A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Oxygenation-sensitive Cardiac MRI with Vasoactive Breathing Maneuvers for the Non-invasive Assessment of Coronary Microvascular Dysfunction
In This Article
Erratum Notice
Summary
The assessment of microvascular function by oxygenation-sensitive cardiac magnetic resonance imaging in combination with vasoactive breathing maneuvers is unique in its ability to assess rapid dynamic changes in myocardial oxygenation in vivo and, thus, may serve as a critically important diagnostic technique for coronary vascular function.
Abstract
Oxygenation-sensitive cardiac magnetic resonance imaging (OS-CMR) is a diagnostic technique that uses the inherent paramagnetic properties of deoxyhemoglobin as an endogenous source of tissue contrast. Used in combination with standardized vasoactive breathing maneuvers (hyperventilation and apnea) as a potent non-pharmacologic vasomotor stimulus, OS-CMR can monitor changes in myocardial oxygenation. Quantifying such changes during the cardiac cycle and throughout vasoactive maneuvers can provide markers for coronary macro- and microvascular function and thereby circumvent the need for any extrinsic, intravenous contrast or pharmacologic stress agents.
OS-CMR uses the well-known sensitivity of T2*-weighted images to blood oxygenation. Oxygenation-sensitive images can be acquired on any cardiac MRI scanner using a modified standard clinical steady-state free precession (SSFP) cine sequence, making this technique vendor-agnostic and easily implemented. As a vasoactive breathing maneuver, we apply a 4-min breathing protocol of 120 s of free breathing, 60 s of paced hyperventilation, followed by an expiratory breath-hold of at least 30 s. The regional and global response of myocardial tissue oxygenation to this maneuver can be assessed by tracking the signal intensity change. The change over the initial 30 s of the post-hyperventilation breath-hold, referred to as the breathing-induced myocardial oxygenation reserve (B-MORE) has been studied in healthy people and various pathologies. A detailed protocol for performing oxygen-sensitive CMR scans with vasoactive maneuvers is provided.
As demonstrated in patients with microvascular dysfunction in yet incompletely understood conditions, such as inducible ischemia with no obstructive coronary artery stenosis (INOCA), heart failure with preserved ejection fraction (HFpEF), or microvascular dysfunction after heart transplantation, this approach provides unique, clinically important, and complementary information on coronary vascular function.
Introduction
Oxygenation-sensitive cardiac magnetic resonance imaging (OS-CMR) uses the inherent paramagnetic properties of deoxyhemoglobin as an endogenous source of MR contrast1,2,3. Used in combination with standardized vasoactive breathing maneuvers (hyperventilation and apnea) as a potent non-pharmacologic vasomotor stimulus, OS-CMR can monitor changes in myocardial oxygenation as a marker for vascular function, thereby circumventing the need for any extrinsic, intravenous contrast or pharmacologic stress agents 4,5,6.
Breathing maneuvers, including breath-holds and hyperventilation, are highly effective vasoactive measures to alter vasomotion and, because of their safety and simplicity, are ideal for controlled endothelial-dependent vasomotion as part of a diagnostic procedure. Studies have shown an added effectiveness when combining hyperventilation with a subsequent breath-hold4,7, as during such a protocol, the vasoconstriction (through the associated decrease of blood carbon dioxide) is followed by vasodilation (increase of blood carbon dioxide); thus, a healthy vascular system transitions through the entire range from vasoconstriction to vasodilation with a strong increase in myocardial blood flow, which in turn increases myocardial oxygenation and, thus, the observable signal intensity in OS-CMR images. The use of cine images for the acquisition also allows for cardiac phase-resolved results with a better signal-to-noise ratio when compared to adenosine infusion8.
Breathing maneuvers can replace pharmacological stress agents for inducing vasoactive changes that can be used for assessing coronary vascular function. This not only reduces patient risk, logistical efforts, and associated costs but also helps in providing results that are clinically more meaningful. Pharmacologic stress agents such as adenosine trigger an endothelium-dependent response and, thus, reflect endothelial function itself. Such specific assessment of endothelial function so far was only possible by an intracoronary administration of acetylcholine as an endothelial-dependent vasodilator. This procedure, however, is highly invasive2,9 and, therefore, rarely performed.
Lacking access to direct biomarkers, several diagnostic techniques have used surrogate markers such as tissue uptake of an exogenous contrast agent. They are limited by the need for one or two intravenous access lines, contraindications such as severe kidney disease or atrioventricular block, and the need for the physical presence of staff with training in managing potentially severe side effects10,11. The most significant limitation of current imaging of coronary function, however, remains that myocardial perfusion as a surrogate marker does not reflect myocardial tissue oxygenation as the most important downstream consequence of vascular dysfunction2.
OS-CMR with vasoactive breathing maneuvers has been utilized to evaluate vascular function in numerous scenarios, including healthy individuals, macrovascular disease in patients with coronary artery disease (CAD), as well as microvascular dysfunction in patients with obstructive sleep apnea (OSA), ischemia with no obstructive coronary artery stenosis (INOCA), after heart transplantation, and heart failure with preserved ejection fraction (HFpEF)4,7,12,13,14,15,16. In a CAD population, the protocol for the breathing-induced myocardial oxygenation reserve (B-MORE) as derived from OS-CMR was proven to be safe, feasible, and sensitive in identifying an impaired oxygenation response in myocardial territories perfused by a coronary artery with a significant stenosis13.
In microvascular dysfunction, OS-CMR demonstrated a delayed myocardial oxygenation response in patients with obstructive sleep apnea, and a blunted B-MORE was found in patients with HFpEF and following heart transplantation12,14,16. In women with INOCA, the breathing maneuver led to an abnormally heterogeneous myocardial oxygenation response, highlighting the advantage of the high spatial resolution of OS-CMR15. This paper reviews the rationale and methodology for performing OS-CMR with vasoactive breathing maneuvers and discusses its clinical utility in the assessment of vascular pathophysiology in patient populations with microvascular dysfunction, specifically as they relate to endothelial dysfunction.
The physiological context of breathing-enhanced oxygenation-sensitive MRI
Under normal physiologic conditions, an increase in oxygen demand is matched by an equivalent increase in oxygen supply through increased blood flow, resulting in no change in local deoxyhemoglobin concentration. In contrast, induced vasodilation leads to "excess" inflow of oxygenated blood without a change in oxygen demand. Consequently, more of the tissue hemoglobin is oxygenated, and thus, there is less deoxyhemoglobin, leading to a relative increase in OS-CMR signal intensity4,17. If vascular function is compromised, it cannot properly respond to an altered metabolic demand or stimulus to augment myocardial blood flow.
In the setting of a stimulus to elicit vasomotion, such as paced hyperventilation eliciting vasoconstriction or a long breath-hold eliciting carbon dioxide-mediated vasodilation, impaired vasomotor activity would result in a relative increase in local deoxyhemoglobin concentration compared with other regions, and, subsequently, a reduced change in OS-CMR signal intensity. In the setting of inducible ischemia, impaired vascular function would result in increased local demand not met by a local increase in myocardial blood flow even in the absence of epicardial coronary artery stenosis. In OS-CMR images, the net local increase in deoxyhemoglobin concentration leads to a decrease in local signal intensity2,18,19,20.
Attenuated vascular smooth muscle relaxation in response to endothelium-dependent and -independent vasodilators (including adenosine) has been demonstrated in patients with coronary microvascular dysfunction21,22,23,24,25,26,27. Endothelial-independent dysfunction is thought to be due to structural abnormalities from microvascular hypertrophy or surrounding myocardial pathology. In contrast, endothelial dysfunction results in both inadequate vasoconstriction and impaired (endothelium-dependent) vasorelaxation, typically caused by a loss of nitric oxide bioactivity in the vessel wall21,28. Endothelial dysfunction has been implicated in the pathogenesis of a number of cardiovascular diseases, including hypercholesterolemia, hypertension, diabetes, CAD, obstructive sleep apnea, INOCA, and HF23,24,28,29,30,31,32. In fact, endothelial dysfunction is the earliest manifestation of coronary atherosclerosis33. The imaging of endothelial function has very strong potential, given its role as a significant predictor of adverse cardiovascular events and long-term outcomes, with profound prognostic implications in cardiovascular disease states23,29,30,31,34,35.
In contrast to perfusion imaging, the breathing-induced myocardial oxygenation reserve (B-MORE), defined as the relative increase in myocardial oxygenation during a post-hyperventilation breath-hold allows for visualizing the consequences of such a vasoactive trigger on global or regional oxygenation itself2,36. As an accurate downstream marker of vascular function, B-MORE can, therefore, not only identify vascular dysfunction but also actual inducible ischemia, indicating a more severe local perfusion or oxygenation problem18,19,37. This is achieved through the ability of OS-CMR to visualize the relative decrease in deoxygenated hemoglobin, which is abundant in the capillary system of the myocardium, which itself represents a significant proportion of myocardial tissue24.
OS-CMR sequence
The magnetic resonance imaging (MRI) sequence used for OS-CMR imaging is a prospectively gated, modified, balanced, steady-state, free precession (bSSFP) sequence acquired in two short-axis slices. This bSSFP sequence is a standard clinical sequence available (and modifiable) on all MRI scanners that perform cardiac MRI, making this technique vendor-agnostic and easily implemented. In a regular bSSFP cine sequence, echo time, repetition time, and flip angle are modified to sensitize the resulting signal intensity to the BOLD effect and, thus, create an oxygenation-sensitive sequence. This approach, a T2-prepared bSSFP readout, has previously been shown to be suitable for acquiring oxygenation-sensitive images with a higher signal-to-noise ratio, higher image quality, and faster scan times when compared to previous gradient echo techniques used for BOLD imaging38. Performing breathing-enhanced OS-CMR with this approach can be applied with very few, mild side effects (Table 1). Of note, more than 90% of participants complete this protocol with sufficiently long breath-hold times4,12,13,16.
Access restricted. Please log in or start a trial to view this content.
Protocol
All MRI scans utilizing OS-CMR with vasoactive breathing maneuvers should be performed in compliance with local institutional guidelines. The protocol outlined below has been used in studies approved by several institutional human research ethics committee. Written consent was obtained for all the human participant data and results described in this protocol and manuscript.
1. Broad overview
- Vary the inclusion and exclusion criteria depending on the study population of interest. Use the following general, common exclusion criteria for an OS-CMR with vasoactive breathing maneuvers protocol: general MRI contraindications (e.g., MRI-incompatible devices such as pacemakers or defibrillators, implanted material, or foreign bodies), consumption of caffeine or vasoactive medication in the 12 h prior to the MRI, and age <18 years.
- First, acquire the standard clinical localizer scout and ventricular structure and function images before acquiring the OS acquisitions. Use the bSSFP long-axis cine images to plan the slice positioning of the OS acquisitions.
NOTE: A review of standardized clinical CMR protocols is described elsewhere39. - Baseline breath-hold
- Acquire the first OS-CMR series as a short, baseline breath-hold acquisition to assess image quality and slice location, check for artifacts, as well as serve as a signal intensity baseline.
- Perform a short (~10 s), single cardiac cycle acquisition after the participant has been breathing normally. Ensure that the breath-hold is done on end-expiration.
- Continuous acquisition with vasoactive breathing maneuver
- Acquire the second OS-CMR series as a 2 min, continuous acquisition comprised of a short 15 s breath hold and 1 min of paced hyperventilation, followed by a voluntary, maximal breath hold (~45 s). As the continuous acquisition obtains multiple cardiac cycles over 2 min, modify one additional parameter (the number of cardiac cycles acquired by the acquisition) to make this series a repeated-measures acquisition.
NOTE: The minimum required breath-hold length is 30 s, although a breath-hold of 45-60 s is considered the standard. - Convey the instructions for the vasoactive breathing maneuver to the participants in the MRI scanner by manually directing the participant throughout the breathing maneuver through a microphone connected to the MRI speaker system or through a prerecorded .mp3 file (Supplemental File 1) that can be played for the participant through the MRI speaker system.
- Start the breathing maneuver with a short 15 s, and end the expiration breath hold to acquire one cardiac cycle. Then guide the participant through paced breathing with the use of audible beeps from a metronome at a frequency of 30 breaths/min (one beep indicates breathing in, one beep indicates breathing out). At the 55 s mark of hyperventilation, give a final voice command to "take a deep breath in and then breathe out and hold your breath" to ensure that the breath-hold is performed at an end-expiration level.
NOTE: The change in blood CO2 is much more pronounced with the breath-hold at end-expiration (the lung surface is smaller, minimizing the residual diffusion of CO2 into the alveoli).
- Acquire the second OS-CMR series as a 2 min, continuous acquisition comprised of a short 15 s breath hold and 1 min of paced hyperventilation, followed by a voluntary, maximal breath hold (~45 s). As the continuous acquisition obtains multiple cardiac cycles over 2 min, modify one additional parameter (the number of cardiac cycles acquired by the acquisition) to make this series a repeated-measures acquisition.
- Image analysis
- To measure the B-MORE, consider the first end-systolic image during breath-hold as time 0 s. Compare the global or regional signal intensity values of the end-systolic image acquired closest to the 30 s time point of the breath-hold to the image signal intensity at the 0 s time point. Report BMORE as a percent change in signal intensity at 30 s compared to time 0 s of the breath-hold.
2. Pre-scan procedure
- Ensure that every participant passes the MRI safety and compatibility questionnaire of the local institution (MRI General Contraindication form), which should include questions on past medical and surgical history and identify the presence of any implant, device, or metallic foreign body inside or at the surgical site of the participant40.
- Obtain a pregnancy test, if applicable.
- Verify that the patient has abstained from vasoactive medication and caffeine in the 12 h prior to the MRI scan.
- Show the participant the instructional breathing maneuver video (Supplemental Video S1).
- Perform a practice session of 60 s of paced hyperventilation followed by a maximal voluntary breath-hold with every participant outside of the MRI scanning room and provide feedback on the performance of the hyperventilation.
- Instruct the participants that they can simply resume breathing when they have a strong urge to do so.
NOTE: See the discussion for points to note and provide feedback on to the participants.
3. MRI acquisition of oxygenation-sensitive sequences
- Modify three parameters from the standard bSSFP sequence on the MRI console: increase repetition time (TR), increase echo time (TE), decrease flip angle (FA).
NOTE: The modified values are dependent on THE MRI scanner field strength (Table 2). Increasing TR and TE and decreasing FA results in an increase in T2* or oxygenation sensitivity of the MRI sequence. These modifications will then result in an increase in bandwidth and base resolution of the sequence. - Create two OS series, a baseline (labeled: OS_base) and the continuous acquisition during which the breathing maneuver is performed (labeled: OS_cont_acq). Leave the baseline OS sequence unchanged. In the OS continuous acquisition, increase the repeated measures from 1 to ~15-40 (depending on the scanner type). Increase the number of cardiac cycles (measures) until the acquisition time is ~2.5 min.
NOTE: Two OS-CMR sequences are needed: OS baseline acquisition and OS continuous acquisition with vasoactive breathing maneuvers. The following sections describe these steps.
4. OS baseline acquisition
- For slice prescription, plan in an end-systolic still frame of a long axis view (two- or four-chamber image). Prescribe two short-axis slices-one at the mid-to-basal and the other at the mid-to-apical ventricular level. See the discussion for points to consider regarding slice location.
- Sequence parameter adjustments
- Adjust the sequence parameters as needed for a given participant. See Table 3 for sequence parameters than can or cannot be changed.
- Adjust the average gap/spacing between slices based on the size of the participant's heart and ensure proper slice location.
- Adjust the field of view to avoid wrap artifacts if necessary. Make every effort to keep the field of view between 360 mm and 400 mm.
- Shim volume
- Adjust the shim volume to be tight around the left ventricle in both the long- and short-axis views.
- Sequence acquisition
- Approve the sequence and run it during the end-expiration breath-hold. Ensure that this baseline OS sequence lasts ~10 s, based on the heart rate and MRI scanner.
- Image quality check
- Check both slices of the acquired series-look for any respiratory motion, poor slice location, or the presence of artifacts. Repeat the baseline OS sequence until adequate image quality has been obtained.
- For troubleshooting, if the slice location is too basal or too apical, adjust the prescribed slice location to be closer to the mid-ventricular level. If there is an artifact present, follow the steps below:
- Check the phase encoding direction.
- Make the field of view larger.
- Adjust the shim volume around the left ventricle.
5. OS continuous acquisition with vasoactive breathing maneuvers
NOTE: Ensure that every participant has been instructed about the proper performance of the breathing maneuver before they are in the MRI scanner (see section 2).
- Sequence planning
- If possible, copy slice position and adjust volume from the OS baseline image or duplicate the baseline OS sequence and, in repeated measurements, increase from 1 to ~15-40 (or close to 2.5 min acquisition time).
- Verify the image and slice positioning, and then capture cycle.
- If possible, open the live stream window.
- In the control room, plug a device with the breathing maneuver instructions .mp3 file into the auxiliary input or prepare to hold it over the microphone projecting into the MRI scanner. Alternatively, manually guide the participant through the breathing maneuver using a stopwatch for timing and verbally provide instructions through the microphone connected to the MRI speaker system.
- Sequence acquisition
- Simultaneously press play for the OS Continuous Acquisition sequence on the MRI scanner and play for the .mp3 breathing instruction file or start the stopwatch if the participant is being manually instructed.
- If manually guiding the participant through the breathing maneuvers, instruct them to breathe in and breathe out, then hold their breath for 15 seconds (for the short breath-hold), and start hyperventilating as soon as they hear the metronome beep.
- Notify the participant at the 40 s mark of hyperventilation (2:40 on the stopwatch).
- At the 55 s time point of hyperventilation (2:55 on the stopwatch), instruct the participant to "take a deep breath in, breathe out, and hold your breath".
NOTE: The free breathing and hyperventilation images will have motion artifacts. This is expected. However, there should not be any motion artifacts during the breath-hold. It is critically important that the breath-held images are acquired after exhalation (comfortable end-expiratory position). Only a breath-hold after exhalation leads to the rapid increase of blood CO2 during the first 30 seconds of the subsequent breath-hold, with the associated change of coronary blood flow and myocardial oxygenation. - Monitor the participant's performance of the paced hyperventilation through the control room window or MRI scanner camera to ensure adequate performance of deep breathing. If bellows are used, then monitor the amplitude peaks on the respiratory gating viewer. If hyperventilation is not being adequately performed after initial guidance, abort the acquisition and repeat the OS continuous acquisition sequence.
- Monitor for any small breaths taken by participants throughout the breath-hold. Do this by monitoring the tracing of a respiration belt on the MRI console or visually through the window/camera.
- Once the participant starts breathing at the end of the breath-hold, stop the acquisition.
- After the end of the acquisition, ask the participant if they experienced any adverse effects and allow the participant to breathe normally for 3 min.
- Troubleshooting: repeat acquisition
- If the breathing maneuvers need to be repeated, repeat the baseline OS sequence.
NOTE: A period of 2-3 min before repeating the acquisition is required to allow the physiology to return to baseline. Previous data have shown that physiology does not return to baseline after 1 min41. - If the image quality of the OS baseline sequence is adequate, repeat the OS continuous acquisition and performance of the breathing maneuvers.
- If the breathing maneuvers need to be repeated, repeat the baseline OS sequence.
6. Image analysis
- Import the OS-CMR image data sets into a DICOM viewer with image contouring capabilities, best with functionality to automatically analyze oxygenation-sensitive signal intensity changes.
- Markers and their measurement
- Acquire a baseline image during a short, baseline breath-hold acquisition before hyperventilation (rest). Compare the first image of the breath-hold (representing the end of the "stress" stimulus) to the baseline image.
NOTE: Hyperventilation is a vasoconstrictive stimulus that reduces myocardial oxygenation (Healthy: %ΔSI ≈−5% to −10%13). - Obtain many images (and cardiac cycles) during the breath-hold. Use the first image of the breath-hold as the baseline and compare all following images to this image.
NOTE: Breath-hold is a vasodilating stimulus that increases myocardial oxygenation (%ΔSI ≈ +5%-15%12,13,14,16). - Myocardial contours
For manual analysis: cardiac phase selection- As the breath-hold can contain greater than 400 images, analyze only a single phase of each cardiac cycle. As a result, focus the analysis on the end-systolic images of each cardiac cycle.
- Identify the end-systolic images of each cardiac cycle.
- Draw the epicardial and endocardial contours around the myocardium.
- Window the image to look for artifacts, which will appear as either dark (susceptibility) or bright areas due to poor gating in the myocardium.
NOTE: Avoid including pixels with partial volume effects from the left and right ventricular blood pools. Most contouring errors occur from the endocardial contour, including pixels with partial volume effects and resultant artificially elevated signal intensity from the left ventricular blood pool. To avoid this, draw the endocardial contour one full pixel inside the myocardium. Similarly, ensure that the epicardial contour is one full pixel inside the myocardium to avoid partial volume effects from the right ventricular blood pool, epicardial fat, or air-lung interface. - Copy and paste the endocardial and epicardial contours from the first end-systolic image of the cardiac cycle to the end-systolic image of the next cardiac cycle. Adjust the contours as needed.
For automated analysis:
NOTE: With automated contouring capabilities, if desired, all phases of the cardiac cycle can be contoured and analyzed. - Check all images to ensure accurate contouring.
NOTE: Some commercially available automated contouring capabilities have been trained on data sets that were contoured for volumetric analysis. These contours are prone to partial volume effects as they are meant to border the blood pool and myocardium. OS-CMR contours must be fully inside of the myocardium.
- Acquire a baseline image during a short, baseline breath-hold acquisition before hyperventilation (rest). Compare the first image of the breath-hold (representing the end of the "stress" stimulus) to the baseline image.
7. Segmentation for regional analysis
- To obtain regional information, identify the anteroseptal and inferoseptal insertion of the right ventricle to divide the myocardium into American Heart Association (AHA) segmentation42.
8. Calculating B-MORE
- Express B-MORE as a percent change in signal intensity from baseline to vasodilation (see equation 1):
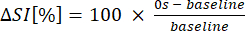 (1)
(1) - Calculate the global B-MORE as the global mean myocardial signal intensity of the end-systolic images at 30 s compared to 0 s of the breath-hold8 (see equation 2):
 (2)
(2)
Access restricted. Please log in or start a trial to view this content.
Results
Interpreting B-MORE
In previously published studies utilizing OS-CMR with vasoactive breathing maneuvers, the global or regional B-MORE was calculated by comparing the first end-systolic image of the breath-hold to the end-systolic image closest to 15 s, 30 s, 45 s, etc. of the breath-hold. The end-systolic phase of the cardiac cycle was chosen for several reasons. The end-systolic image is the most consistent phase identified among and between readers: it contains the greatest number of pixels in ...
Access restricted. Please log in or start a trial to view this content.
Discussion
x`The addition of an OS-CMR acquisition with standardized, vasoactive breathing maneuvers to an already established research or clinical MRI protocol adds little time to the overall scan. With this short addition, information about underlying macro- and microvascular function can be obtained (Figure 2). An important consequence of endothelial dysfunction is the inability of the vasculature to respond to physiologic stimuli, as initially demonstrated through abnormal flow-mediated relaxation ...
Access restricted. Please log in or start a trial to view this content.
Disclosures
MGF is listed as a holder of United States Patent No. 14/419,877: Inducing and measuring myocardial oxygenation changes as a marker for heart disease; United States Patent No. 15/483,712: Measuring oxygenation changes in tissue as a marker for vascular function; United States Patent No 10,653,394: Measuring oxygenation changes in tissue as a marker for vascular function - continuation; and Canadian Patent CA2020/051776: Method and apparatus for determining biomarkers of vascular function utilizing bold CMR images. EH is listed as a holder of International Patent CA2020/051776: Method and apparatus for determining biomarkers of vascular function utilizing bold CMR images.
Acknowledgements
This paper and methodology review was made possible by the entire team of the Courtois CMR Research Group at the McGill University Health Centre. Special thanks to our MRI technologists Maggie Leo and Sylvie Gelineau for the scanning of our participants and feedback on this manuscript.
Access restricted. Please log in or start a trial to view this content.
Materials
| Name | Company | Catalog Number | Comments |
| balanced SSFP MRI sequence | Any | To modify to create the OS-CMR sequence | |
| DICOM/ Imaging Viewer | Any | Best if the viewer has the ability for quantitative measurements (i.e., Area19 prototype software) | |
| Magnetic Resonance Imaging scanner | Any | 3 Tesla or 1.5 Tesla | |
| Metronome | Any | Set to 30 breaths per minute. To use if manually communicating breathing maneuver instructions to participants. | |
| Speaker system | Any | To communicate breathing maneuver instrucitons to participants through | |
| Stopwatch | Any | To use if manually communicating breathing maneuver instructions to participants |
References
- Ogawa, S., Lee, T. M., Kay, A. R., Tank, D. W. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proceedings of the National Academy of Sciences of the United States of America. 87 (24), 9868-9872 (1990).
- Friedrich, M. G., Karamitsos, T. D. Oxygenation-sensitive cardiovascular magnetic resonance. Journal of Cardiovascular Magnetic Resonance. 15, 43(2013).
- Guensch, D. P., et al. The blood oxygen level dependent (BOLD) effect of in-vitro myoglobin and hemoglobin. Scientific Reports. 11 (1), 11464(2021).
- Guensch, D. P., et al. Breathing manoeuvre-dependent changes in myocardial oxygenation in healthy humans. European Heart Journal - Cardiovascular Imaging. 15 (4), 409-414 (2014).
- Fischer, K., Guensch, D. P., Shie, N., Lebel, J., Friedrich, M. G. Breathing maneuvers as a vasoactive stimulus for detecting inducible myocardial ischemia - An experimental cardiovascular magnetic resonance study. PloS One. 11 (10), 0164524(2016).
- Friedrich, M. G. Tracking myocardial oxygenation over a breath hold with blood oxygen level−dependent MRI: A radically different approach to study ischemia. Radiology. 294 (3), 546-547 (2020).
- Teixeira, T., Nadeshalingam, G., Fischer, K., Marcotte, F., Friedrich, M. G. Breathing maneuvers as a coronary vasodilator for myocardial perfusion imaging. Journal of Magnetic Resonance Imaging. 44 (4), 947-955 (2016).
- Fischer, K., Guensch, D. P., Friedrich, M. G. Response of myocardial oxygenation to breathing manoeuvres and adenosine infusion. European Heart Journal Cardiovascular Imaging. 16 (4), 395-401 (2015).
- Ong, P., Athanasiadis, A., Sechtem, U. Intracoronary acetylcholine provocation testing for assessment of coronary vasomotor disorders. Journal of Visualized Experiments. (114), e54295(2016).
- Voigtländer, T., et al. The adverse events and hemodynamic effects of adenosine-based cardiac MRI. Korean Journal of Radiology. 12 (4), 424-430 (2011).
- Tsang, K. H., Chan, W. S. W., Shiu, C. K., Chan, M. K. The safety and tolerability of adenosine as a pharmacological stressor in stress perfusion cardiac magnetic resonance imaging in the Chinese population. Hong Kong Medical Journal. 21 (6), 524-527 (2015).
- Roubille, F., Fischer, K., Guensch, D. P., Tardif, J. -C., Friedrich, M. G. Impact of hyperventilation and apnea on myocardial oxygenation in patients with obstructive sleep apnea - An oxygenation-sensitive CMR study. Journal of Cardiology. 69 (2), 489-494 (2017).
- Fischer, K., et al. Feasibility of cardiovascular magnetic resonance to detect oxygenation deficits in patients with multi-vessel coronary artery disease triggered by breathing maneuvers. Journal of Cardiovascular Magnetic Resonance. 20 (1), 31(2018).
- Iannino, N., et al. Myocardial vascular function assessed by dynamic oxygenation-sensitive cardiac magnetic resonance imaging long-term following cardiac transplantation. Transplantation. 105 (6), 1347-1355 (2021).
- Elharram, M., et al. Regional heterogeneity in the coronary vascular response in women with chest pain and nonobstructive coronary artery disease. Circulation. 143 (7), 764-766 (2021).
- Fischer, K., et al. Insights into myocardial oxygenation and cardiovascular magnetic resonance tissue biomarkers in heart failure with preserved ejection fraction. Circulation: Heart Failure. 15 (4), 008903(2022).
- Li, D., Dhawale, P., Rubin, P. J., Haacke, E. M., Gropler, R. J. Myocardial signal response to dipyridamole and dobutamine: demonstration of the BOLD effect using a double-echo gradient-echo sequence. Magnetic Resonance in Medicine. 36 (1), 16-20 (1996).
- Arnold, J. R., et al. Myocardial oxygenation in coronary artery disease: insights from blood oxygen level-dependent magnetic resonance imaging at 3 tesla. Journal of the American College of Cardiology. 59 (22), 1954-1964 (2012).
- Karamitsos, T. D., et al. Relationship between regional myocardial oxygenation and perfusion in patients with coronary artery disease: Insights from cardiovascular magnetic resonance and positron emission tomography. Circulation: Cardiovascular Imaging. 3 (1), 32-40 (2010).
- Friedrich, M. G., Niendorf, T., Schulz-Menger, J., Gross, C. M., Dietz, R. Blood oxygen level-dependent magnetic resonance imaging in patients with stress-induced angina. Circulation. 108 (18), 2219-2223 (2003).
- Cai, H., Harrison, D. G. Endothelial dysfunction in cardiovascular diseases: The role of oxidant stress. Circulation Research. 87 (10), 840-844 (2000).
- Kothawade, K., Bairey Merz, C. N. Microvascular coronary dysfunction in women: Pathophysiology, diagnosis, and management. Current Problems in Cardiology. 36 (8), 291-318 (2011).
- Gimbrone, M. A., García-Cardeña, G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circulation Research. 118 (4), 620-636 (2016).
- Vancheri, F., Longo, G., Vancheri, S., Henein, M. Coronary microvascular dysfunction. Journal of Clinical Medicine. 9 (9), 2880(2020).
- Camici, P. G., Crea, F. Coronary microvascular dysfunction. The New England Journal of Medicine. 356 (8), 830-840 (2007).
- Ford, T. J., et al. Assessment of vascular dysfunction in patients without obstructive coronary artery disease: Why, how, and when. JACC: Cardiovascular Interventions. 13 (16), 1847-1864 (2020).
- Taqueti, V. R., Di Carli, M. F. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. Journal of the American College of Cardiology. 72 (21), 2625-2641 (2018).
- Budhiraja, R., Parthasarathy, S., Quan, S. F. Endothelial dysfunction in obstructive sleep apnea. Journal of Clinical Sleep Medicine. 3 (4), 409-415 (2007).
- Sena, C. M., Pereira, A. M., Seiça, R. Endothelial dysfunction - A major mediator of diabetic vascular disease. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1832 (12), 2216-2231 (2013).
- Vanhoutte, P. M., Shimokawa, H., Feletou, M., Tang, E. H. C. Endothelial dysfunction and vascular disease - A 30th anniversary update. Acta Physiologica. 219 (1), 22-96 (2017).
- Juni, R. P., Duckers, H. J., Vanhoutte, P. M., Virmani, R., Moens, A. L. Oxidative stress and pathological changes after coronary artery interventions. Journal of the American College of Cardiology. 61 (14), 1471-1481 (2013).
- Simsek, E. C., et al. Endothelial dysfunction in patients with myocardial ischemia or infarction and nonobstructive coronary arteries. Journal of Clinical Ultrasound. 49 (4), 334-340 (2021).
- Stillman, A. E., et al. Imaging the myocardial ischemic cascade. The International Journal of Cardiovascular Imaging. 34 (8), 1249-1263 (2018).
- Fischer, D., et al. Endothelial dysfunction in patients with chronic heart failure is independently associated with increased incidence of hospitalization, cardiac transplantation, or death. European Heart Journal. 26 (1), 65-69 (2005).
- Hurst, T., Olson, T. H., Olson, L. E., Appleton, C. P. Cardiac syndrome X and endothelial dysfunction: New concepts in prognosis and treatment. The American Journal of Medicine. 119 (7), 560-566 (2006).
- Bauer, W. R., et al. Theory of the BOLD effect in the capillary region: An analytical approach for the determination of T*2 in the capillary network of myocardium. Magnetic Resonance in Medicine. 41 (1), 51-62 (1999).
- Manka, R., et al. BOLD cardiovascular magnetic resonance at 3.0 tesla in myocardial ischemia. Journal of Cardiovascular Magnetic Resonance. 12 (1), 54(2010).
- Dharmakumar, R., Qi, X., Hong, J., Wright, G. A. Detecting microcirculatory changes in blood oxygen state with steady-state free precession imaging. Magnetic Resonance in Medicine. 55 (6), 1372-1380 (2006).
- Kramer, C. M., et al. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. Journal of Cardiovascular Magnetic Resonance. 22 (1), 17(2020).
- Expert Panel on MR Safety et al. ACR guidance document on MR safe practices: 2013. Journal of Magnetic Resonance Imaging: JMRI. 37 (3), 501-530 (2013).
- Macey, P. M., Kumar, R., Ogren, J. A., Woo, M. A., Harper, R. M. Global brain blood-oxygen level responses to autonomic challenges in obstructive sleep apnea. PLoS One. 9 (8), 105261(2014).
- Cerqueira, M. D., et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. Circulation. 105 (4), 539-542 (2002).
- Hayoz, D., et al. Flow-mediated arterial dilation is abnormal in congestive heart failure. Circulation. 87 (6), 92-96 (1993).
- Hillier, E., Friedrich, M. G. The potential of oxygenation-sensitive CMR in heart failure. Current Heart Failure Reports. 18 (5), 304-314 (2021).
- Hawkins, S. M., et al. Hyperventilation-induced heart rate response as a potential marker for cardiovascular disease. Scientific Reports. 9 (1), 17887(2019).
- Dass, S., et al. No evidence of myocardial oxygen deprivation in nonischemic heart failure. Circulation: Heart Failure. 8 (6), 1088-1093 (2015).
- Endemann, D. H., Schiffrin, E. L. Endothelial dysfunction. Journal of the American Society of Nephrology. 15 (8), 1983-1992 (2004).
- Costanzo, M. R., et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. The Journal of Heart and Lung Transplantation. 29 (8), 914-956 (2010).
- Lanza, G. A. Cardiac syndrome X: A critical overview and future perspectives. Heart. 93 (2), 159-166 (2007).
- Gould, K. L., Johnson, N. P. Coronary physiology beyond coronary flow reserve in microvascular angina: JACC state-of-the-art review. Journal of the American College of Cardiology. 72 (21), 2642-2662 (2018).
- Guensch, D. P., Nadeshalingam, G., Fischer, K., Stalder, A. F., Friedrich, M. G. The impact of hematocrit on oxygenation-sensitive cardiovascular magnetic resonance. Journal of Cardiovascular Magnetic Resonance. 18 (1), 42(2016).
- Dharmakumar, R., et al. Assessment of regional myocardial oxygenation changes in the presence of coronary artery stenosis with balanced SSFP imaging at 3.0T: Theory and experimental evaluation in canines. Journal of Magnetic Resonance Imaging. 27 (5), 1037-1045 (2008).
- Hillier, E., Benovoy, M., Friedrich, M. A fully automated post-processing tool identifies a reduced global myocardial oxygenation reserve in patients with ischemia and no obstructive coronary artery stenosis when compared to patients with significant CAD. SCMR 25th Annual Scientific Sessions. , (2022).
Access restricted. Please log in or start a trial to view this content.
Erratum
Formal Correction: Erratum: Oxygenation-sensitive Cardiac MRI with Vasoactive Breathing Maneuvers for the Non-invasive Assessment of Coronary Microvascular Dysfunction
Posted by JoVE Editors on 1/01/1970. Citeable Link.
This corrects the article 10.3791/64149
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved