Zum Anzeigen dieser Inhalte ist ein JoVE-Abonnement erforderlich. Melden Sie sich an oder starten Sie Ihre kostenlose Testversion.
Method Article
Nasolacrimal Lavage as a Treatment for Ocular Surface Toxic Soup Syndrome
In diesem Artikel
Zusammenfassung
OSTSS leads to pooled inflammatory mediators in the tear film, causing symptoms like epiphora and discomfort. Here, we present a case where therapeutic nasolacrimal lavage every 2 months resolved epiphora and itchiness, suggesting its efficacy as a therapeutic intervention for OSTSS. Additionally, we report subjective improvements in symptoms in 3 additional patients.
Zusammenfassung
Ocular surface toxic soup syndrome (OSTSS) is characterized by inadequate tear drainage through the nasolacrimal duct system, leading to the accumulation of inflammatory mediators in the tear film. This condition can result in toxic keratoconjunctivitis, with symptoms such as conjunctival hyperemia, itchiness, discomfort, and epiphora. Dilation and irrigation are common diagnostic procedures in both optometry and ophthalmology, used to assess nasolacrimal duct obstruction in cases of epiphora. This technique involves the injection of saline into the nasolacrimal duct system through the puncta, followed by the evaluation of reflux, which indicates obstruction. Although intended to be diagnostic, many patients report significant improvements in epiphora and ocular comfort after the procedure. In this paper, we present a case study in which a patient achieved complete resolution of epiphora and itchiness following therapeutic nasolacrimal lavage performed every 2 months. Subjective improvements in symptoms in 3 additional patients are also reported. We propose nasolacrimal lavage not only as a diagnostic tool but also as an effective therapeutic intervention for managing OSTSS.
Einleitung
Tear flow is essential for ocular surface homeostasis, maintained through interactions among the secretory and neurovascular systems, with the meibomian glands, lacrimal gland, goblet cells, conjunctiva, and their vascular and neural networks working together to sustain a stable tear film1,2. This balance relies on the dynamic interplay between tear production and drainage, which directly affects the overall tear turnover rate (TTR)3. A reduced TTR can exacerbate dry eye symptoms by leading to the accumulation of inflammatory mediators on the ocular surface, resulting in what we term Ocular Surface Toxic Soup Syndrome (OSTSS). Reduced TTR is suspected to contribute to dry eye, as symptomatic patients typically have lower tear turnover rates compared to asymptomatic controls4. Tear production and turnover rates likely influence the cytokine environment of the ocular surface, both by delivering cytokines through the tear fluid and by removing those accumulated on the ocular surface5. The dysfunction of the nasolacrimal system, which impairs tear drainage and absorption of tear fluid components, may contribute to the development of OSTSS by allowing inflammatory mediators to accumulate on the ocular surface, potentially triggering abnormal immune responses and exacerbating dry eye pathology6,7.
Punctal plugs have long been a cornerstone in managing dry eye disease associated with aqueous tear deficiency by blocking tear drainage to enhance tear retention on the ocular surface8,9. However, the effectiveness of punctal occlusion has been questioned recently10. Lacrimal irrigation, or nasolacrimal lavage, on the other hand, offers a potential alternative treatment to alleviate dry eye symptoms in cases of suspected OSTSS. In this report, we present a case in which nasolacrimal lavage provided significant relief for a patient with mixed etiologies, demonstrating its versatility as a treatment option.
Consent for nasolacrimal lavage is similar to consent for probe and irrigation, with the primary difference being that nasolacrimal lavage is an off-label, therapeutic treatment for keratoconjunctivitis sicca and allergic conjunctivitis, whereas probe and irrigation is considered a diagnostic procedure to determine the cause of epiphora. Patients must be informed of the off-label nature of this treatment.
The goal of nasolacrimal lavage is to improve tear drainage through the nasolacrimal system to promote tear turnover and clear the lacrimal sac. There are no direct alternatives that accomplish the same goal.
Nasolacrimal lavage carries minimal risk. When performed correctly, and in the absence of nasolacrimal duct obstruction, patients will experience saline drainage either into the back of the throat (with the head tilted back) or into the nose (with the head tilted forward). Mild irritation may occur around the puncta or at the punctal opening. Additionally, there is a slight risk of unintentional contact with the eyelid or globe from the blunt cannula.
When in the setting of epiphora and clinically appropriate, nasolacrimal lavage is a procedure generally covered by insurance under the description of probe and irrigation.
A 73-year-old Black woman presented with complaints of intermittent, yet severe, itchiness medially and mild grittiness in both eyes. The patient's ocular medications included cyclosporine 0.05%, twice daily in both eyes; preservative-free artificial tears as needed in both eyes; alcaftadine 0.25%, once daily in both eyes; and eyelid wipes once daily. She had previously used tobramycin 0.3% and dexamethasone 0.1% four times daily for 10 days, which provided effective symptom relief, but her symptoms recurred upon discontinuation. Her medical history was notable for bilateral keratoconjunctivitis, bilateral meibomian gland dysfunction, and squamous blepharitis of the upper and lower eyelids in both eyes. Ocular surgical history included barrier laser retinopexy in the right eye for a retinal tear, performed 7 months prior. Systemic medications included atorvastatin for hyperlipidemia and a daily inhalation of fluticasone furoate 200 µg/umeclidinium 62.5 µg/vilanterol 25 µg for chronic obstructive pulmonary disease (COPD).
On ocular surface examination, there was trace inferior corneal staining in both eyes, 1+ bulbar conjunctival injection in both eyes, 1+ papillary reaction of the palpebral conjunctiva in both lower eyelids, mild conjunctivochalasis, 1+ blepharitis of both upper eyelids, and 3+ meibomian gland dysfunction with thickened secretions. Mild lower eyelid laxity was also noted in both eyes. Schimer's I score was 17 mm in the right eye and 14 mm in the left eye.
The patient reported pruritus in the inner canthus of both eyes, where tears drain from the ocular surface into the nasolacrimal duct system through the puncta. Additionally, there was conjunctival injection at the nasal aspect of the bulbar conjunctiva, where tears accumulate before draining from the ocular surface. These findings are consistent with ocular surface tear dysfunction syndrome (OSTSS), which is associated with the accumulation of allergen particulates and inflammatory mediators. Given this, nasolacrimal lavage was performed at the lower puncta of both eyes as an off-label therapeutic intervention to facilitate proper tear drainage and reduce the buildup of allergens and inflammatory mediators in the inner canthus.
Protokoll
The study received approval from the Colorado Multiple Institutional Review Board, and all research conformed to the tenets of the Declaration of Helsinki.
1. Preparation of the sterile field
- Gather the necessary instruments and materials: Topical anesthetic (e.g., proparacaine), punctal dilator, lacrimal cannula (25 G x 1/2 inch), and a 3 mL syringe filled with saline.
- Prepare a sterile field to ensure a clean procedure environment.
- Thoroughly review and have the patient sign the consent form prior to the procedure. Explain to the patient that nasolacrimal lavage is an off-label therapeutic procedure unless they qualify for an on-label probe and irrigation procedure.
2. Patient instructions
- Procedure overview
- Explain that the bilateral nasolacrimal lavage procedure typically lasts about 5 min.
- Inform the patient that they may experience mild discomfort, irritation, stinging, or watering during the procedure. There may be some pressure, but there should be no overt pain.
- Positioning
- Have the patient sit back and relax. Ensure the back of their head is supported by the headrest.
- Instruct the patient to look up, which helps direct the saline toward the throat if the duct is patent.
- During the procedure
- Instruct the patient to stay as still and calm as possible. Limit talking, except for expressing discomfort. This minimizes distractions and ensures a smooth procedure.
- Advise the patient to breathe normally and avoid holding their breath. This reduces tension and helps the patient stay relaxed.
- Tell the patient to minimize blinking. If they cannot keep their eyes open, gently evert the lower eyelid to expose the lower punctum.
- Ensure the patient's head is positioned correctly with the eyes looking up and out towards the ceiling while the lower punctum is probed.
- After the procedure
- Patients may experience mild discomfort, stinging, or watering around the inner corner of the eye. These sensations are normal and should subside shortly.
- Some mucus or discharge from the eye is expected after the procedure. Advise the patient to gently wipe away any discharge with a clean tissue.
- Advise patients not to rub their eyes, as this may cause irritation or injury.
- If the patient experiences discomfort or mild swelling, recommend using a cold compress for 10-15 min. Suggest preservative-free artificial tears to relieve irritation.
- Instruct the patient to return to the clinic or contact the performing optometrist or ophthalmologist if they experience persistent discharge, increased redness, swelling, pain, or changes in vision.
3. Procedure
- Hand hygiene and equipment check
- Wash hands thoroughly and don clean gloves.
- Verify that all required instruments are available in the sterile field (as listed in Section 1.1).
- Attach the 3 mL syringe filled with saline to the lacrimal cannula.
- Anesthesia
- Instill one drop of topical anesthetic (e.g., proparacaine) into the intended eye(s).
- Wait 30-60 s to allow the anesthetic to take effect. Monitor for patient comfort.
- Punctal dilation (if necessary)
- If the punctum is too small to proceed with cannulation, select the smallest punctal dilator and gently insert it vertically 1-2 mm into the lower punctum.
- Rotate the dilator 90° so that the tip points toward the nose.
- Gradually increase the size of the dilator until it comfortably accommodates the lacrimal cannula. Ensure that the punctum is dilated without causing trauma.
- Cannulation
- Gently insert the lacrimal cannula into the lower punctum and advance it into the vertical canaliculus.
- Rotate the cannula horizontally with the blunt tip facing toward the nose.
- Gently advance the cannula 3-6 mm into the canaliculus. Ensure the cannula moves smoothly without resistance.
- Irrigation
- Slowly inject 2-3 mL of saline solution through the cannula into the lacrimal duct system. Apply gentle pressure to avoid discomfort or trauma.
- Observe for resistance or reflux during irrigation. Check for resistance, which may indicate a duct obstruction. Reflux may suggest improper cannula placement or obstruction.
- Remove the cannula from the punctum.
- Assessment and repetition.
- After irrigation, observe for displaced mucus or signs of improvement in ocular discomfort symptoms.
- Use a slit lamp to assess tear flow by observing small particles moving toward the punctum along the lower tear meniscus.
- If the patient detects irrigated fluid in the back of the throat (head tilted back) or nose (head tilted forward), confirm that the lacrimal system is patent.
- If the patient experiences pain during irrigation, suspect distal obstruction at the nasolacrimal duct. Replace the saline with a topical anesthetic to numb the lacrimal sac. Continue irrigation to attempt to clear the obstruction.
- Repeat procedure on contralateral side (if applicable)
- If treatment is required on the other eye, repeat the procedure following the same steps for the contralateral lower punctum.
- Post-procedure care
- Remove excess discharge or mucus from the eye using a clean tissue.
- Monitor the patient for signs of discomfort, redness, or significant discharge.
- Provide post-procedure instructions, including the use of cold compresses and preservative-free artificial tears if needed.
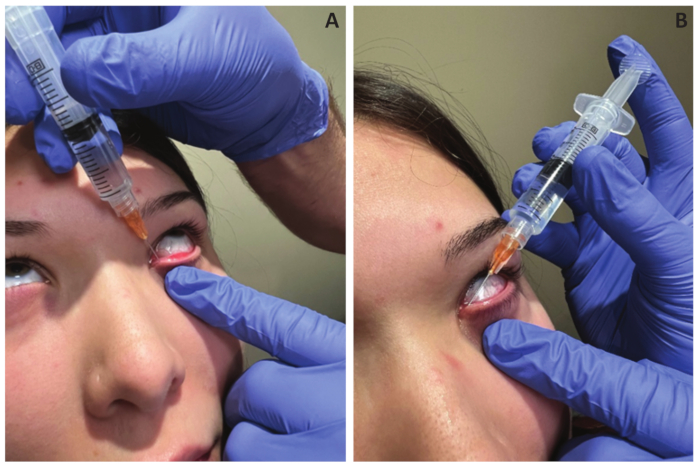
Figure 1: Cannula positioning. (A,B) Inserting the cannula into the vertical canaliculus of the lower punctum, then rotating the cannula into the horizontal canaliculus. Please click here to view a larger version of this figure.
4. Post-procedure examination
- After the procedure, examine the anterior segment of the treated eye(s) to ensure no trauma has occurred to the cornea, bulbar conjunctiva, palpebral conjunctiva, punctum, or eyelids.
- Remove any excess discharge or mucus from the eye with a clean tissue or sterile cotton swab.
- Monitor the patient for any signs of discomfort or complications (e.g., swelling, redness, or significant discharge).
- Provide the patient with post-procedure instructions, including the use of cold compresses and preservative-free artificial tears for comfort, if needed.
Ergebnisse
The patient (Patient 1) initially reported 100% improvement in nasal itchiness immediately following the procedure. At her 3-month follow-up, she reported remaining free of pruritus since the previous visit. Upon examination, bilateral inferior corneal staining, bulbar injection, and papilla had resolved. Four months later, the patient returned to the clinic with a recurrence of medial itchiness in both eyes. Her bilateral inferior corneal staining, bulbar injection, and papilla had reapp...
Diskussion
Nasolacrimal lavage is a procedure designed to irrigate the nasolacrimal duct system, analogous to the use of a sinus rinse for the nasal passages. We hypothesize that it may remove allergens and inflammatory biomarkers from the tear drainage system, which could otherwise backflow onto the ocular surface. Additionally, nasolacrimal lavage aims to enhance tear turnover by clearing mucus or dacryoliths that may obstruct tear drainage. In essence, nasolacrimal lavage serves as an inverse to the commonly performed procedure ...
Offenlegungen
The authors have nothing to disclose.
Danksagungen
We would like to express their sincere gratitude to the patient discussed in this case, who has since passed away. Her passing is deeply felt by both her family and the clinic staff. Throughout her treatment, her sincere appreciation during each nasolacrimal lavage not only inspired us to continue this procedure with other patients but also encouraged the writing of this manuscript. We hope that this manuscript serves as a small tribute to her memory.
Materialien
| Name | Company | Catalog Number | Comments |
| Blunt Fill Needle | BD | 305180 | 18 G |
| Lacrimal cannula | BVI VisiTec | 585068 | 25 G x 1/2 inch |
| Luer Lock Disposable Syringe | Medline | SYR105010 | 5 mL |
| Nitrile Gloves (SensiCare Ice) | Medline | MD26803 | Nitrile Gloves |
| Polylined Sterile Field | Busse | 697 | 18' x 26", fenestrated |
| Saline bullets | Hudson RCI | 200-59 | 5 mL sterile |
Referenzen
- Dartt, D. A. Neural regulation of lacrimal gland secretory processes: relevance in dry eye diseases. Prog Retin Eye Res. 28 (3), 155-177 (2009).
- Pflugfelder, S. C., Stern, M. E. Biological functions of tear film. Exp Eye Res. 197, 108115 (2020).
- Garaszczuk, I. K., Montes Mico, R., Iskander, D. R., Expósito, A. C. The tear turnover and tear clearance tests-a review. Expert Rev Med Devices. 15 (3), 219-229 (2018).
- Sorbara, L., Simpson, T., Vaccari, S., Jones, L., Fonn, D. Tear turnover rate is reduced in patients with symptomatic dry eye. Cont Lens Anterior Eye. 27 (1), 15-20 (2004).
- Barton, K., Nava, A., Monroy, D. C., Pflugfelder, S.C. Cytokines and Tear Function in Ocular Surface Disease. In Lacrimal Gland, Tear Film, and Dry Eye Syndromes 2: Basic Science and Clinical Relevance. Springer, Boston, MA (1998).
- Paulsen, F., Schaudig, U., Thale, A. B. Drainage of tears: impact on the ocular surface and lacrimal system. Ocul Surf. 1 (4), 180-191 (2003).
- Wang, D. et al. Detection & analysis of inflammatory cytokines in tears of patients with lacrimal duct obstruction. Indian J Med Res. 154 (6), 888-894 (2021).
- Willis, R. M., Folberg, R., Krachmer, J. H., Holland, E. J. The treatment of aqueousdeficient dry eye with removable punctal plugs: a clinical anti impressioncytologic study. Ophthalmology. 94 (5), 514-518 (1987).
- Jehangir, N., Bever, G., Mahmood, S. J., Moshirfar, M. Comprehensive review of the literature on existing punctal plugs for the management of dry eye disease. J Ophthalmol. 2016 (1), 9312340 (2016).
- Ervin, A. -M., Law, A., Pucker, A. D. Punctal occlusion for dry eye syndrome: summary of a Cochrane systematic review. Br J Ophthalmol. 103 (3), 301-306 (2019).
- Tsubota, K. Tear dynamics and dry eye. Prog Retin Eye Res. 17 (4), 565-596 (1998).
- Tawfik, H. A., Abdulhafez, M. H., Fouad, Y. A. Congenital upper eyelid coloboma: embryologic, nomenclatorial, nosologic, etiologic, pathogenetic, epidemiologic, clinical, and management perspectives. Ophthalm Plast Reconstr Surg. 31 (1), 1-12 (2015).
- Dua, H. S., Ting, D. S. J., Al Saadi, A., Said, D. G. Chemical eye injury: pathophysiology, assessment and management. Eye. 34 (11), 2001-2019 (2020).
- Kuo, M. T. et al. Tear proteomics approach to monitoring Sjögren syndrome or dry eye disease. Int J Mol Sci. 20 (8), 1932 (2019).
- HorwathWinter, J., Thaci, A., Gruber, A., Boldin, I. Longterm retention rates and complications of silicone punctal plugs in dry eye. Am J Ophthalmol. 144 (3), 441-444.e441 (2007).
- Tai, M. -C., Cosar, C. B., Cohen, E. J., Rapuano, C. J., Laibson, P. R. The clinical efficacy of silicone punctal plug therapy. Cornea. 21 (2), 135-139 (2002).
- Bourkiza, R., Lee, V. A review of the complications of lacrimal occlusion with punctal and canalicular plugs. Orbit. 31 (2), 86-93 (2012).
- Chen, F. et al. Tear meniscus volume in dry eye after punctal occlusion. Invest Ophthalmol Vis Sci. 51 (4), 1965-1969 (2010).
- Hartikainen, J., Lehtonen, O. -P., Saari, K.M. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol. 81 (1), 37-40 (1997).
- Kelly, D. J., Hughes, N. J., Poole, R.K. Microaerobic Physiology: Aerobic Respiration, Anaerobic Respiration, and Carbon Dioxide Metabolism. In Helicobacter pylori: Physiology and Genetics. ASM Press, Washington, DC (2001).
- McGinnigle, S., Naroo, S. A., Eperjesi, F. Evaluation of dry eye. Surv Ophthalmol. 57 (4), 293-316 (2012).
- Dursun, D. et al. A mouse model of keratoconjunctivitis sicca. Invest Ophthalmol Vis Sci. 43 (3), 632-638 (2002).
- Pflugfelder, S. C. et al. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tearfilm disorders known to cause ocular irritation. Cornea. 17 (1), 38 (1998).
- Afonso, A.A. et al. Correlation of tear fluorescein clearance and Schirmer test scores with ocular irritation symptoms. Ophthalmology. 106 (4), 803-810 (1999).
Nachdrucke und Genehmigungen
Genehmigung beantragen, um den Text oder die Abbildungen dieses JoVE-Artikels zu verwenden
Genehmigung beantragenThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Alle Rechte vorbehalten