Aby wyświetlić tę treść, wymagana jest subskrypcja JoVE. Zaloguj się lub rozpocznij bezpłatny okres próbny.
Method Article
Retzius-Sparing Robot-Assisted Radical Prostatectomy
* Wspomniani autorzy wnieśli do projektu równy wkład.
W tym Artykule
Podsumowanie
Robot-assisted Retzius-sparing radical prostatectomy is a technique that enables to preserve urinary continence or facilitates recovery of urinary continence in the majority of patients. Patients must be informed about the risk of a positive surgical margin.
Streszczenie
The technique of Retzius-sparing robot-assisted radical prostatectomy (RS-RARP) and initial experience with it at a single center are provided. The technique is described step-by-step and further illustrated by a video to enhance reproducibility. Early oncological and functional results were evaluated. In total, 77 patients were included with a median follow-up of 11 months (range: 3-21 months). Fifty-one percent of patients had local high-risk or locally advanced prostate cancer. There were no intra-operative complications, and all high-grade complications (2.6%) were related to pelvic lymph node dissection performed concomitant with RS-RARP. Median operation time was 160 min (range: 122-265 min) and median hospital stay was 3 (range: 3-8) days. A positive surgical margin was reported in 42.9%. One-year biochemical recurrence-free survival was 90.1%. After 6 months, all patients were socially continent and after 1 year, 94.3% were fully continent. Of sexually active patients who underwent at least unilateral nerve-sparing, 43.3% were able to have sexual intercourse. This series underlines the surgical safety of performing RS-RARP by a standardized technique and confirms the beneficial effect on the early return of continence. The patient needs to be informed about the risk of a positive surgical margin.
Wprowadzenie
To cure localized and selected cases of locally advanced prostate cancer, radical prostatectomy is one of the recommended treatment options1. Minimal invasive techniques (conventional laparoscopy and robot-assisted laparoscopy) have the advantage to lower blood loss, postoperative pain, and duration of hospitalization as compared to open radical prostatectomy2,3. Among the minimal invasive techniques, robot-assisted surgery combines the advantages of minimal invasive surgery with increased dexterity and freedom of movement of the surgical instruments and with 3-dimensional perioperative vision. In well-resourced countries, robot-assisted radical prostatectomy (RARP) has become the predominant mode to perform radical prostatectomy4.
Urinary incontinence, temporary or definitive, is a common side effect of radical prostatectomy, irrespective of the mode by which it has been performed5. With open (abdominal), laparoscopic, and "standard" anterior RARP (SA-RARP), radical prostatectomy is performed by an anterior approach in which the retropubic (Retzius') space is opened6. Thanks to the increased dexterity associated with RARP, an alternative anatomic approach is possible in which the prostate is resected through the rectovesical pouch or Douglas' pouch as first described by Galfano et al.7. This posterior approach leaves the Retzius' space intact ("Retzius-sparing RARP"; RS-RARP). The main advantage of RS-RARP appears to be a higher and faster recovery of urinary continence8. This study aims to describe in detail (as suggested by the Pasadena consensus panel9) the steps of RS-RARP supported by audiovisual material and to report on the early functional and oncological outcomes of the first cases in a single center.
Protokół
This study has been submitted to the local ethics committee of Ghent University Hospital and institutional approval has been granted (EC UZG 2019/1506). The study has been registered in the Belgian study registry under reference B670201941650. All patients provided written informed consent.
1. Patient preparation and positioning
- Preparation
- Follow contemporary internationally accepted guidelines to diagnose prostate cancer and to set the indication for radical prostatectomy1. Use multiparametric MRI for local staging as this provides important information about prostate volume, concomitant prostatic enlargement and median lobe, and tumor location and extension. This will help in the decision whether to perform nerve-sparing and/or bladder-neck-sparing10. Be sure that this imaging is available at the time of the operation.
- Offer RS-RARP to patients with local or locally advanced prostate cancer and a life-expectancy >10 years. Discuss alternative treatment options such as active surveillance, other modalities of radical prostatectomy, and irradiation whenever applicable. Do not offer RS-RARP to patients with metastatic prostate cancer.
- Rule out medical conditions that are a contra-indication for robotic surgery in steep Trendelenburg position by preoperative anesthesiologic examination. If these medical conditions are present, treat them first (if possible) or discuss alternative treatment with the patient. Include the type and screen of the patient's blood in the preoperative evaluation in the rare case a blood transfusion will be necessary.
- Administer natriumlaurylsulfoacetate-sorbitol-natriumcitratedihydrate clysma 4-8 h before the operation to clean the rectum. Allow food intake and intake of clear fluids until 6 h and 4 h before induction, respectively.
- Perform general anesthesia with endotracheal intubation. Administrate a single-shot prophylactic shot of cefazolin 2g at induction.
- Insert one large-caliber peripheral intravenous line and one arterial line to ensure access and monitoring of the circulatory system. Use pulsoxymetry and 4-lead cardiac monitoring during the entire procedure.
- Positioning
- Place the patient in the supine position. Place and secure the arms along the body of the patient and secure the legs by a strap at the level of the knees. Secure any compression points with gel pads.
NOTE: The patient wears thrombo-embolus deterrent stockings. - Apply shoulder supports to avoid shifting due to the steep Trendelenburg position. Secure the thorax of the patient to the table with adhesive tape (7.5 cm width) to prevent further shifting. Cover the patient with a thoracic warming blanket device.
- Disinfect the surgical field by povidone-iodine alcoholic solution or, alternatively, by chlorhexidine in case of iodine-allergy. Include the anterior abdomen, groins, and genitalia into the surgical field. Attach sterile drapes at the borders of the field after disinfection.
- Place a 16 F hydrogel-coated latex transurethral catheter to ensure urinary drainage and bladder emptying at the time of trocar insertion. Be sure to have easy access to the transurethral catheter as it will aid in the identification of the urethra later during the procedure.
- Place the patient in the supine position. Place and secure the arms along the body of the patient and secure the legs by a strap at the level of the knees. Secure any compression points with gel pads.
2. Docking the robotic system
- Cover the robotic arms of the patient cart with sterile drapes as they will be later in contact with the surgical field. Use a 30° camera.
NOTE: The Da Vinci Xi system is used for this operation (Figure 1). This system consists of three basic parts: a surgeon console that is placed at a distance of the operation table; a patient cart with four robotic arms that will be docked to the trocars and a vision cart with the monitor for scrub nurse and assistant, electrocautery system and CO2-insufflator placed alongside the patient. - Trocar insertion
- Insertion of camera trocar
- Make a skin incision longitudinally over 2-2.5 cm about 1 cm above the umbilicus. Dissect the subcutaneous fatty tissue bluntly until the rectus fascia is identified.
- Incise the rectus fascia longitudinally and place absorbable polyglactin 1 stay sutures at the fascia on both sides.
- Open the peritoneum with scissors. Ensure by digital palpation with the index finger that there is no contact of the bowel to this opening.
- Insert an 8 mm robotic camera trocar with Hasson cone in the peritoneal cavity. Attach the clamps of the cones to the stay sutures at the fascia.
- Attach the camera trocar to the CO2 insufflator and inflate to 12-15 mmHg pressure. Bring the patient in the 30-35° Trendelenburg position to free the minor pelvis from the small bowel. Ensure that there is no shifting of the body during steep Trendelenburg positioning.
- Place at the horizontal level of the camera trocar, two and one 8 mm trocars for the robotic instruments, respectively, at the left and right sides of the camera trocar with 6-8 cm distance between any robotic trocars. Place all trocars under direct vision with the camera. Use the blunt tip obturator to place the trocars.
- Place a 5 mm assistant trocar 5 cm cranially to the midline between the camera trocar and the right robotic trocar. Place a 12 mm assistant trocar 3 cm above the right spina iliaca anterior superior.
NOTE: The assistant is at the patient's right-handed side while the scrub nurse is at the patient's left side. - Disconnect the insufflation cable at the camera trocar and connect to the 12 mm assistant trocar.
- Insertion of camera trocar
- Docking of the patient cart and insertion of robotic instruments
- Move the patient cart to the right-hand side of the patient until the third arm can be connected to the camera trocar. Optimize the positioning of the patient cart further using the automatic application of the system. Connect the three other 8 mm trocars with at least 10 cm distance between the arms to avoid collision during operative movements.
- Use as robotic instruments, a monopolar curved scissor, a fenestrated bipolar forceps, a Cadiere forceps, and a large needle driver. At the start of the operation, place the monopolar scissor in the right robotic trocar, the bipolar fenestrated forceps in the medial left robotic trocar, and the Cadiere forceps in the lateral left robotic trocar.
- Control insertion of robotic instruments by a direct vision to avoid perforation of viscera, omental adhesions, or vascular structures.
- As assistant instruments, use a laparoscopic suction-irrigation device placed in the 5 mm assistant trocar and a laparoscopic grasper placed in the 12 mm assistant trocar. Take place at the surgeon console to start the robot-assisted part of the operation.
NOTE: These laparoscopic instruments are handled by the assistant and are not connected to robotic arms.
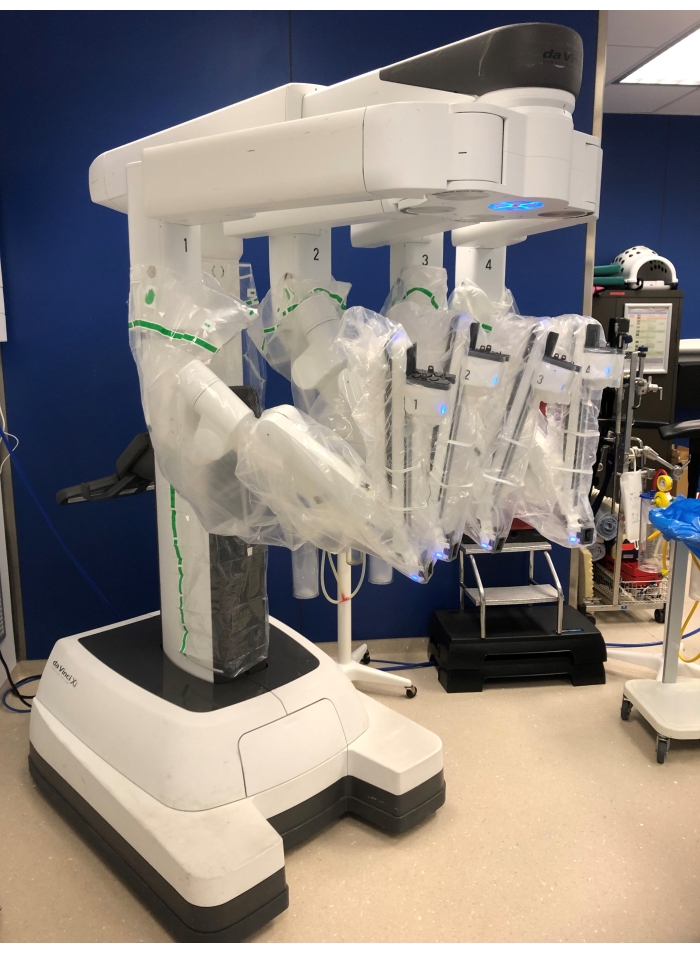
Figure 1: The patient cart with 4 robotic arms. Please click here to view a larger version of this figure.
3. Dissection of the seminal vesicles
- Access to the minor pelvis
- Perform adhesiolysis by releasing any adhesions that hamper easy access to the minor pelvis and rectovesical pouch. Perform this adhesiolysis with the lens turned 30° downward.
- Facilitate access to the rectovesical pouch (or Douglas') by pushing the bladder upward with the Cadiere forceps and by pushing the rectum downward with the suction-irrigation device.
- Access to the seminal vesicles
- Incise the peritoneum over the vas deferens on both sides and continue medially until these incisions reach each other.
NOTE: The vas deferens is most easily identified when it crosses over the external iliac vessels, especially in obese men. - At the lateral edge of the incision, dissect the vas deferens in a circumferential fashion and transect it. Dissect the vas deferens medially until the tip of the seminal vesical is reached.
- Incise the peritoneum over the vas deferens on both sides and continue medially until these incisions reach each other.
- Dissection of the seminal vesicles
- Peel off the Denonvilliers' fascia medially from the vas deferens in case there is no evidence of seminal vesicle invasion. If there is suspicion of seminal vesicle invasion, incise the Denonvilliers' fascia 1-2 mm below the lower edge of the seminal vesicle to ensure a safe surgical margin.
- Secure the vessels where they enter at the tip and lateral surface of the seminal vesicle by bipolar hemostasis or with 5 mm metallic clips and transect them. Continue this dissection until the base of the prostate has been reached. Perform the same procedure on the opposite side.
NOTE: The erectile nerves are close to the tip and lateral surface of the seminal vesicles and monopolar coagulation should be avoided in case nerve-sparing is attempted.
4. Posterolateral dissection of the prostate
- Lateral dissection of the prostate
- Retract the seminal vesicle medially by the Cadiere forceps for the right side and by the assistant laparoscopic grasper for the left side. This allows visualization of the fatty tissue at a triangle between the base of the seminal vesicle and the region lateral to the base of the prostate.
NOTE: This triangle is just above the erectile nerves and prostatic pedicle. - Perform blunt dissection in this fatty tissue along the lateral surface of the prostate until the reflection of the endopelvic fascia is encountered. Perform hemostasis by the bipolar forceps as monopolar current could damage the erectile nerves.
- Retract the seminal vesicle medially by the Cadiere forceps for the right side and by the assistant laparoscopic grasper for the left side. This allows visualization of the fatty tissue at a triangle between the base of the seminal vesicle and the region lateral to the base of the prostate.
- Suspension of the peritoneum
- Facilitate access to the prostate and bladder neck by two suspension sutures through the upper part of the peritoneal incision.
- Insert the large needle driver in the right robotic arm. Place a straight needle with a non-resorbable suture through the abdominal wall 2-3 cm above the pubic bone just medially from the medial umbilical ligament.
- Perforate the upper part of the peritoneal incision and the underlying fatty tissue with the straight needle. Bring the needle back outside the body close to the insertion tract. Keep this suspension stitch under tension using a mosquito clamp outside the abdomen. Do the same on the contralateral side.
- Posterior dissection of the prostate
- Remove the needle driver and bring back the curved scissors in the right robotic arm. Retract the seminal vesicles upward and slightly lateral with the Cadiere forceps and the assistant laparoscopic grasper for the left and right sides, respectively, to bring the Denonvilliers' fascia under tension.
- Handling of erectile nerves.
- Bilateral nerve-sparing approach: Develop a plane by blunt dissection between the prostatic fascia and the Denonvilliers' fascia up to the apex of the prostate and laterally until the prostatic vessels are encountered.
- Non-nerve sparing approach: Incise the Denonvilliers' fascia 1-2 mm below the prostate base. Dissect the anterior surface of the rectum and more laterally in the perirectal fatty tissue.
- Unilateral nerve-sparing approach: Perform step 4.3.2.1 at the site of nerve-sparing and step 4.3.2.2 at the site of non-nerve sparing. Incise the Denonvilliers' fascia at the midline over the rectal wall.
- Hemostasis of the prostatic pedicle and dissection of the neurovascular bundle
- Access to the right side: Grasp the prostate base with the Cadiere forceps just under the attachment of the ipsilateral seminal vesicle. Retract the prostate base medially and slightly upward to bring the prostatic pedicle under tension.
- Make a window with the monopolar scissors in the prostatic pedicle and secure this part of the pedicle using a large polymer locking clip that is applied through the 12 mm assistant trocars. Transect this part of the pedicle at the prostatic side of the clip.
- Repeat 4.4.2 (usually 2-3 times) until the entire prostatic pedicle is secured. Keep tension on the prostatic pedicle after each time a part of the pedicle is transected.
- Repeat step 4.4.2 until the apex of the prostate is reached. Keep a safe distance from the prostatic surface each time a window is made.
NOTE: This will sacrifice the neurovascular bundle containing the erectile nerves. - Peel off the neurovascular bundle from the prostatic fascia by blunt dissection and by keeping the bundle under slight tension using a progressive medial and upward retraction with the Cadiere forceps.
- Secure small vessels attached to the prostate by 5 mm metallic clips and transect them with scissors. Proceed until the apex of the prostate is reached. Ensure suction and irrigation by the assistant through the 5 mm trocar whenever needed.
- Access to the left side: Switch the Cadiere forceps to the medial left-sided trocar and the fenestrated bipolar forceps to the lateral left-sided trocar. Retract the prostate base medially and upward. Use the endowrist of the instrument to create a 90° angle downward under which the assistant has easy access to place the clips. Repeat the procedure at the left side as described above (steps 4.4.2 until 4.4.6).
5. Dissection of the bladder neck
- Grasp the seminal vesicles by the Cadiere forceps and retract them downward to create tension between the bladder neck and the prostate base.
- Develop the plane between the bladder neck and prostate base using a combination of monopolar incisions with the scissors and blunt dissection. Preserve the circular muscle fibers of the bladder neck in case of bladder neck sparing. Move the seminal vesicles more laterally to facilitate the lateral dissection of the bladder neck.
- Opening of the bladder neck
- Incise the mucosa at the posterior aspect of the bladder neck over 1 cm. Visualize the urethral catheter.
- Place an absorbable polyglactin 3-0 suture at the posterior aspect of the bladder neck. Deflate the balloon of the catheter and retract the catheter.
- Grasp the stay suture with the fenestrated bipolar forceps and move upward until the anterior part of the bladder neck becomes visible. Incise the mucosa further and release the bladder neck from the base of the prostate.
- Place a second stay suture at the anterior aspect of the bladder neck with absorbable polyglactin 3-0 suture just before the bladder neck is completely released.
NOTE: These stay sutures will facilitate later identification of the bladder neck for the vesico-urethral anastomosis.
6. Anterior and prostatic apex dissection
- Anterior dissection
- Continue slight upward tension at the stay suture on the posterior aspect of the bladder with the fenestrated bipolar forceps. Place the Cadiere forceps in the prostatic urethra and apply downward traction to create tension at the anterior surface of the prostate.
- Follow the anterior surface of the prostate using a combination of blunt dissection and monopolar incision sparing the Santorini's plexus, the puboprostatic ligaments, and the Retzius' space. Move the Cadiere forceps laterally to facilitate anterolateral dissection.
- Prostatic apex dissection
- Identify the membranous urethra by grasping the urethral catheter with the Cadiere forceps.
- Incise the circular fibers of the urethra 1-2 mm caudally to the apex of the prostate. Push the circular fibers toward the apex of the prostate to expose the inner longitudinal layer of the urethra (the so-called lissosphincter). Transect this inner layer as close to the prostate as possible to maximally preserve the lissosphincter.
- Incise any attachments dorsally to the membranous urethra until the prostate is completely freed from the surrounding tissues. Insert an endobag through the 12 mm assistant trocar to put in the prostate (and seminal vesicles). Close the endobag and leave it closed in the right iliac fossa.
7. Vesico-urethral anastomosis
- Place the large needle driver in the right robotic trocar and the Cadiere forceps and fenestrated bipolar forceps, respectively, in the medial and lateral left robotic trocar. Use the fenestrated bipolar forceps to gently push the bladder toward the urethra in order to reduce tension at the anastomosis.
- Suturing of the vesico-urethral anastomosis
- Place the first suture of the first absorbable barbed wire (3-0, 23 cm in length) outside-in just lateral to the right of the 12 o'clock position on the bladder neck. Pull the anterior stay suture that was placed in step 5.3.4 to identify the bladder neck and the mucosa of the bladder.
- Place the suture inside-out on the urethra, also slightly lateral to the right of the 12 o'clock position. Identify the urethra by moving the tip of the urethral catheter into the membranous urethra.
- Place the first suture of the second absorbable barbed wire (3-0, 23 cm in length) outside-in just lateral to the left of the 12 o'clock position on the bladder neck and inside-out on the urethra at the same position.
- For posterior suturing at the left side, approximate the bladder mucosa against the urethral mucosa by progressive traction on both ends of the barbed wires. Repeat the suturing with the second barbed wire outside-in on the bladder neck and inside-out on the urethra twice at which moment the 9 o'clock position is reached. Approximate the bladder mucosa against the urethral mucosa after each suture.
- For suturing at the right side, perform suturing with the first barbed wire outside-in on the bladder neck and inside-out on the urethra, until the 6 o'clock position is reached. Do not approximate the last suture yet in order to allow space to finalize the left-handed side of the anastomosis.
- For anterior suturing at the left side, continue the anastomosis at the left side going from 9 o'clock to 6 o'clock position. Do not approximate the last suture yet to allow the tip of the catheter to pass between the left and right barbed wires.
- Grasp the tip of the catheter and place it in the bladder. Insufflate the balloon.
- Tighten the last sutures on the left and right sides until the bladder and urethral mucosa are approximated. Check the water-tightness of the anastomosis by instillation of 120 mL of water in the bladder (leak-test).
- Place the first suture of the first absorbable barbed wire (3-0, 23 cm in length) outside-in just lateral to the right of the 12 o'clock position on the bladder neck. Pull the anterior stay suture that was placed in step 5.3.4 to identify the bladder neck and the mucosa of the bladder.
- Remove the suspension sutures at the upper part of the peritoneal incision. Use the remains of the barbed wires to close the peritoneal incision from medial to lateral on both sides. Perform a bilateral pelvic lymph node dissection if indicated by contemporary internationally accepted guidelines1.
NOTE: No surgical drain is left in case pelvic lymph node dissection has not been performed.
8. Extraction of the prostate and closure of the incisions
- Transfer the extraction wire of the endobag from the right robotic trocar to the camera trocar under direct vision.
- Deflate the abdomen and remove the trocars under direct vision. Change the Trendelenburg position to the neutral supine position. Further incise the supra-umbilical skin incision and fascia incision to allow easy extraction of the prostate.
NOTE: The size of this incision depends on the size of the prostate. - Close the rectus fascia with a resorbable polyglactin 1 suture. Close the subcutaneous tissue at the camera trocar and 12 mm assistant trocar with resorbable polyglactin 3-0 suture. Close all skin incisions with skin staplers.
9. Postoperative care
- Transfer the patient to the postoperative care unit and monitor for 2-3 h. Transfer the patient to the hospitalization unit after approval by the anesthesiologist and surgeon.
- Allow the patient to resume intake of clear fluids. Allow intake of solid food and stimulate to walk around during the first postoperative day. Remove the urethral catheter at the third postoperative day and measure micturition volume and residual bladder volume. Replace the catheter in case of substantial residual volume and remove it at the polyclinic 1 week later.
- Discharge the patient on the third postoperative day. Remove the skin staplers between the 10th and 14th postoperative days by the general practitioner. Administrate low molecular weight heparin subcutaneously until the 20th postoperative day by a nurse at home or by the patient himself.
Wyniki
All patients with local or locally advanced prostate cancer with a life expectancy >10 years and with no anesthesiologic contra-indications were offered RS-RARP as one of the treatment options for their disease. Patients undergoing cytoreductive radical prostatectomy for metastatic prostate cancer in the context of a clinical trial or salvage radical prostatectomy were not offered RS-RARP, and patients with anterior tumors were preferably offered SA-RARP. Patients with a follow-up of fewer than 3 months were excluded...
Dyskusje
During RS-RARP, the whole procedure is performed by approaching the bladder through the posterior end. Consequently, the main difference with SA-RARP is the preservation of the Retzius' space. Preservation of Retzius' space has several anatomical advantages7: First, the bladder is not detached from the abdominal wall and the umbilical ligaments are not transected. Therefore, the bladder remains in its anatomical position. Second, the anterior detrusor apron and puboprostatic ligaments are ...
Ujawnienia
The authors have no conflicts of interest.
Podziękowania
No funding was obtained for this research.
Materiały
| Name | Company | Catalog Number | Comments |
| adhesive tape | BSNmedical | 15200028 | Tensoplast |
| assistant trocar 5mm | Aesculap | EKO17R | reusable trocar |
| assistant trocar 12mm | Conmed | iAS12-120LPi | AirSeal trocar |
| barbed wire | Covidien | VLOCM0024 | for vesico-urethral anastomosis |
| Cadiere forceps | Intuitive | 470049 | robotic instrument, grasper |
| camera 30° | Intuitive | 470027 | endoscope |
| cefazolin | Sandoz | BE217296 | Belgian farmaceutical registration |
| CO2-insufflator | Conmed | AS-iFS2 | AirSeal insufflator |
| Da Vinci Xi system | Intuitive | 600062 | robotic system |
| endobag | Covidien | 173050G | Endo Catch 10mm |
| endoscopic hem-o-lok applier | Teleflex | 544995T | to apply the locking clips |
| fenestrated bipolar forceps | Intuitive | 470205 | robotic instrument, bipolar forceps |
| Hasson cone 8mm trocar | Intuitive | 470398 | only at the camera trocar |
| heparin, low molecular weight (enoxaparin) | Sanofi | BE144347 | Belgian farmaceutical registration |
| hydrogel coated latex transurethral catheter | Bard | D226416 | Biocath |
| insufflation cable | Conmed | ASM-EVAC1 | AirSeal Tri-lumen filtered tube set |
| laparoscopic grasper | Aesculap | PO235R | Atraumatic wave grasper, double action |
| large needle driver | Intuitive | 470006 | roboic instrument, needle driver |
| locking clip | Grena | 5-13mm | Click'aVplus |
| metallic clips 5mm | Aesculap | PL453SU | for vessel ligation |
| monopolar curved scissor | Intuitive | 470179 | robotic instrument, hot shears |
| mosquito clamp | Innovia Medical | MQC2025-D | to secure bladder suspension stitch |
| natriumlaurylsulfoacetate-sorbitol-natriumcitratedihydrate clysma | Johnson & Johnson Consumer BV | RVG 05069 | Belgian farmaceutical registration |
| polyglactin 3.0 suture | Ethicon | V442H | stay suture bladder neck, subcutaneous sutures |
| polyglactin 1 suture | Ethicon | D9708 | stay suture fascia and fascia closurie |
| povidone-iodine alcoholic solution | Mylan | BE230736 | Belgian farmaceutical registration |
| robotic trocar 8mm | Intuitive | 470002 | standard length |
| Skin stapler | Covidien | 8886803712 | skin closure |
| sterile drapes robotic arms | Intuitive | 470015 | draping system robotic arms |
| suction-irrigation device | Geyi | GYSL-5X330 | laparoscopic use by assitant |
| suspension sutures | Ethicon | 628H | Ethilon 2-0 nylon suture |
| thrombo-embolus deterrent stockings | Covidien | 7203 | T.E.D. stockings |
| warming blanket device | 3M | 54200 | Bear Hugger |
Odniesienia
- Mottet, N., et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. European Urology. 79 (2), 243-262 (2021).
- Ilic, D., et al. Laparoscopic and robotic-assisted versus open radical prostatectomy for the treatment of localised prostate cancer. The Cochrane Database of Systematic Reviews. 9 (9), (2017).
- Ab del Raheem, A., et al. Retzius-sparing robot-assisted radical prostatectomy versus open retropubic radical prostatectomy: a prospective comparative study with 19-month follow-up. Minerva Urologica e Nefrologica: The Italian Journal of Urology and Nephrology. 72 (5), 586-594 (2020).
- Gandaglia, G., et al. Comparative effectiveness of robot-assisted and open radical prostatectomy in the postdissemination era. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 32 (14), 1419-1426 (2014).
- Ficarra, V., et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. European Urology. 62 (3), 405-417 (2012).
- Martini, A., et al. Contemporary techniques of prostate dissection for robot-assisted prostatectomy. European Urology. 78 (4), 583-591 (2020).
- Galfano, A., et al. A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. European Urology. 58 (3), 457-461 (2010).
- Checcucci, E., et al. Retzius-sparing robot-assisted radical prostatectomy vs the standard approach: a systematic review and analysis of comparative outcomes. BJU International. 125 (1), 8-16 (2020).
- Montorsi, F., et al. Best practices in robot-assisted radical prostatectomy: recommendations of the Pasadena Consensus Panel. European Urology. 62 (3), 368-381 (2012).
- Stabile, A., et al. Multiparametric MRI for prostate cancer diagnosis: current status and future directions. Nature Reviews. Urology. 17 (1), 41-61 (2020).
- Dindo, D., Demartines, N., Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 240 (2), 205-213 (2004).
- Xylinas, E., et al. Evaluation of combined oncological and functional outcomes after radical prostatectomy: trifecta rate of achieving continence, potency and cancer control--a literature review. Urology. 76 (5), 1194-1198 (2010).
- Walz, J., et al. A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. European Urology. 57 (2), 179-192 (2010).
- Walz, J., et al. A critical analysis of the current knowledge of surgical anatomy of the prostate related to optimisation of cancer control and preservation of continence and erection in candidates for radical prostatectomy: An update. European Urology. 70 (2), 301-311 (2016).
- Albisinni, S., et al. Systematic review comparing Anterior vs Retzius-sparing robotic assisted radical prostatectomy: can the approach really make a difference. Minerva Urology and Nephrology. , (2021).
- Menon, M., et al. Functional recovery, oncologic outcomes and postoperative complications after robot-assisted radical prostatectomy: An evidence-based analysis comparing the Retzius sparing and standard approaches. The Journal of Urology. 199 (5), 1210-1217 (2018).
- Olivero, A., et al. Retzius-sparing robotic radical prostatectomy for surgeons in the learning curve: A propensity score-matching analysis. European Urology Focus. 7 (4), 772-778 (2021).
- Galfano, A., et al. Retzius-sparing robot-assisted radical prostatectomy: early learning curve experience in three continents. BJU International. 127 (4), 412-417 (2021).
- Galfano, A., et al. Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of the first 200 patients with >/= 1 year of follow-up. European Urology. 64 (6), 974-980 (2013).
- Hoffman, K. E., et al. Patient-reported outcomes through 5 years for active surveillance, surgery, brachytherapy, or external beam radiation with or without androgen deprivation therapy for localized prostate cancer. JAMA. 323 (2), 149-163 (2020).
- Dalela, D., et al. A pragmatic randomized controlled trial examining the impact of the Retzius-sparing approach on early urinary continence recovery after robot-assisted radical prostatectomy. European Urology. 72 (5), 677-685 (2017).
- Yossepowitch, O., et al. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. European Urology. 65 (2), 303-313 (2014).
- Vale, C. L., et al. Adjuvant or early salvage radiotherapy for the treatment of localised and locally advanced prostate cancer: a prospectively planned systematic review and meta-analysis of aggregate data. Lancet. 396 (10260), 1422-1431 (2020).
- Lumen, N., et al. Safe introduction of robot-assisted radical prostatectomy after a training program in a high-volume robotic centre. Urologia Internationalis. 91 (2), 145-152 (2013).
- Galfano, A., Secco, S., Bocciardi, A. M. Mottrie A. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: An international survey on surgical details and worldwide diffusion. European Urology Focus. 6 (5), 1021-1023 (2020).
- Checcucci, E., et al. Precision prostate cancer surgery: an overview of new technologies and techniques. Minerva Urologica e Nefrologica: The Italian Journal of Urology and Nephrology. 71 (5), 487-501 (2019).
- Grasso, A. A., et al. Posterior musculofascial reconstruction after radical prostatectomy: an updated systematic review and a meta-analysis. BJU International. 118 (1), 20-34 (2016).
- Manfredi, M., et al. Total anatomical reconstruction during robot-assisted radical prostatectomy: focus on urinary continence recovery and related complications after 1000 procedures. BJU international. 124 (3), 477-486 (2019).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone