Method Article
Laparoscopic-Assisted Seldinger Technique for Peritoneal Dialysis Catheter Insertion
In This Article
Summary
Here, we present a protocol for performing the laparoscopic-assisted Seldinger technique (LAST) for peritoneal dialysis (PD) catheter insertion, highlighting a combination of the Seldinger method's minimal invasiveness with the enhanced visualization of laparoscopy.
Abstract
The management of kidney failure has advanced considerably, with peritoneal dialysis (PD) established as a reliable treatment option that uses the peritoneal membrane to remove excess fluid and toxins. PD has shown particular benefits in the initial stages of treatment, potentially leading to better outcomes compared to hemodialysis. Successful PD, however, depends heavily on the correct placement of the PD catheter. This study presents a protocol to perform the laparoscopic-assisted Seldinger technique (LAST) for peritoneal dialysis catheter insertion, highlighting a combination of the Seldinger method's minimal invasiveness with the enhanced visualization of laparoscopy. LAST allows precise catheter placement, making it especially suitable for patients with prior abdominal surgery or those requiring urgent-start PD. This technique enables patients to initiate PD within a day of catheter insertion. The post-surgical protocol involves a gradual increase in dialysate volume, allowing patients to achieve a full PD dose by day five while maintaining controlled peritoneal pressure and minimizing the risk of dialysate leaks. By integrating laparoscopic visualization with the minimally invasive Seldinger technique, LAST has the potential to offer a superior alternative to traditional methods
Introduction
The management of kidney failure has evolved significantly over the past few decades, with peritoneal dialysis (PD) emerging as a well-established treatment modality. PD utilizes the peritoneal membrane as a natural filter to remove excess fluid, correct electrolyte imbalances, and eliminate toxins in patients with kidney failure. PD offers several advantages, including preserving residual kidney function, protecting vascular access, and improving early mortality outcomes1. Additionally, PD provides greater flexibility in treatment schedules and is better tolerated by patients with cardiovascular comorbidities2, making it a preferred option for many. As a result, the global prevalence of PD continues to rise3; however, the success of PD is heavily reliant on the proper placement of the PD catheter, which is critical for ensuring effective dialysis and minimizing complications. Traditional methods of PD catheter insertion, including percutaneous, open surgery, and laparoscopic techniques, have been widely used, but each method presents its own challenges. Both open surgical and percutaneous approaches may not be suitable for patients with a history of previous abdominal surgery due to bowel adhesions. These adhesions, caused by previous surgery-induced inflammation, restrict the free movement of the bowel and increase the risk of needle penetration into hollow organs during PD catheter insertion. In contrast, laparoscopic surgery and the LAST technique provide direct intra-abdominal visualization, which helps avoid needle penetration of adhesed organs and offers a safer alternative for patients with prior abdominal surgery4.
In response to the challenges of PD catheter insertion, we developed a novel approach called the laparoscopic-assisted Seldinger technique (LAST). This hybrid method combines the simplicity and effectiveness of the Seldinger technique, originally developed for vascular access, with the enhanced visualization provided by laparoscopy. The Seldinger method uses a guidewire to facilitate precise catheter placement with minimal tissue disruption5. By integrating laparoscopic assistance, LAST allows for direct visualization of the abdominal cavity, enabling surgeons to navigate anatomical variations and avoid potential complications.
LAST is particularly advantageous for patients with a history of abdominal surgeries, as the visual guidance helps mitigate the risks associated with adhesions and scarring. It is also ideal for patients requiring urgent-start peritoneal dialysis, as the minimally invasive nature of the procedure minimizes tissue trauma, allowing patients to begin PD as early as the day after surgery. This approach enhances the safety and efficiency of PD catheter insertion, making it a preferred option in routine and complex cases.
Protocol
This technique is recommended for patients choosing peritoneal dialysis following shared decision-making. Previous abdominal surgery is not a strict contraindication, as a diagnostic laparoscopic examination can evaluate the abdominal condition before catheter insertion. The protocol was conducted in accordance with the ethical standards set by the institutional human research ethics committee of Taipei Veterans General Hospital.
1. Preoperative preparation
- Administer a routine enema and prophylactic cefazolin (1 g) before surgery.
- Assess the coagulation profile, particularly platelet function closure time, and correct as needed with cryoprecipitate (6-10 units).
- Use a 42 cm straight, double-cuff, Tenckhoff peritoneal dialysis catheter (see Table of Materials).
- Administer cefazolin intravenously as a prophylactic antibiotic.
NOTE: In this protocol, the procedure requires a surgeon, a surgical nurse, and an anesthetist. For most cases, general anesthesia is typically used due to the need for laparoscopic insertion. However, the procedure can also be performed under deep intravenous sedation, depending on the patient's condition and institutional resources.
2. Surgical incision design
- Position the patient supine and disinfect the abdominal area.
- Make two 1 cm incisions (Figure 1).
- Supraumbilical incision: Perform a mini-laparotomy to access the peritoneal cavity, insert a 10 mm trocar for the camera port, and establish a pneumoperitoneum.
NOTE: Both 0° and 30° lenses, 5 mm or 10 mm, rigid or flexible laparoscopes, are feasible. - Catheter insertion incision: Place the incision above the left rectus muscle, 1 cm higher than the deep cuff, positioning the catheter tip at the pubic symphysis.
- Supraumbilical incision: Perform a mini-laparotomy to access the peritoneal cavity, insert a 10 mm trocar for the camera port, and establish a pneumoperitoneum.
3. Catheter insertion technique
- Open the anterior sheath at the catheter insertion site, securing it with two stat sutures for pre-closure (Figure 2A).
- Insert the Tenckhoff catheter using the Seldinger method.
- Puncture the peritoneum obliquely using a 16 G needle under laparoscopic view (Figure 2B). Ensure meticulous hemostasis if rectus muscle bleeding occurs to avoid clotting around the catheter.
- Thread a guidewire into the peritoneal cavity and remove the introducer needle (Figure 2C). Pass a sheath dilator along the guidewire (Figure 2D).
- Insert the Tenckhoff catheter using a straight stylet while peeling the introducer sheath (Figure 2E, F).
NOTE: Refer to Table of Materials for tools used in section 2. - Push the deep cuff into the rectus muscle above the peritoneum (Figure 2G).
- Guide the catheter tip to the pelvic area by the stylet under laparoscopic vision (Figure 2H).
- Close the anterior sheath with pre-placed sutures (Figure 2I).
- Test the catheter function by inflowing PD dialysate and draining it out to ensure proper placement and function while the patient is still on the operating table (Figure 2J).
4. Exit site design
- Design the exit site laterally and lower than the insertion site, creating a subcutaneous pocket to allow the catheter to curve upward (Figure 3A).
- Pull the catheter through the exit site using a skin trocar, ensuring the superficial cuff is at least 2 cm from the exit site (Figure 3B).
NOTE: Avoid placing the exit site near the subcostal region or anterior superior iliac spine to prevent obstruction when sitting. Avoid positioning the exit site too laterally for ease of use. - Close the surgical incisions as per routine practice (Figure 3C).
Results
Surgical results
Implementing the laparoscopic-assisted Seldinger technique (LAST; Supplementary Video 1) for PD catheter insertion resulted in a high success rate, with an overall catheter placement success rate of 99% at the last follow-up. Among a cohort of 200 new PD patients at our hospital, one-sixth had a history of previous abdominal surgery. Of these patients, only one case (0.5%) required reoperation due to omental wrapping 2 days after the surgery, which was successfully addressed in a follow-up procedure. Complications were minimal, with 30-day infectious complications (a composite of exit site infection, peritonitis, and tunnel infection) occurring in 2.9% of patients. The long-term infection rates included an exit site infection rate of 0.6 infections per 100 patient months and a peritonitis rate of 1.4 per 100 patient months. Details of surgical outcomes are summarized in Table 1. In a 3-year follow-up, 18 patients died, and 54 required catheter removal due to tunnel infections, severe peritonitis, or transition to hemodialysis. Among them, 22 had tunnel infections and underwent simultaneous catheter removal and reinsertion, allowing them to continue peritoneal dialysis without interruption.
Post-surgery PD dwell protocol
Patients who undergo the LAST can start peritoneal dialysis the day after catheter insertion. Following the protocol, 500 mL of PD dialysate is administered for 5-6 exchanges on the first day. The volume is then increased to 800 mL on the second day, 1,000 mL on the third, and 1,200 mL on day four. This gradual increase in PD dwell volume helps maintain peritoneal pressure within safe limits and reduces the risk of dialysate leakage. Consequently, patients reach full-dose PD treatment by day five.
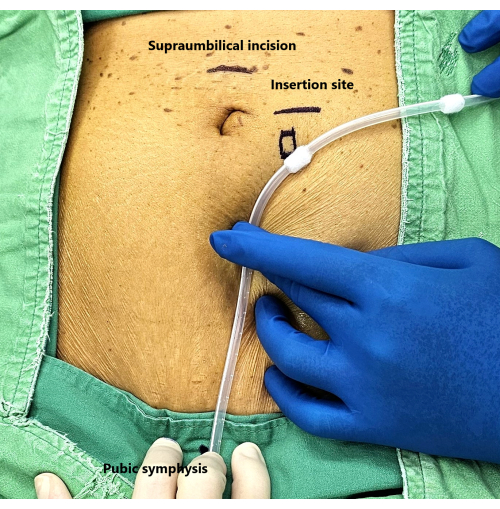
Figure 1: Surgical incision design. Please click here to view a larger version of this figure.
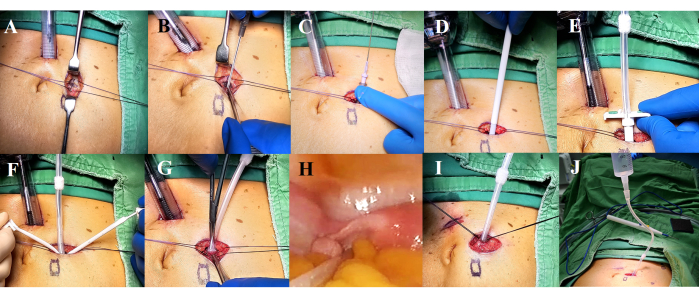
Figure 2: Steps for catheter insertion. (A) Open the anterior sheath and place two sutures for pre-closure. (B-F) Insert the Tenckhoff catheter using the Seldinger method. (G) Position the deep cuff within the rectus muscle layer. (H) Guide the catheter tip with a stylet to the pelvic area under laparoscopic visualization. (I) Close the anterior sheath. (J) Test catheter functionality. Please click here to view a larger version of this figure.
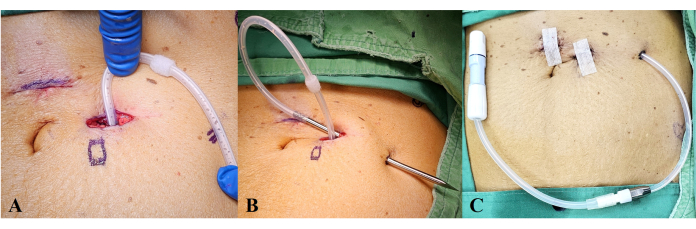
Figure 3: Exit site design. (A) Position the catheter to curve upward, with the exit site designed laterally and lower than the insertion site. (B) Use a skin trocar to pull the catheter through, ensuring the superficial cuff is positioned at least 2 cm from the exit site. (C) Finalize all procedures and confirm catheter placement. Please click here to view a larger version of this figure.
| Complications | n = 208 (%) | |
| Technical complications | Tip migration | 2 (1.0%) |
| Catheter kinking | 0 (0%) | |
| Leakage | 8 (3.8%) | |
| Exit site oozing | 10 (4.8%) | |
| Subcutaneous hematoma | 2 (1.0%) | |
| Early Infectious complication (within 30 days) | Exit site infection | 2 (0.1%) |
| Peritonitis | 6 (2.8%) | |
| Tunnel infection | 0 (0%) | |
| Late complications (occurred 30 days after surgery) | Exit site infection (per 100 patient-month) | 0.6 |
| Peritonitis (per 100 patient-month) | 1.4 | |
| Tunnel infection (per 100 patient-month) | 0.07 | |
| Omental wrapping | 3 (1.4%) | |
Table 1: Surgical outcome of LAST for PD catheter insertion.
Supplementary Video 1: Partial video of LAST. Please click here to download this Video.
Discussion
The introduction of the LAST for PD catheter insertion represents a significant advancement in managing patients with kidney failure. This hybrid approach combines laparoscopic visualization with the minimally invasive Seldinger technique, offering an attractive alternative to traditional catheter placement methods6.
In the context of PD catheter insertion, the percutaneous Seldinger technique allows patients to begin treatment within 24 h without an increased risk of dialysate leak. However, its main drawback is the lack of visual monitoring, making it unsuitable for patients with previous abdominal surgery or adhesions7,8,9. In contrast, laparoscopic insertion is preferred due to the full visualization of the peritoneal cavity, allowing for safer and more accurate catheter placement. Although laparoscopic insertion requires a two-week waiting period before starting treatment, it has gained widespread acceptance for its favorable outcomes10,11,12. The LAST method combines the advantages of both techniques. Patients who undergo LAST can initiate PD the day after surgery; this rapid initiation is particularly crucial for patients requiring urgent-start PD13.
Additionally, LAST is associated with a lower incidence of surgical complications, such as exit site infections and peritonitis, than the traditional laparoscopic method6. The reduced complication rates are attributed to the minimal tissue trauma associated with the Seldinger technique, preserving the integrity of the peritoneal membrane and surrounding structures. LAST also offers significant cost-effectiveness and resource utilization benefits. By reducing hospitalization length and overall medical expenses, LAST alleviates the financial burden on healthcare systems6.
The LAST represents an innovative approach to PD catheter insertion that utilizes basic laparoscopy, making it an attractive option for healthcare facilities. One of the key advantages of LAST is that it does not require hospitals to invest in expensive, specialized equipment, such as Y-TEC peritoneoscope14. In contrast, LAST can be implemented using readily available laparoscopic instruments, allowing hospitals to provide quality care without incurring excessive costs. This affordability makes LAST a feasible option for a wide range of healthcare settings, from large academic medical centers to smaller hospitals. Furthermore, the learning curve associated with LAST is relatively short. The technique incorporates fundamental laparoscopic principles, enabling surgeons to quickly gain proficiency without extensive additional training. With a focus on simplicity and effectiveness, LAST empowers surgeons to perform catheter insertions with enhanced safety and accuracy. The combination of cost-effectiveness and ease of learning ensures that LAST can be widely adopted, ultimately improving patient outcomes. By minimizing the time between catheter insertion and the start of dialysis, LAST allows for a smoother transition for patients, particularly those needing urgent care. Additionally, this technique can be especially beneficial for patients who require the removal of an old catheter due to a tunnel infection, as it allows for the simultaneous insertion of a new PD catheter on the opposite side of the abdomen.
Despite its advantages, LAST does have limitations, primarily related to the availability of laparoscopic equipment and the peeling sheath required for the procedure. These factors may hinder widespread adoption in some healthcare settings, highlighting the need for access to the necessary tools and trained personnel. In addition, since the procedure uses only a single camera without accessory ports or forceps, the ability to exteriorize the omentum and perform an omentectomy is limited. As a result, omentectomy is not routinely performed in LAST.
In conclusion, LAST is a significant advancement in PD catheter insertion for kidney failure patients. By integrating laparoscopic visualization with the minimally invasive Seldinger technique, LAST has the potential to offer a superior alternative to traditional methods.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by Taiwan National Science and Technology Council grant 113-2314-B-075 -075 -MY3 and by the Y.L. Lin Huang Tai Education Foundation.
Materials
| Name | Company | Catalog Number | Comments |
| Argyle Tenckhoff Peritoneal Catheter | Covidien | 8810888003 | Straight, 42 cm, 2 Cuffs |
| Introcan Safety Deep Access | B. Braun | N/A | Size: 16 G |
| Pull Apart Introducer Set for Inserting Catheters abd Pacing Leads | Covidien | 8815544010 | Size: 16Fr |
References
- Marron, B., Remon, C., Perez-Fontan, M., Quiros, P., Ortiz, A. Benefits of preserving residual renal function in peritoneal dialysis. Kidney Int Suppl. 108, S42-S51 (2008).
- Teitelbaum, I. Peritoneal dialysis. N Engl J Med. 385 (19), 1786-1795 (2021).
- Auguste, B. L., Bargman, J. M. Peritoneal dialysis prescription and adequacy in clinical practice: Core curriculum 2023. Am J Kidney Dis. 81 (1), 100-109 (2023).
- Briggs, V. R., et al. Catheter insertion techniques for improving catheter function and clinical outcomes in peritoneal dialysis patients. Cochrane Database Syst Rev. 2 (2), CD012478 (2023).
- Hafiani, H., Charif Saibari, R., Morsad, N., Rami, A. Sven Ivar Seldinger (1921-1998): The founding father of interventional radiology. Cureus. 16 (5), e60397 (2024).
- Li, S. Y., et al. Hybrid method for peritoneal dialysis catheter insertion: A new technique for improved outcomes and reduced costs. Am J Nephrol. 54 (7-8), 349-358 (2023).
- Kim, J. H., et al. Percutaneous peritoneal dialysis catheter implantation with no break-in period: A viable option for patients requiring unplanned urgent-start peritoneal dialysis. Kidney Res Clin Pract. 39 (3), 365-372 (2020).
- Xie, D., et al. Percutaneous insertion of peritoneal dialysis catheter is a safe and effective technique irrespective of BMI. BMC Nephrol. 21 (1), 199 (2020).
- Jo, Y. I., Shin, S. K., Lee, J. H., Song, J. O., Park, J. H. Immediate initiation of CAPD following percutaneous catheter placement without break-in procedure. Perit Dial Int. 27 (2), 179-183 (2007).
- Haggerty, S., et al. Guidelines for laparoscopic peritoneal dialysis access surgery. Surg Endosc. 28 (11), 3016-3045 (2014).
- Sun, M. L., et al. Randomized controlled trials for comparison of laparoscopic versus conventional open catheter placement in peritoneal dialysis patients: a meta-analysis. BMC Nephrol. 21 (1), 60 (2020).
- Hagen, S. M., Lafranca, J. A., Steyerberg, E. W., IJzermans, J. N. M., Dor, F. J. M. F. Laparoscopic versus open peritoneal dialysis catheter insertion: a meta-analysis. PLoS One. 8 (2), e56351 (2013).
- Rajora, N., Shastri, S., Pirwani, G., Saxena, R. How To build a successful urgent-start peritoneal dialysis program. Kidney360. 1 (10), 1165-1177 (2020).
- Al Azzi, Y., Zeldis, E., Nadkarni, G. N., Schanzer, H., Uribarri, J. Outcomes of dialysis catheters placed by the Y-TEC peritoneoscopic technique: a single-center surgical experience. Clin Kidney J. 9 (1), 158-161 (2016).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved