Laparoscopic versus open resection of gastric gastrointestinal stromal tumors. American Journal of Clinical Oncology. 35 (5), 451-454 (2012).
- Shoji, Y., et al. Optimal minimally invasive surgical procedure for gastric submucosal tumors. Gastric Cancer. 21 (3), 508-515 (2018).
- Hiki, N., et al. Laparoscopic endoscopic cooperative surgery. Digestive Endoscopy. 27 (2), 197-204 (2015).
- Ntourakis, D., Mavrogenis, G. Cooperative laparoscopic endoscopic and hybrid laparoscopic surgery for upper gastrointestinal tumors: Current status. World Journal of Gastroenterology. 21 (43), 12482-12497 (2015).
- Aisu, Y., Yasukawa, D., Kimura, Y., Hori, T. Laparoscopic and endoscopic cooperative surgery for gastric tumors: Perspective for actual practice and oncological benefits. World Journal of Gastrointestinal Oncology. 10 (11), 381-397 (2018).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved