A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Vascularized Composite Hand Allograft Procurement and Preparation for Distal and Proximal Forearm Allotransplantation: A Stepwise Approach
In This Article
Summary
Here, we present a protocol for procuring and preparing vascularized composite hand allografts during distal or proximal forearm transplantation.
Abstract
Upper limb amputations represent a real medical and surgical challenge. The ideal treatment should restore function, sensation, and body image. At present, neither traditional reconstructions nor prostheses meet all these criteria. However, vascularized composite allografts offer a unique option for restoring form and function satisfactorily despite harmful immunosuppression.
Ideally, donor tissue is procured in excess to repair without tension. The donor upper limb is procured through a fish-mouth incision at the mid-arm level. Then, the brachial artery and vein, median, ulnar, and radial nerve are located and dissected. The biceps, brachioradialis, and triceps muscles are sectioned, and then an osteotomy of the humerus is performed above the elbow. For distal forearm transplantation, the donor upper limb can also be procured below the elbow by disarticulating through the joint.
The brachial artery is cannulated, and the graft is irrigated with a preservative solution. Preparation of the graft then begins with two incisions, anterior and posterior, to raise two lateral skin flaps. A medial skin flap exposes the basilic vein, medial antebrachial cutaneous nerve, medial epicondylar muscles, ulnar nerve, median nerve, brachial artery, and vein. A lateral skin flap, including the cephalic vein, the lateral antebrachial cutaneous nerve, the radial nerve up to its division, the brachioradialis, and the lateral epicondylar muscles, completes graft preparation. In the case of transplantation, cutting guides are attached to the posterior surface of the two forearm bones to perform the osteotomies.
This protocol presents a systematized procedure for procuring and preparing a vascularized forearm composite allograft to ensure optimal results and minimize tissue damage during procurement.
Introduction
Since the first successful hand transplantation by Dubernard in 19981, the medical community has done a lot of research and has made progress on upper extremity vascularized composite allotransplantation (VCA). The main advantage is that VCA provides a unique option to restore form and function compared to traditional prosthetics or reconstructions2,3. Hand VCA is one of the best examples of VCA, comprising many diverse tissues: skin, neurovascular, bone, cartilage, and muscle4. To this date, there have been more upper extremity transplants than any other kind of vascularized composite allotransplantation5. Since there are some publications in the literature about the procurement and the preparation of hand VCA6,7,8,9, we simplified the protocol and gathered the main steps of this procedure.
Upper extremity transplantation is a multiple-step complex reconstructive procedure where surgical rehearsals can decrease ischemia time and complications8,10,11,12. Also, upper extremity transplants should be procured before solid organ procurement, and the hand procurement team needs to be trained and efficient to ensure the solid organs are not jeopardized4,6,11,13. Hence, there is a need for a standardized protocol to reliably procure and prepare an upper extremity vascularized composite allotransplant. As Dr Robert Acland, forefather of modern-day microsurgery, said, "Preparation is the only shortcut you need in surgery."
This protocol details all the processes, from the positioning to the closure of the donor limb during an upper extremity VCA. It explains the steps to procure the graft above the elbow or in a second method through the elbow. The preparation of the procured limb is different according to the level of transplantation: proximal forearm or distal forearm. Both preparations are described in this protocol. This detailed procedure aims to standardize procuring and preparing a vascularized forearm composite allograft, which is of interest both for research and translational studies, as well as in clinical practice, given the increasing number of forearm transplants to ensure optimal results and minimize tissue damage.
Protocol
The Anatomy Laboratory of the Faculty of Medicine of Nice, France, generously provided the specimens and material used for the study. The French National Ethics Committee approved this study (approval number 83.2024), which was conducted following the Helsinki Declaration.
1. Preoperative care
- On a selected deceased organ donor, position the patient supine with the arm abducted on a hand table.
- Apply a tourniquet over the upper donor arm, as proximal as possible.
- Prepare and drape the limb with a pierced sterile drape rolled up distal to the tourniquet.
- Inflate the tourniquet at 100 mmHg above the systolic blood pressure.
2. Donor upper limb procurement above the elbow (mid-humeral transection) (Figure 1)
- Make a circumferential fish mouth incision with a surgical scalpel blade (no 15) at the mid-arm level.
- Raise the volar proximal skin flap using fine needle cautery and a pair of Adson tissue forceps, ligating proximally and dividing the cephalic and basilic veins.
NOTE: Ligate the structures with a 0 braided absorbable suture or hemostatic clips. - Expose, ligate proximally, and divide the brachial artery and veins a few centimeters above the elbow crease.
- Dissect, with scissors, on the medial arm and transect, with a scalpel, the median nerve and the ulnar nerve deep to the medial intermuscular septum.
- Raise the dorsal proximal skin flap using fine needle cautery and a pair of Adson tissue forceps, and clip proximally any superficial veins with hemostatic clips.
- Identify the radial nerve deep to the lateral intermuscular septum. Transect the radial nerve with a scalpel proximal to its branches for brachioradialis (BR), extensor carpi radialis longus (ECRL), and extensor carpi radialis brevis (ECRB).
- Isolate and transect biceps, brachialis, and triceps muscle bellies with a monopolar diathermy.
- Make a transverse humerus osteotomy a few centimeters above the elbow joint with an oscillating saw. Ligate and divide the rest of the neurovascular bundle to detach the limb ( Figure 1).
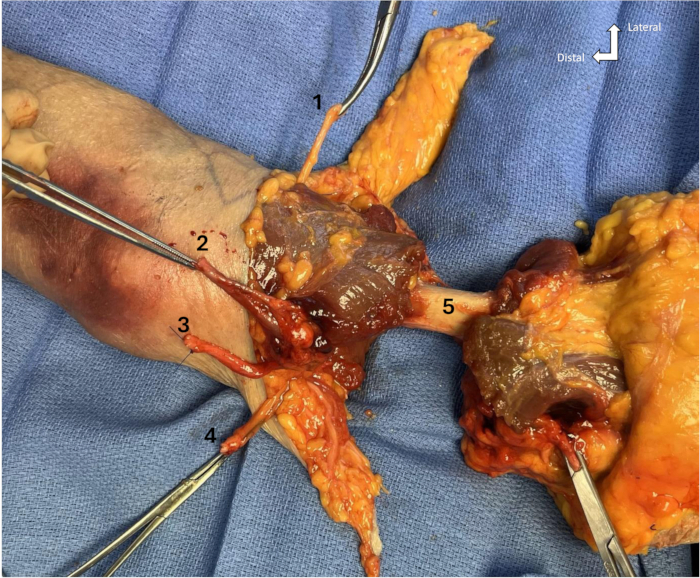
Figure 1: Mid arm with nerves, artery, veins, and muscles transected. (1) Radial nerve, (2) Brachial artery and vein, (3) Median nerve, (4) Ulnar nerve, (5) Humerus diaphysis. Please click here to view a larger version of this figure.
3. Packaging of the graft
- Transfer the limb to the back table for preparation for transport to the recipient center.
- Catheterize the brachial artery with a vascular cannula with a stopcock and secure the cannula in the lumen with 2-0 silk suture ligation.
- Flush the limb via a universal irrigation set and attach it to the stopcock in the brachial artery with 1-3 L of University of Wisconsin (UW) solution at 4 °C to preserve the graft.
NOTE: Perfuse until clear venous outflow. Note the dominant venous system comparing the returning fluid velocity in the superficial and deep veins. Other preservation fluids, such as histidine-tryptophanketoglutarate (HTK) infused with 5000 units of unfractionated heparin, can be used.- Disconnect the irrigation set and close the stopcock.
- Wrap the limb in saline-moistened sterile towels, place it in a sealed sterile bag, and label it. Apply a second empty sterile bag, then put it in a third sterile bag filled with ice water as per standard solid organ transplantation (SOT) protocol.
- Place bags in the wheeled cooler and label the cooler.
4. Management of the donor residual limb
- Remove the tourniquet after the recovery of all solid organs.
- Complete a careful hemostasis using bipolar diathermy. Close the fish mouth incision on the arm with running or interrupted subdermal sutures followed by staples for a water-tight seal.
- Attach the cosmetic prosthesis to the donor residual limb and roll over the sleeve of the proximal segment of the prosthesis for restoration of form.
5. Donor upper limb procurement through the elbow (elbow transection)
NOTE: Same preoperative care, with the tourniquet at mid-arm.
- Mark the medial and lateral epicondyles to draw the fish mouth incision below the elbow joint.
- Incise with a surgical scalpel blade (no 15) and raise the volar skin flap using fine needle cautery and a pair of Adson tissue forceps, ligating proximally and dividing the cephalic and basilic veins.
- Incise the antebrachial fascia with a scalpel, identify, then transect with scissors the brachial artery and the median nerve under the lacertus fibrosis, ulnar to the biceps brachii tendon.
NOTE: For proximal forearm transplantation, transect the median nerve proximal to the origin of the pronator teres branch. - Transect the pronator teres and forearm flexor mass through their proximal bellies with monopolar diathermy.
NOTE: For proximal forearm transplantation, the flexor and extensor origins are dissected free along with the periosteum of medial and lateral epicondyles and not transected. This provides strong tissue for reinsertion to the recipient bone. - Identify and transect with scissors the ulnar nerve where it exits the cubital tunnel.
NOTE: For proximal forearm transplantation, transect the ulnar nerve proximal to the origin of the flexor carpi ulnaris branch. - Transect the elbow flexors with monopolar diathermy near their distal insertion to expose the ulnar elbow joint capsule and the proximal ulna.
- Transect the mobile wad and the common extensor mass in their proximal bellies to identify the radial nerve and expose the radial elbow joint capsule. Transect the radial nerve proximal to its division in superficial and deep branches.
NOTE: For proximal forearm transplantation, transect the radial nerve proximal to the origin of brachioradialis, extensor carpi radialis longus, and extensor carpi radialis brevis branches. - Incise the anterior elbow joint capsule with a scalpel. Fully flex the elbow and raise the dorsal skin flap using fine needle cautery and a pair of Adson tissue forceps.
- Isolate and transect the triceps tendon with a scalpel, then incise the posterior elbow joint capsule to disarticulate the elbow and detach the limb fully.
NOTE: The same packaging of the graft and management of the donor residual limb are needed.
6. Preparation of the graft for proximal forearm transplantation (Figure 2 and Figure 3)
NOTE: Tag each structure with a rectangular piece of Esmarch bandage marked with indelible ink markers and secured with 2-0 silk sutures or sterilized titanium named tags.
- Make a longitudinal median volar incision with a surgical scalpel blade (no 15) from proximal to distal (to the mid-forearm level) and a longitudinal dorsal incision onto the shaft of the ulna up to 14 cm below the olecranon.
- Raise the medial skin flap using fine needle cautery and a pair of Adson tissue forceps and dissect off the skin for some distance the basilic vein and the medial antebrachial cutaneous nerve with scissors.
- Raise the lateral skin flap and dissect the cephalic vein and the lateral antebrachial cutaneous nerve.
NOTE: The medial and lateral flaps are raised like this to interdigitate with the recipient limb's volar and dorsal skin flaps. - Dissect with scissors distally the ulnar nerve until the origin of the flexor carpi ulnaris branch and the median nerve until the origin of the pronator teres branch.
- Dissect the radial nerve with scissors and identify the BR, ECRL, and ECRB motor branches. Tag the branches and transect them at their origins from the radial nerve. Separately tag the superficial and the deep branch of the radial nerve.
NOTE: On the recipient residual limb, radial nerve branches to BR, ECRL, and ECRB are transected close to the point of muscle entry so they can be later coapted to the donor ECRL, ECRB, and BR branches.
- Dissect the radial nerve with scissors and identify the BR, ECRL, and ECRB motor branches. Tag the branches and transect them at their origins from the radial nerve. Separately tag the superficial and the deep branch of the radial nerve.
- Dissect distally the brachial artery and its vena comitantes up to the division in radial and ulnar vessels (Figure 2).
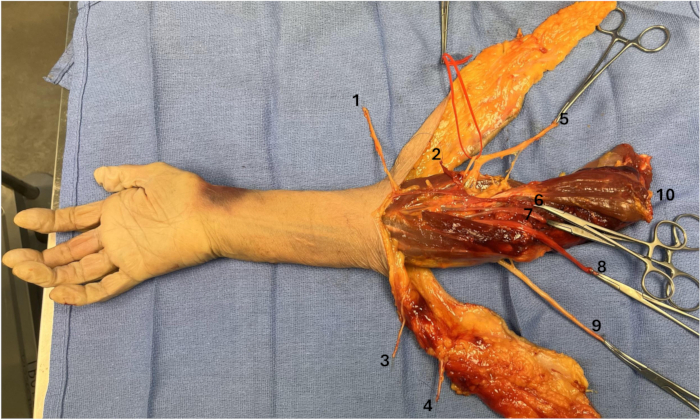
Figure 2: Neurovascular structures at the proximal forearm. (1) Lateral antebrachial cutaneous nerve, (2) Cephalic vein, (3) Medial antebrachial cutaneous nerve, (4) Basilic vein, (5) Radial nerve with its branches for BR, ECRL, ECRB, deep motor branch and superficial sensitive branch in a red loop, (6) Brachial veins, (7) Brachial artery, (8) Median nerve, (9) Ulnar nerve with its branch for FCU, (10) Biceps brachialis. Please click here to view a larger version of this figure.
- Elevate with a scalpel the origins of flexor and extensor muscle mass off the medial and lateral epicondyles in a subperiosteal plan. Elevate the brachioradialis from its humeral insertion.
- Dissect the radius distally from the biceps tendon insertion with a scalpel to allow plate fixation.
- Reflect the brachialis proximally and the forearm muscle mass distally from the proximal ulna by anterior and posterior subperiosteal dissection.
NOTE: The biceps tendon insertion is an essential landmark for orientation and osteotomy. Be careful to preserve the deep branch of the radial nerve, and if necessary, split the interosseous membrane proximally. - Continue the elevation, with a scalpel, of forearm muscles from the radius and ulna until three holes of the dynamic compression plates can be accommodated beyond the planned osteotomies (Figure 3).
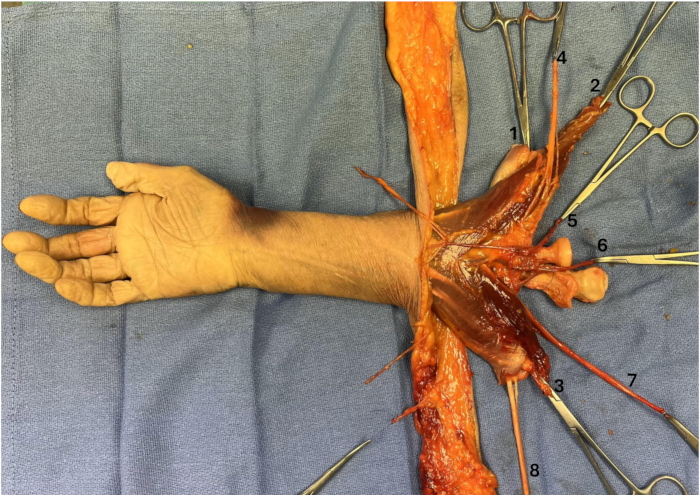
Figure 3: Forearm muscle mass elevated. (1) Extensor mass, (2) Brachioradialis, (3) Flexor mass, (4) Radial nerve, (5) Brachial veins, (6) Brachial artery, (7) Median nerve, (8) Ulnar nerve. Please click here to view a larger version of this figure.
7. Preparation of the graft for distal forearm transplantation (Figure 4 and Figure 5)
NOTE: Tag each structure with a rectangular piece of Esmarch bandage marked with indelible ink markers and secured with 2-0 silk sutures or sterilized titanium named tags.
- Make mid-axial volar and dorsal incisions up to wrist level distally using a surgical scalpel blade (no 15). Release the carpal tunnel with the volar incision.
- Raise radial and ulnar skin flaps with the antebrachial fascia using fine needle cautery and a pair of Adson tissue forceps. Preserve the skin perforators of the distal forearm on both flaps.
- Dissect off the radial skin flap, the cephalic vein, and the lateral antebrachial cutaneous nerve with scissors. Dissect off the ulnar skin flap, the basilic vein, and the medial antebrachial cutaneous nerve.
- Identify and excise the brachioradialis with fine needle cautery and dissect the radial sensory nerve underneath.
- Elevate the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) by opening the first compartment with a scalpel.
NOTE: Skeletonize all tendons with a scalpel by excising the muscle to leave the tendinous part as long as possible for repair.- Isolate ECRL and ECRB, and dissect the extensor pollicis longus (EPL) free from its sheath.
- Identify the extensor indicis proprius (EIP), extensor digitorum communis (EDC), and extensor digiti minimi (EDM). Elevate the extensor carpi ulnaris (ECU) (Figure 4).
NOTE: EIP, EDC, and EDM can be sutured together if individual repair is not possible during transplantation.
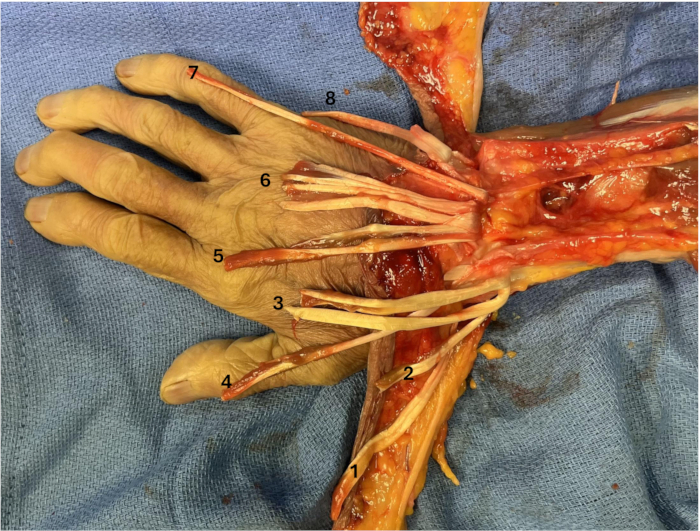
Figure 4: Extensor tendons dissected. (1) APL, (2) EPB, (3) ECRL and ECRB, (4) EPL, (5) EIP, (6) EDC, (7) EDM, (8) ECU. Please click here to view a larger version of this figure.
- Dissect the radial artery and its vena comitantes using scissors and Adson tissue forceps.
- Isolate the flexor carpi radialis (FCR) and excise the palmaris longus with a scalpel. Dissect the median nerve.
- Identify each tendon of flexor digitorum superficialis (FDS), the flexor pollicis longus (FPL) and the 4 tendons of flexor digitorum profundus (FDP). Elevate the flexor carpi ulnaris (FCU).
NOTE: FDS can be sutured together, and the same is true for FDP if individual reparation is not possible during transplantation. - Dissect carefully with scissors the ulnar artery and nerve to identify the dorsal sensory branch of the ulnar nerve.
- Excise the pronator quadratus (PQ) with fine needle cautery. Expose the volar side of the radius and ulnar side of the ulna until three holes of the osteosynthesis plates can be accommodated beyond the planned osteotomies (Figure 5).
NOTE: Be careful with the anterior interosseous artery on the interosseous membrane at this level.
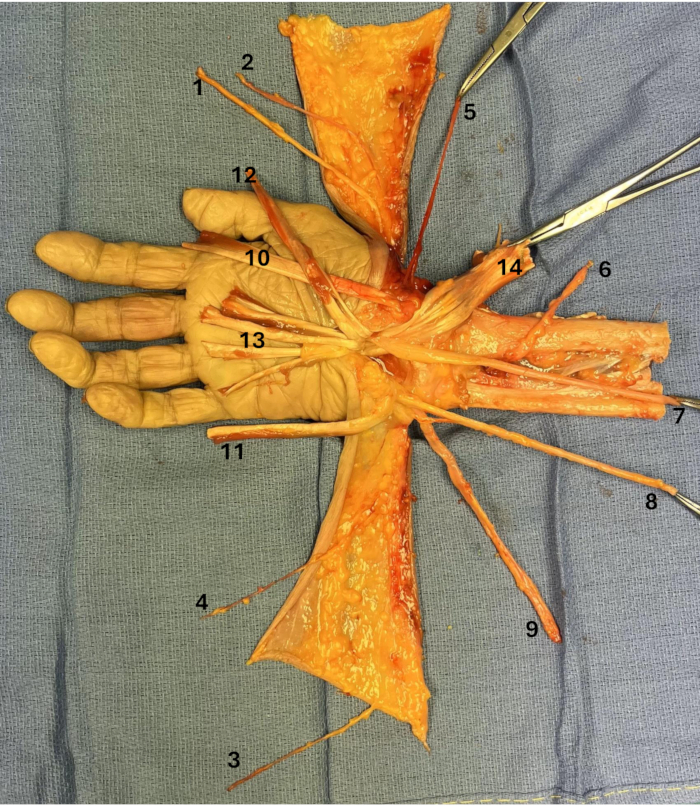
Figure 5: Flexor tendons and neurovascular bundles dissected. (1) Radial sensory branch, (2) Cephalic vein, (3) Medial antebrachial cutaneous nerve, (4) Basilic vein, (5) Radial artery, (6) Anterior interosseous artery, (7) Median nerve, (8) Ulnar nerve with its dorsal sensitive branch, (9) Ulnar artery, (10) FCR, (11) FCU, (12) FPL, (13) FDS, (14) FDP. Please click here to view a larger version of this figure.
Results
At the end of this protocol, the donor limb should be ready for transplantation on the receiving residual limb. The radius and ulna are sufficiently exposed for the osteosynthesis with a 3.5-mm locking compression plate14,15,16 or 2.7-mm volar locking distal radius and ulna plates in distal forearm transplant. The brachial or radial and ulnar arteries are dissected depending on the level, allowin...
Discussion
This protocol presents some critical steps. First, the skin flap incisions are marked. The goal is to properly match the flaps to ensure sufficient tissue to close over the bulky tendon anastomoses without skin surplus, which can lead to bulky skin adaptation. Furthermore, distal tip perfusion of the flaps should be ensured. To help in this surgical planning, three-dimensional (3D) stereophotogrammetry and 3D-printed skin incision guides can be useful, as Hummelink et al.23 described. The rad...
Disclosures
The authors have no disclosures.
Acknowledgements
The authors would like to thank the individuals who donated their bodies to facilitate the anatomical research.
Materials
| Name | Company | Catalog Number | Comments |
| 11.5” medium premium surgiclip II auto suture vessel clip applier | Covidien | ||
| 2-0 silk suture | N/A | N/A | |
| Adson forceps | MPM | 106-2112A | |
| Bipolar coagulation forceps | Olsen | 20-1320I | |
| Custodiol HTK solution for limb perfusion | Essential Pharmaceuticals Inc. | off-label use | |
| Cysto/Bladder irrigation set | Baxter Healthcare Corp. | 2C4040 | |
| Disposable scalpel #15 | Sklar | ||
| DLP 3 mm vessel cannula blunt tip | Medtronic Inc | https://www.medline.com/product/Medtronic-DLP-Vessel-Cannulae/Cannulas-Tubing/Z05-PF24250?question=vessel%20cannula | |
| Fine needle cautery | Cormedica | ||
| Forceps dilators | WPI | 15910 | |
| IV stopcock | N/A | N/A | |
| Micro scissors | WPI | 504492 | |
| Monopolar diathermy | Medtronic Inc | Valleylab | |
| Oscillating saw | GPC Medical | https://www.gpcmedical.com/1015/BTD1138/battery-operated-oscillating-saw.html | |
| Saline solution 0,9% | GenDepot | S0600-101 | |
| Sterile Esmarch bandage | N/A | N/A | |
| Sterile indelible ink markers | N/A | N/A | |
| Strabismus scissors | Surtex | 102-4109 | |
| Surgical marking pen | Cardinal health | 212PR | |
| Sutures Ethilon 4.0 | Ethicon | 1667G | |
| Syringue 10 mL | Agilent | 9301-6474 | |
| Three sterile procurement plastic bags, and three sterile zip ties | N/A | N/A | |
| Tissue forceps | MPM | 106-0511 | |
| Vessel loop | Deroyal | 30-711 |
References
- Dubernard, J. M., et al. Human hand allograft: report on first 6 months. Lancet. 353 (9161), 1315-1320 (1999).
- Wells, M. W., Rampazzo, A., Papay, F., Gharb, B. B. Two decades of hand transplantation: a systematic review of outcomes. Ann Plast Surg. 88 (3), 335-344 (2022).
- Kumnig, M., Kobler, C., Zaccardelli, A., Brandacher, G., Talbot, S. G. Advancing vascularized composite allotransplantation: essential factors for upper extremity transplant program development. Front Transplant. 3, 1406626 (2024).
- Schuind, F., Abramowicz, D., Schneeberger, S. Hand transplantation: the stateoftheart. J Hand Surg Eur. 32 (1), 2-17 (2007).
- Hernandez, J. A., et al. OPTN/SRTR 2022 annual data report: vascularized composite allograft. Am J Transplant. 24 (2), S534-S556 (2024).
- Mendenhall, S. D., et al. Technique for rapid hand transplant donor procurement through the elbow. Hand. 16 (3), 391-396 (2021).
- Mendenhall, S. D., Brown, S., BenAmotz, O., Neumeister, M. W., Levin, L. S. Building a hand and upper extremity transplantation program: lessons learned from the first 20 years of vascularized composite allotransplantation. Hand. 15 (2), 224-233 (2020).
- Cetrulo, C. L., Kovach, S. J. Procurement of hand and arm allografts. Tech Hand Up Extrem Surg. 17 (4), 232-238 (2013).
- Dalla Pozza, E., et al. Procurement of extended vascularized skin flaps from the donor enables hand transplantation in severe upper extremity burns: an anatomical study. Plast Reconstr Surg. 142 (2), 425-437 (2018).
- Gittings, D. J., et al. Preparation is the only shortcut you need in surgery: a guide to surgical rehearsals for hand and upper extremity transplantation. Tech Hand Up Extrem Surg. 22 (4), 137-140 (2018).
- Hausien, O., et al. Surgical and logistical aspects of donor limb procurement in hand and upper extremity transplantation. Vasc Compos Allotransplantation. 1 (1-2), 31-41 (2014).
- Griffin, J. M., et al. Using team science in vascularized composite allotransplantation to improve team and patient outcomes. Front Psychol. 13, 935507 (2022).
- Margreiter, R., et al. A doublehand transplant can be worth the effort. Transplantation. 74 (1), 85-90 (2002).
- Hartzell, T. L., et al. Surgical and technical aspects of hand transplantation: is it just another replant. Hand Clin. 27 (4), 521-530 (2011).
- Cavadas, P. C., Ibáñez, J., Thione, A., Alfaro, L. Bilateral transhumeral arm transplantation: result at 2 years. Am J Transplant. 11 (5), 1085-1090 (2011).
- Haddock, N. T., Chang, B., Bozentka, D. J., Steinberg, D. R., Levin, L. S. Technical implications in proximal forearm transplantation. Tech Hand Up Extrem Surg. 17 (4), 228-231 (2013).
- Sharma, M., et al. First two bilateral hand transplantations in India (part 2): technical details. Indian J Plast Surg. 50 (2), 153-160 (2017).
- Tawa, P., Gurunian, R., Rampazzo, A., Papay, F., Bassiri Gharb, B., et al. Upper extremity transplantation: the Massachusetts General Hospital experience. Reconstructive Transplantation. , 231-238 (2023).
- Brown, S. H. M., et al. Mechanical strength of the sidetoside versus Pulvertaft weave tendon repair. J Hand Surg. 35 (4), 540-545 (2010).
- Schneeberger, S., et al. First forearm transplantation: outcome at 3 years. Am J Transplant. 7 (7), 1753-1762 (2007).
- Sharma, M., et al. Indian subcontinent's first proximal forearm level double upper extremity transplantation. Indian J Plast Surg. 52 (3), 277-284 (2019).
- Cavadas, P. C., Landin, L., Ibañez, J. Bilateral hand transplantation: result at 20 months. J Hand Surg Eur. 34 (4), 434-443 (2009).
- Hummelink, S., Kruit, A. S., Hovius, S. E. R., Ulrich, D. J. O. Designing and utilizing 3Dprinted skin incision guides during the first Dutch bilateral handarm transplantation. J Plast Reconstr Aesthet Surg. 74 (11), 2965-2968 (2021).
- Wood, M. D., Kemp, S. W. P., Weber, C., Borschel, G. H., Gordon, T. Outcome measures of peripheral nerve regeneration. Ann Anat. 193 (4), 321-333 (2011).
- Serra López, V. M., et al. . Hand Allotransplantation: The Penn Experience. In Reconstructive Transplantation. , (2023).
- McClelland, B., et al. Proximal forearm transplantation for below elbow amputations: rationale and surgical technique. Vasc Compos Allotransplantation. 2 (1), 26-28 (2015).
- Jablecki, J., Kaczmarzyk, L., Patrzalek, D., Domanasiewicz, A., Chełmoński, A. A detailed comparison of the functional outcome after midforearm replantations versus midforearm transplantation. Transplant Proc. 41 (2), 513-516 (2009).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved