A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Quantification of Levator Ani Hiatus Enlargement by Magnetic Resonance Imaging in Males and Females with Pelvic Organ Prolapse
In This Article
Summary
Here we present a protocol to standardize the measurement of the levator ani hiatus size by magnetic resonance imaging. The purpose is to extract biomechanical inferences from image analysis by comparing resting and straining values in patients of both sexes with pelvic prolapse, using consistent anatomical bony landmarks.
Abstract
Here we present a protocol to examine the levator ani hiatus in males and females with pelvic organ prolapse, during the Valsalva maneuver and while evacuating acoustic gel, using a horizontally oriented 1.5 T magnetic resonance (MR) scanner. On midsagittal images, the vertical distance of pelvic organs is measured in millimeters relative to the hymen plane (female) and to the lower border of the symphysis pubis (male), preceded by - (above) or + ( below) signs. On axial images, the levator ani area is calculated in square centimeters with a free-hand tracing method from three key images, passing through the midsymphysis (level I), tangential to the lower border of the symphysis (level II), and at the maximal anterior rectal wall bulging (level III). Areas at rest and strained are compared to find evidence of a percentage of increase. The purpose is to provide objective evidence of the maximal extent of pelvic organs descent and hiatus enlargement without the interference of foreign objects or the examiner's proximity, so as to overcome the limitations of pelvic examination and transperineal sonography (i.e., subjectivity and sex-related limitations [female only]).
Introduction
Pelvic organ prolapse (POP) develops when the forces acting inside the boundaries of levator ani hiatus are no longer counteracted by those outside, leading to abnormal enlargement and organ impingement. Several factors are responsible for the disease, including ligaments, fascia, or muscular tonic activity. Whatever the mechanism involved, the increased hiatus size has been credited with a reliable index to assess the inability to keep it closed. Usually, the status of pelvic support is determined in women during a pelvic examination1 by observing the location of the cervix, vaginal apex, and vaginal walls during the Valsalva maneuver. However, the inaccuracy of the method, combined with a failure to identify all involved sites2,3 and sex-related constrictions (female only), has led clinicians and researchers to seek alternative methods, namely diagnostic imaging.
Current methods for determining hiatus size include transperineal ultrasonography (TPUS)4,5 and, more recently, magnetic resonance imaging (MRI). Unfortunately, existing methods of performing the examination and measurement of individual parameters vary greatly among researchers6,7,8,9,10,11,12,13, making a comparison of study results difficult. Moreover, significant differences still exist in the definition and terminology of the most common pelvic descent processes, as well as in the classification and quantification of the adopted systems14,15.
This study highlights the advantages of MRI over other methods and describes the technical details and diagnostic criteria for the quantification of POP in patients of both sexes. In particular, the description focuses on the quantification of pelvic organs descent and levator ani hiatus enlargement when straining, with the patient supine, to demonstrate that the lack of a vertically oriented MR system16,17 (i.e., gravity will not adversely affect the detection of various changes associated with POP).
Protocol
Procedures involving human subjects have been performed according to the National Guidelines of the Italian Radiological Society
1. Patient preparation
- Help patients to fill in a form which provides information on their history, current symptoms, treatments (either medical or surgical), and prior medical records, if any.
- Obtain each patient's written consent before beginning the examination.
- Clearly explain in advance the characteristics and purpose of the procedure, including the performance of various maneuvers such as squeezing, straining, and rectal emptying.
- Give information on the duration (average time: 25 min) of the procedure and the need for the insertion of a small catheter into the anal canal for contrast administration (acoustic gel).
- Ask the patients to empty their bladder in the toilet just before starting the examination.
NOTE: On the basis of the patients' histories and presenting symptoms, tailor the procedure to each single case with regard to the amount of contrast administered and the number of scan planes and pulse sequences used.
2. Diagnostic room and facilities
- Keep a trolley inside the area of the diagnostic room, equipped with all necessary instruments and supplies, including gloves, syringes, a catheter, lubricant jelly, acoustic gel, etc. (see Table of Materials).
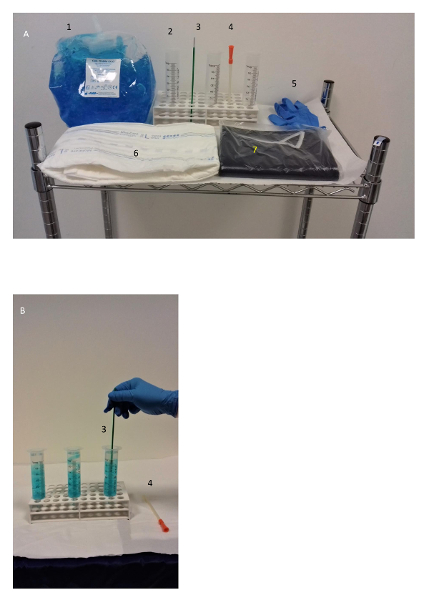
Figure 1: Supplies. This picture shows (A) a trolley with supplies for the MR examination and (B) the dilution of acoustic gel with water (50/30 mL per syringe) in the area adjacent to the diagnostic room before the administration. Please click here to view a larger version of this figure.
- Ask the patient to lay on the diagnostic table of the MR scanner in the left lateral position (Sims' position). Gently insert the catheter into the rectum and administer the contrast administration (acoustic coupling gel) until the patient experiences a characteristic desire to evacuate (the average amount is 250 mL). Turn the patient in the supine position afterward.
- Adjust the absorbent pad beneath the buttocks, and wrap around the patient's pelvis a surface phased-array coil for the image acquisition.
NOTE: In case of anticipated sensation, urgency, discomfort, or involuntary leakage, interrupt the injection and register the total volume injected before the leakage, as well as the volume leaked.
3. Technique and image acquisition
- Acquire a localizer scout scan in the coronal, axial, and sagittal planes (TFE T1 pulse sequence, TR of 8 ms, TE of 5 ms, flip angle (FA) of 25°, thickness of 15 mm, and the number of images: 5-11) to mark the boundaries of the region of interest (ROI).
- Then, obtain three subsequent dynamic series in the midsagittal plane (see Table 1, series 1: TR/TE of 2.7/1.3 ms; FA of 45°) centered over the anorectal junction, with the patient at rest, squeezing his/her anal sphincter, and straining (10 s each).
- Thereafter, instruct the patient to start - at will - the movement of rectal emptying, and notice when it starts (by acoustic device) to allow the simulatenous acquisition of images over an entire time cycle of 58 s (see Table 1, series 1: TR/TE of 2.7/1.3 ms; FA of 45°; thickness of 35 mm; acquisition time of 58 s).
NOTE: If necessary, repeat the series until obtaining an adequate stream of contrast. - Repeat the latter sequence in the coronal plane (see Table 1, series 2: TR/TE of 2.8/1.3 ms; FA of 45°; thickness of 35 mm; acquisition time of 58 s) while the patient is expelling the residual rectal contrast.
- Then, instruct the patient to perform a steady-state Valsalva maneuver without interruption for 9 s.
- Taking the sagittal images acquired during the rectal emptying as a reference, select three horizontal planes in the axial plane (see Figure 3) to image the levator hiatus as follows: the first at the midsymphysis (level I), the second tangent to the inferior border of the symphysis (level II), and the third at the point of the maximal bulging of the anterior rectal wall (level III).
NOTE: The reason for the above is to include most relevant anatomical areas inside and outside the hiatus boundaries of both sexes in the ROI: bladder base, urethra, vagina, cervix, perineal body, anorectal junction, endopelvic fascia, and fat recesses (female), or bladder base, retropubic space, prostate, seminal vesicles, Denonvilliers' fascia, anorectal junction, mesorectal fascia, and presacral space (male). - Acquire a horizontal 1 cm-thick section in the axial plane (see Table 1, series 3: TR/TE of 3/1.5 ms; FA of 45°; thickness of 10 mm; acquisition time of 9 s) from each level during the Valsalva maneuver, leaving the patient a 60 s interval between two subsequent maneuvers to relax.
- Finally, acquire static T2-weighted images when at rest in the axial, sagittal, and coronal planes (see Table 1, series 4, 5, and 6: TR/TE of 3649-4656/100; FA of 90°; thickness/gap of 4/0.4 mm; acquisition time of 3:00-3:44 min) to provide a complete evaluation of the pelvic anatomy.
NOTE: Refer to Table 1 for the technical settings.

Table 1: Technical settings for MR defecography, using a 1.5 T scanner and an external coil.
4. Image analysis and measurements
- To measure the position of the pelvic organs when at rest and while straining, from midsagittal dynamic MR images in the analysis software, go to the list of toolbar options positioned at the top of the screen and hover over Annotation Tools.
- Then, click on the arrow and select Ruler to obtain a linear measurement in millimeters of the vertical distance of the bladder neck, uterine cervix, prostate base, seminal vesicles, and rectal floor from two reference lines, as follows: express the distances by negative (proximal) or positive (distal) numbers relative to the hymen plane (female) or to a horizontal line drawn tangent to the inferior border of the symphysis pubis (male).
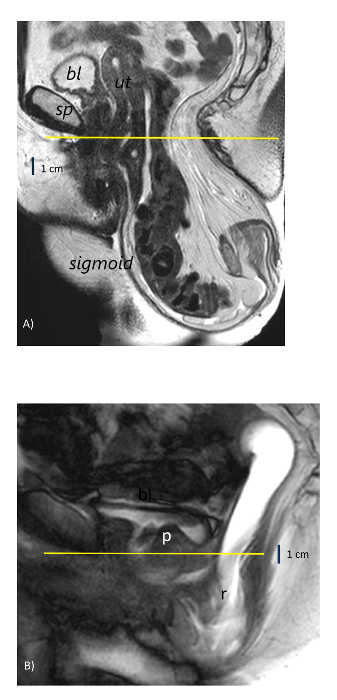
Figure 2: Reference lines for pelvic organ descent on midsagittal MR images. (A) A 61-year-old woman with a rectal descent of >10 cm below the hymen plane (yellow line) and sigmoidocele. (B) A 42-year-old man with rectal intussusception and a descent of >3 cm below the lower border of the symphysis pubis (yellow line). bl = bladder; sp = symphysis pubis; ut = uterus; r = rectum; p = prostate. Please click here to view a larger version of this figure.
- To measure the hiatal anterior/posterior and transverse diameter (in millimeters) from the axial static and dynamic images, repeat the same selection of linear measurements described in steps 4.1-4.2 and calculate the distance from the pubic symphysis to the anterior margin of the puborectalis sling and the distance between the medial borders of the levator ani muscle.
- To measure the hiatal area (in square centimeters) when at rest and during maximum strain, click again on Annotation Tools and choose Free-ROI to select a free-hand contour-tracing technique (see Figure 3).
- Depict the internal area of the levator ani muscle and express the differences between resting and straining measurements as absolute values and an increase in percentage from sections of the same level identified by the recognition of bony landmarks, namely the symphysis pubis and the ischial tuberosities (level 2).
NOTE: Register any impingement of the organs within the levator ani hiatus and refer, for organ prolapse definition and grading, to the standards recommended by the international committee on pelvic organ prolapse14,15 and to the traditional "HMO" MRI classification system of pelvic organ prolapse described by Comiter et al.9.
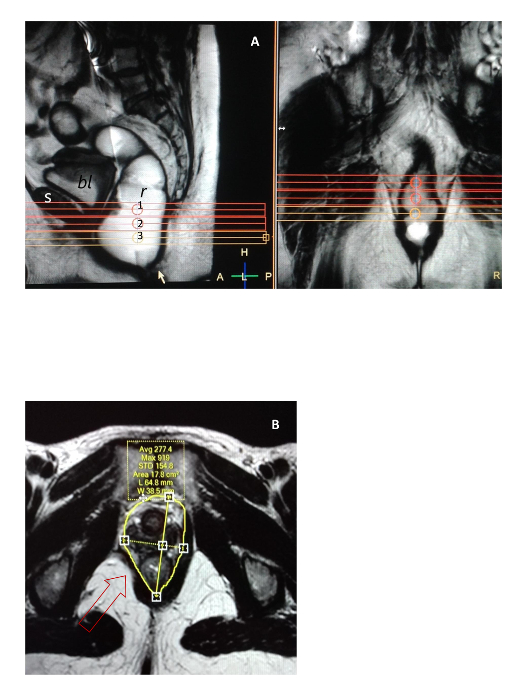
Figure 3: Method for levator ani hiatus imaging and area measurement. (A) A selection of three axial scan sections from a midsagittal image taken relative to the midsymphysis pubis (level 1), tangent to its lower border (level 2), and at the maximal bulging of the anterior rectal wall (level 3) during rectal emptying. (B) An example of an asymmetric area measured when at rest from level 2 with the free-hand contour-tracing method in a 52-year-old woman with a focal defect of the right pubococcygeus muscle (arrow). s = symphysis pubis; bl = bladder; r = rectum.The left panel = a sagittal view;the right panel = a coronal view.The area values are expressed in square centimeters.1 = first level; 2 = second level; 3 = third level. Please click here to view a larger version of this figure.
Results
Between 2012 and 2018, this protocol has been successfully adopted in three different diagnostic centers in Italy at an average cumulative rate of 30 ± 4 exams per month, using the same 1.5 T MR scanner model and technical settings (see Table 1 and Table of Materials). During this period, over 2,000 examinations have been performed in patients of both sexes for the following three main disease categories: pelvic organ prolapse and evacuation disturba...
Discussion
This method has an overt advantage over pelvic examinations that are limited to the assessment of the urogenital hiatus in only females. In contrast, the method presented here examines the entire levator ani hiatus in both sexes. Moreover, although easily examined by palpation by the gynecologist, the female hiatus can be calculated only approximately with a ruler, to produce the area of an oval1. Similarly, an advantage does exist over 2- and 3-D TPUS4,
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors are especially indebted to nurses Paola Garavello and Giulia Melara, for their valuable assistance during the examinations.
Materials
| Name | Company | Catalog Number | Comments |
| MR scanner | Philips Medical Systems, High Tech Campus 37, 5656 AE, Eindhoven, The Netherlands | Description: 1.5 T horizontally oriented, Multiva model, SENSE XL Torso coil Procedure: Position the patient in the left lateral decubitus on the diagnostic table with the coil warpped around the pelvis | |
| Catheter | Convatek ltd, First avenue Deeside, Flintshire CH5 2NU UK | Description: Sterile vaginal catheter, 16 ch,180 mm long, 3 mm wide Procedure: Gently insert the lubricated tip inside the anal canal for contrast administration with patients in the left side position | |
| Holder | Kartell Plastilab, Artiglas Srl, Via Carrara Padua, Italy | Description: Universal test-tube holder with multiple 13-mm holes Procedure: Put 3 empty syringes vertically inside the holes with the outlet cone down | |
| Syringe | Pikdare Srl, Via Saldarini Catelli 10 , 22070 Casnate con Bernate (Como) Italy | Description: Sterile, latex free,60 mL graduated transparent cylinder, catheter cone Procedure: Fill with contrast, adjust the plunger and connect to the catheter | |
| Contrast | Ceracarta SpA, Via Secondo Casadei 14 47122 Forlì Italy | Description: Eco supergel not irritant, water soluble, salt free Procedure: Dilute the content of each syringe adding 30 mL of tap water to 50 mL of acustic gel | |
| Mixer device | Kaltek Srl, Via del Progresso 2 Padua Italy | Description: Kito-Brush for endovaginal sampling Procedure: Rotate one full turn 10-20 times until obtaining an homogeneous gel | |
| Pad | Fater SpA, Via A. Volta 10, 65129 Pescara Italy | Description: Pad for incontinent subjects Procedure: Wrap around patient's pelvis to collect any material and prevent diagnostic table contamination | |
| Lubricant | Molteni farmaceutici, Località Granatieri Scandicci (Florence) Italy | Description: Luan gel 1% Procedure: Apply on the tip of catheter before insertion | |
| Apron | Mediberg Srl, via Vezze 16/18 Calcinate 24050 (Bergamo) Italy | Description: Kimono Procedure: Put on counteriwise (opening back) to maintain patient's dignity | |
| Gloves | Gardening Srl, Via B. Bosco 15/10 16121 Genova Italy | Description: Nitrile, latex free, no talcum powdered Procedure: Wear during contrast preparation and catheter insertion; change regularly to prevent cross contamination |
References
- DeLancey, J. O. L., Hurd, W. W. Size of the urogenital hiatus in the levator ani muscles in normal women and women with pelvic organ prolapse. Obstetrics & Gynecology. 91 (3), 364-368 (1998).
- Siproudhis, L., Ropert, A., Vilotte, J. How accurate is clinical examination in diagnosing and quantifying pelvirectal disorders? A prospective study in a group of 50 patients complaining of defecatory difficulties. Diseases of the Colon & Rectum. 36 (5), 430-438 (1993).
- Maglinte, D. D. T., Kelvin, F. M., Fitzgerald, K., Hale, D. S., Benson, J. T. Association of compartment defects in pelvic floor dysfunction. American Journal of Roentgenology. 172 (2), 439-444 (1999).
- Dietz, H. P., Jarvis, S. K., Vancaillie, T. G. The assessment of Levator muscle strength: a validation of three ultrasound techniques. International Urogynecology Journal and Pelvic Floor Dysfunction. 13 (3), 156-159 (2002).
- Dietz, H. P., Shek, C., Clarcke, B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Obstetrics & Gynecology. 25 (6), 580-585 (2005).
- Yang, A., Mostwin, J. L., Rosenhein, N. B., Zerhouni, E. A. Pelvic floor descent in women: dynamic evaluation with fast MR imaging and cinematic display. Radiology. 179 (1), 25-33 (1991).
- Lienemann, A., Anthuber, C., Baron, A., Kohz, P., Reiser, M. Dynamic MR colpocystorectography assessing pelvic floor descent. European Radiology. 7 (8), 1309-1317 (1997).
- Healy, J. C., et al. Patterns of prolapse in women with symptoms of pelvic floor weakness: assessment with MR imaging. Radiology. 203 (1), 77-81 (1997).
- Comiter, C. V., Vasavada, S. P., Barbaric, Z. L., Gousse, A. E., Raz, S. Grading pelvic prolapse and pelvic floor relaxation using dynamic magnetic resonance imaging. Urology. 54 (3), 454-457 (1999).
- Kelvin, F. M., Maglinte, D. D. T., Hale, D. S., Benson, J. T. Female pelvic organ prolapse: a comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. American Journal of Roentgenology. 174 (1), 81-88 (2000).
- Pannu, H. K., et al. Dynamic MR imaging of pelvis organ prolapse: spectrum of abnormalities. RadioGraphics. 20 (6), 1567-1582 (2000).
- Hoyte, L., Ratiu, P. Linear measurements in 2-dimen¬sional pelvic floor imaging: the impact of slice tilt angles on measurement reproducibility. American Journal of Obstetrics and Gynecology. 185 (3), 537-544 (2001).
- Tunn, R., DeLancey, J. O. L., Quint, E. E. Visibility of pelvic organ support system structures in magnetic resonance images without an endovaginal coil. American Journal of Obstetrics and Gynecology. 184 (6), 1156-1163 (2001).
- Bump, R. C., et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. American Journal of Obstetrics and Gynecology. 175 (1), 10-17 (1996).
- Haylen, B. T., et al. An inter-national Urogynecological Association (IUGA) / International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Floor Dysfunction. Neurology and Urodynamics. 29 (1), 4-20 (2009).
- Fielding, J. R., et al. MR imaging of pelvic floor continence mechanisms in the supine and sitting positions. American Journal of Roentgenology. 171 (6), 1607-1610 (1998).
- Bertschinger, K. M., et al. Dynamic MR imaging of the pelvic floor performed with patient sitting in an open-magnet unit versus with patient supine in a closed-magnet unit. Radiology. 223 (2), 501-508 (2002).
- Piloni, V., Ambroselli, V., Nestola, M., Piloni, F. Quantification of levator ani (LA) hiatus enlargement and pelvic organs impingement on Valsalva maneuver in parous and nulliparous women with obstructed defecation syndrome (ODS): a biomechanical perspective. Pelviperineology. 35 (1), 25-31 (2016).
- Piloni, V., Pierandrei, G., Pignalosa, F., Galli, G. Fusion imaging by transperineal sonography/magnetic resonance in patients with fecal blockade syndrome. EC Gastroenterology and Digestive System. 5 (1), 11-16 (2018).
- Piloni, V., Bergamasco, M., Melara, G., Garavello, P. The clinical value of magnetic resonance defecography in males with obstructed defecation syndrome. Techniques in Coloproctology. 22 (3), 179-190 (2018).
- Chanda, A., Unnikrishnan, V. U., Roy, S., Ricther, H. E. Computational modeling of the female pelvic support structures and organs to understand the mechanisms of pelvic organ prolapse: a review. Applied Mechanics Reviews. 67 (4), 040801-040814 (2015).
- Rostaminia, G., Abramowitch, S. Finite element modeling in female pelvic floor medicine: a literature review. Current Obstetrics and Gynecology Reports. 4 (2), 125-131 (2015).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved